Research Article - (2025) Volume 15, Issue 1
Background: Despite health being a fundamental human right, health inequality continues to be a challenge to many societies and is a threat to sustainable development. One major contributing factor is lack of human resource for health especially in rural and remote areas. One of the interventions to reduce this burden is medical education training that includes innovations that take the health worker closer to the environment and community he/she is likely to serve. In order ring this to a reality, Busitema University Faculty of Health Sciences (BUFHS) undergraduate courses were designed with a strong Community-Based Education, Research and Services (COBERS) program since its inception in 2013. Included along were Inter-Professional Education (IPE) approach and research education. IPE as a new innovation in the COBERS, was innovated with a target to create different professionals of health workers that will appreciate learning and working together rather than run in silos to solve community needs. This communication is aimed at providing a platform from which health training institutions can learn from our experience and the successes and probably challenges of COBERS.
Materials and methods: We implemented COBERS with IPE in our curriculum for the undergraduate students of nursing and medicine during their community attachment. Students under the different programmes were randomly chosen to go to the COBERS sites for their community training and cross-cutting courses were designed to be undertaken during that period. The same groups of students are maintained, and same facility and preceptors and mentors are maintained for the duration of the training. They were assigned a preceptor at the site and a supervisor at the faculty. Follow up of of the successful implementation of the programme was done on a daily basis by the trainers led by the preceptor and an interim assessment is done by the supervisor. At the end of the placement students write a report that is marked together with their log books.
Results: COBERS program significantly has improved year over year. In addition to the value of the community experiences to the students, tangible program outcomes have been recorded. Some of the program outcomes include capacity building in research skills for faculty mentors, research skills introduced in undergraduate training, a strong research mentorship program, health promotion in the communities, and a strong relationship between the university and the community training sites.
Conclusion: The program did not only allow the university to rethink traditional learning strategies and programs but also improved the skills of the academic staff and preceptors.
Community Based Education and Research Services (COBERS) • Inter-professional education • Community-involvement • Community entry • Community diagnosis • Busitema University
BU: Busitema University; COBERS: Community Based Education and Research Services; BUFHS: Busitema University Faculty of Health Sciences; GOU: Government of Uganda; HEPI: Health Professional Education Partnership Initiative; IPE: Inter Professional Education; PHC: Primary Health Care; NDPIII: Third National Development Plan; RHITES: E-Regional Health Integration to Enhance Services-EAST; SWOT: Strength Weaknesses Opportunities and Threats
Health is a fundamental right of human beings and thus recognising it as one obliges states and governments to ensure access to timely, acceptable and affordable health care. Despite being one, disparities exist across the world between the rural and the more affluent areas and across different geographical planes [1,2]. the reason the need for equity has been echoed within the Sustainable Development Goals (SDGs) [3]. These inequalities are also evident in Uganda [4,5].
To bridge this gap, there must be concerted and targeted efforts that resonate with the gravity of the problem and this may include changing the training needs and trends of health workforce. Busitema University, Faculty of Health Sciences (BUFHS) opened as the fourth public medical school in Uganda, after Makerere University College of Health Sciences, Mbarara University of Science and Technology, and Gulu University. BUFHS promotes a rich culture of service-learning, a commitment that extends to every faculty in the university. Internationally, the focus of education in medical schools has shifted from traditional hospital-based training to learning in the community [6].
The development of community-based medical education has been driven by the desire to train doctors and nurses where they will base their future practice a practice that occurs increasingly within communities. This is in contrast with the more traditional method of teaching students from large urban hospitals. Underlying this change is the idea that medical practice is place-dependent, and that learning in one location does not necessarily equip the student to practice somewhere else [7]. The training of health workers who can, and who want to, practice in rural communities is best done experientially in rural settings and calls for a multifaceted approach [8-10].
Informed by the wider place-based education movement, it is this idea that led to the development of the community based education research and service program at faculty of health sciences, Busitema University. The difference between BUFHS COBERS programmes and that of other universities in the country is the component of research while at the site of community placement. Thus Community-Based Education and Service (COBES) is upgraded to COBERS. We hinged our upgrade on the positive impact COBES had had at Makerere University, college of health sciences as described in a study by Mwanika, et al. [11,12].
The university’s commitment to the Community-Based Education Research and Service (COBERS) program was built on several basic values that continue today: The fundamental dignity of all; poverty and lack of opportunity breed problems; and to understand community problems, one must live in and embrace the community. These values are very evident in BUFHS’s educational, research and service program.
The BUFHS’s mission statement is “To promote innovations in teaching, learning, and research for enhanced access to quality health care”.
To carry out this mission, four of the BUFHS six institutional goals are related to community service-learning programs:
• To increase the number of high-quality health professionals in the country.
• To produce graduates with high morale and motivation to work in rural (including hard-to-reach) areas as their training will be based in such communities.
• To strengthen the district hospitals and health centres through a strong community training and research program.
• To maintain a leadership role in forming health care policy at the university, district, and national levels.
Related to its mission and goals, BUFHS has a set of competency statements, many of which are related to community programs: “A graduate of the medicine and nursing programs at BUFHS will be competent to:
• Apply the fundamental principles of the behavioural sciences as they relate to patient-centred approaches for promoting, improving, and maintaining health
• Employ the interpersonal and communication skills necessary to provide health care to a diverse patient population and to function in a multicultural work environment
• Evaluate various models of health care management and delivery.
• Apply the principles of ethical reasoning and professional responsibility as they relate to patient care and practice management.
COBERS was designed to connect classroom-based learning with meaningful community involvement by preparing students to be participating members of a community through health care delivery and wellness promotion which, in turn, advances sustainable socio economic development. Rural communities struggle to retain doctors and this contributes to health inequities characterized by higher rates of disease morbidity and mortality. Increasing access to health care services in rural communities remains a key priority of BUFHS and is clearly in line with attainment of SDGs specifically 3 and 5 and Government of Uganda (GOU) Third National Development Plan (NDPIII) strategic plan [13].
We describe the elements of the community based education research and service program, introduction of inter-profession education therein at BUFHS and the environment that has helped it become successful. This report validates OBERS from 2013 to 2019.
The study site
These sites included Moroto regional referral hospital, Katakwi general hospital, Amuria Health Centre IV (HCIV) currently upgraded to a level of a general hospital, Serere HCIV, Ngora HCIV, Bukedea HCIV, Busiu HCIV, Busolwe hospital, Kibuku HCIV, Busia HCIV, Masafu hospital, Kidera HCIV, Bugono HCIV, Bududa hospital, Bugobero HCIV, Muyembe HCIV, Kapchorwa general hospital, Kaproron HCIV, and Bukwo general hospital (Figure 1).
The Uganda health sector is organized in a bottom-up approach with the village health teams at each village level, that feed into and are provided with technical support by the health centre II, the latter feeding into health centre III and health centre into health centre IV, to the general hospital and then to the regional referral hospital and finally to the national referral hospitals. At each level of health care, there is a different level of the target population and the nature of services provided and thus the different skills and technical knowledge and mix of health workers. Description of the health care system in Uganda has been earlier explained by Wanial, et al. [14].
Each COBERS site had to sign a Memorandum of Understanding (MOU) with BUFHS. The MOU covers aspects of areas of collaboration (teaching, patient care, and research), data and intellectual property rights, ethical considerations, evaluation of the MOU, review, and amendments of the MOU. The criteria used for choosing the COBERS sites included; availability of health facility that serves as student base and link to the community, availability of a medical doctor and or graduate nurse) to serve as a preceptor for the student’s community program and a variety of community disease case burdens for students to learn from. Conversely, highly specialized health facilities were deliberately excluded since the curriculum was designed for general exposure to communities with disease case mix. Health units with a catchment population of above 2,000 people within a distance of 5 Km radius to communities and preferably not linked to other universities in the country for implementation of COBERS activity were chosen.
In 2013 a total of 10 sites met the criteria and were used for COBERS placement. In 2014 two of the ten sites were dropped because of the absence of medical officers to work as preceptors. In 2015, with the increase in the number of students, there was a need to increase the number of COBERS sites.
Therefore, between 2015 and 2016 the committee assessed more sites and this took the number to 17 sites. With three groups of students for community placement, namely students in the year I, II, and III, the 17 sites were not adequate hence the number of sites is rose to the current nineteen. Below is a map showing the COBERS sites (Figure 1).
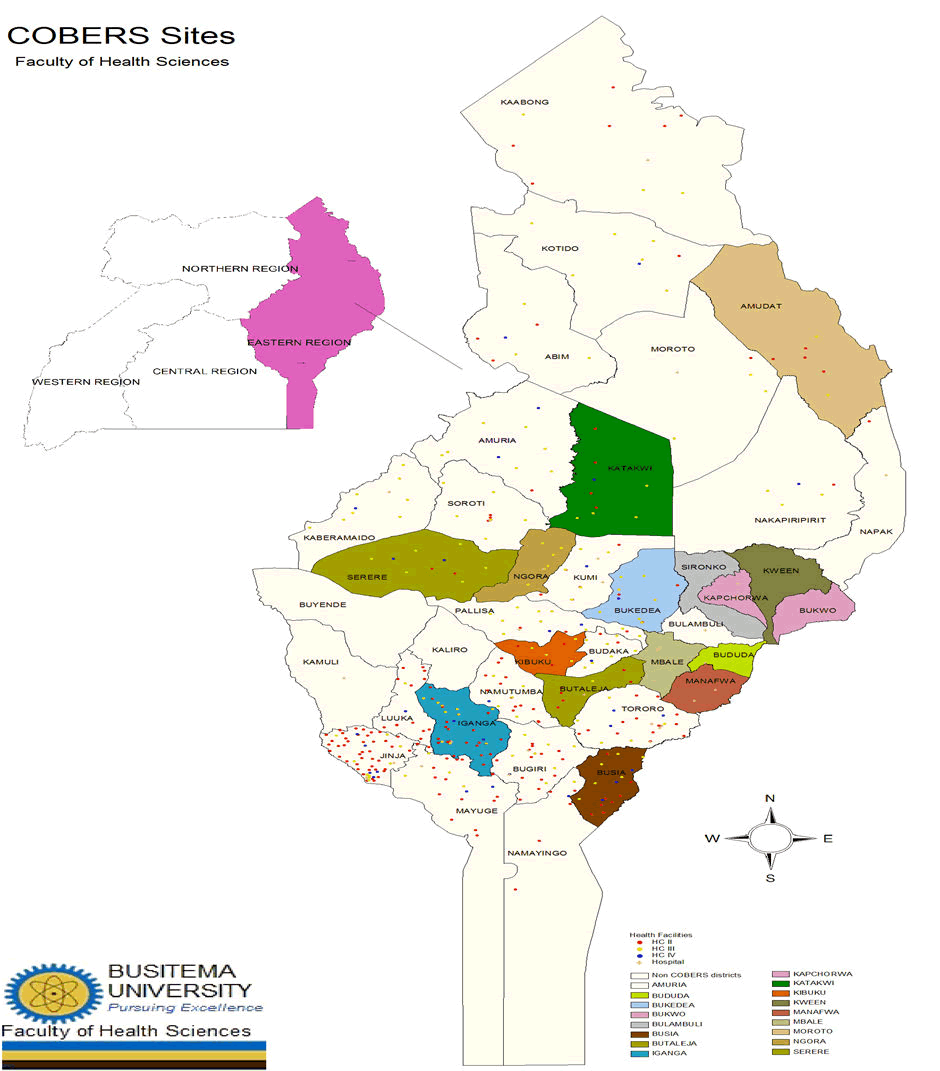
Figure 1. Map showing the 19 COBERS sites.
Value
The COBERS program adds value in ways that go beyond caring for the underserved. First, the program takes students to where patients live, providing first-hand experience with social barriers to care (such as transportation, values, culture, and economics). Second, students gain valuable practice management experience in those settings.
Moreover, practicing in community health facilities provides students with an opportunity to work consistently with a preceptor/ mentor. Furthermore, students gain insight into the policies and politics of health facilities and Districts. Additionally, they observe the management of many more patients in the health facilities than would be the case in the school-based hospital and gain skills and confidence that come with more clinical experience. Finally, students help to reduce access disparities by assisting in the provision of care to more patients in the community health facilities.
Notwithstanding, the involvement of students into the research component of training helps then have insight into the real health challenges of the communities and the country at large.
Quality assurance in the program
Every health facility that hosts students has a qualified medical doctor and or graduate nurse called a preceptor, who supervises students during their training in the community. The doctor works closely with a nursing officer at the facility. This is emphasized because of the mix of the students at the sites and the need for them to appreciate inter-professionalism. Interprofessional education is integrated in a piece meal during the three years of the placement. It is emphasised that the same students go to same facility throughout their COBERS training.
The faculty holds training and orientation meetings with preceptors annually to equip them with teaching and learning methods. The faculty also arranges for supervision visits during the community placement. These visits provide an opportunity for faculty staff to interact and support the preceptors during a community placement. The preceptors also participate in assessing students in knowledge, attitude, and skills and give feedback to the faculty. In-house surveys have revealed consistent students’ enthusiasm and support of the community attachments and their understanding of underserved patients, communities, and the healthcare delivery system.
Elements of the COBERS program
The COBERS program aims to develop health professional students who are responsive to the needs of local communities and who will become socially accountable and transformative agents of change in the struggling Ugandan healthcare system.
The COBERS program comprises three, 4-week modules in the first, second, and third academic years of the undergraduate medical and nursing curricula. Successful completion of these modules is a prerequisite for graduating from the medical and nursing programs. Clear learning outcomes are prescribed in the curriculum that includes the research process and incorporates scholarship competencies. The 4 weeks are scheduled to follow the recess term. Students are randomly grouped by an independent member into groups of 4 to 6 and randomly assigned to the different sites, ensuring a mix of medical and nursing students to promote inter professional learning, a mix of direct entrants, and diploma-qualified health workers to promote hand-on training at the sites.
Organization and the curriculum: Before COBERS placement, students are taken through an intense one-week program of first aid and nursing skills as a way of preparing them for the community clinical/nursing work. This is done through lectures and practical skills in taking vitals that are key to patient’s monitoring.
In the first COBERS module, the students are introduced to basic principles of epidemiology, biostatistics, and demography. The students are tasked to explore communities and understand their structures, including identifying the gatekeepers who must be engaged before accessing the rest of the community. They make a community diagnosis and identify the top five key gaps in their community placement. They are tasked to use a prioritization matrix and chose one of the gaps that they would research. From this, they formulate a relevant Primary Health Care (PHC) research question. Each group then prepares a referenced literature review around the selected research topic and they also prepare a report.
During the second COBERS module in the 2nd academic year, each group is assigned a research mentor who is a member of the faculty. Each group prepares a research protocol informed by structured lectures and mentorship on basic research methods. The students are given chance to present their proposals to staff in the unit, they are given comments and time to improve the proposals. The research protocols are presented to the institutional higher degrees and ethics review board for approval. With informed consent, the students collect data in the COBERS sites and communities. With support from the research mentors, the students analyze the data, write reports, and present scientific research posters to peers and examiners. The students are further encouraged to write manuscripts and publish with the support of the mentors and the faculty.
In the third COBERS module in the third year, health promotion projects informed by the research findings during year II research are implemented hence closing the research cycle. The students also learn primary health care, health systems management and are introduced to clinical clerkship and the nursing process.
The community-based medical education research and service program at BUFHS is not housed in a particular department. It is headed by a coordinator appointed by the Dean and supported by the committee appointed by the faculty board (Figure 2).
Figure 2. The COBERS cycle at Busitema University faculty of health sciences.
Resources for the COBERS program: The COBERS program is quite resource-intensive but the program objectives and thus outcomes continue to indicate that it is a worthwhile investment. Collaboration with several stakeholders helped ease the resource pressure. The program’s success relies much on the commitment of the faculty and the preceptors rather than monetary investments. Funding for this program comes from the university budget. During the routine budgeting process, activities for community placement are routinely included. Funding majorly goes to accommodation facilities, transport for the students to and from the sites, facilitation, and travel for the site supervisors and preceptors’ allowances. The students are also provided with gas stoves for cooking and stationery for learning activities. Furthermore, efforts have been taken by the faculty to equip each site (save for very few) with a desktop loaded with e-books and other materials to aid students learning and research.
Program outcomes: Student support for the COBERS program remains strong. The community experiences are valued by students who enjoy the relatively supervised clinical ‘independence’ while in the community sites. The students have gained skills in problem identification, proposal writing, research methods, and scientific writing. Several papers have been published from the COBERS program.
Through the health promotion projects, there has been increased awareness about health issues and general improvement in the quality of health care. The University management continues to offer strong support for the program as evidenced in the budgetary allocation and believes that it is fundamental for a first-class education.
The faculty have continued to support the program through the research mentorship and supervision provided to the learners. This has helped improve scientific writing skills of both the faculty and learners. This initiative helps break the barriers of research training the ‘Four I’s’ (lack of initiative, impulse, incentive and idols). The impact of research inclusion in the COBERS programme has been reported by Delport, et al.[15]. Subsequently, several publications have been churned out with the students. In turn, these publications have increased the scientific knowledge base and raised Busitema University visibility.
As a university, we have been able to reach out to the community through the COBERS program, and through dialogue with the community members, we have been able to identify gaps that need to be addressed (Table 1).
Strength, Weaknesses, Opportunities and Threats (SWOT) analysis for the COBERS program
| Strengths | Weaknesses |
|
|
| Opportunities | Threats |
|
|
Table 1. SWOT analysis for the COBERS program.
BUFHS COBERS program as a training model is worthwhile.
Despite needing resources for implementation, it is a model that we would recommend for health sciences faculty as it may help bridgethe gap between remote and rural health inequalities. Furthermore, it may help build capacity in research skills for the faculty, preceptors and students.
Suggested area of research
How universities harness community resources to substantially contribute resources for this community can based training? These resources may include but are not limited to identifying retired civil servants and other community persons who could offer accommodation to students at no fee as long as the university could meet minimum maintenance costs.
Strength of this narrative
Authors walk the journey through the programme from its inception and document its invaluable achievements but not forgetting the challenges. This could help inspire other health training institutions planning to have COBERS in their models.
Whereas Busitema University mobilizes resources to run the program, no funding was provided for documenting and publishing this manuscript.
The written ethical approval was considered not applicable for this manuscript by the Busitema University, faculty of health science since it is a documentation of the successes and challenges in the implementation of a community based program.
Also, no participants were recruited to contribute to the information presented in this manuscript, therefore, consent to participate was not applicable.
RN coordinated the COBERS program and conventionalized the documentation of the evolution and success of the program, PO, JN, YG, LS, IJS reviewed the document and also mentored students in the program, JML, JW, P W supervised and mobilized resources for the program. All authors read and approved the final version to be published.
We declare no conflict of interest
All data on which conclusions of this manuscript are drawn has been included in this manuscript and whatever may be missing is available on request from the corresponding author.
We are grateful to the district administration; the chief administrative officers, the district medical officers, the resident district commissioners and our Preceptors in the different districts and sites who have continued to immensely contribute to the COBERS program. MEPI/MESAU played a very key role in funding student’s activities from the inception of the program and HEPI project (Fogarty international centre of the national institutes of health, U.S. department of state’s office of the U.S. Global AIDS coordinator and health diplomacy (S/GAC), and President’s Emergency Plan for AIDS Relief (PEPFAR) under Award Number 1R25TW011213. The content is solely the responsibility of the authors and does not necessarily represent the official views of the national institutes of health.”) was very instrumental in funding the students’ research projects. The top administration of Busitema University has always supported the evolution and success of the program from its inception.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Nekaka R, et al. "The Successful Implementation of Community Based Education and Research Services Programme at a Rural Health Sciences Faculty in Uganda: Case of Busitema University". Primary Health Care: Open Access, 2025, 15(1), 1-5.
Received: 12-Jan-2024, Manuscript No. JPHC-24-125030; Editor assigned: 15-Jan-2024, Pre QC No. JPHC-24-125030 (PQ); Reviewed: 29-Jan-2024, QC No. JPHC-24-125030; Revised: 19-Mar-2025, Manuscript No. JPHC-24-125030 (R); Published: 26-Mar-2025, DOI: 10.35248/2471-8556.25.15(1).496
Copyright: © 2025 Nekaka R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.