Research Article - (2025) Volume 15, Issue 1
Introduction: Adolescence is a period of transition from childhood to adulthood that involves physiological, anatomical, and psychological and biochemical changes that influence natural experimentation, abstract thought, contemplating the future, empathy, and idealism. Therefore, parental investments in adolescents may be reflected in adulthood outcomes. Uganda has poor adolescent health indices such as national teenage prevalence rate of 25% and adolescent human immune virus rates between 11-18%. These threaten the national development plan III and sustainable development goals 1,3,4,5, and 8. We therefore aimed to study the influence of parent/parent-figure teenage communication and its influence on contraceptive use in Uganda.
Materials and methods: A community based cross sectional descriptive study with mixed methods was used. We used researcher administered structured questionnaires to collect quantitative data and analysed it using STARTA 4 while focus group discussions were used for qualitative data collection and analysed using NVIVO. We premised this study on theory of elaborate likelihood model and theory of planned behaviour and reinforced by constructive parental behaviour.
Results: 387 adolescents were enrolled of whom 50.4% were females and 49.6% males. 85.5% were rural dwellers, 97.1% had formal education, 72.1% were single, 84.2% were Christians and 27.9% married. About 47.8% had dropped out of school and only 7% were employed. Additionally, 63.8% were from nuclear family while 5.9% were from single parent families. Significantly 66.14% had had sex in the past 1 year and 73.7% used a contraceptive. Whereas 99.2% had heard about contraceptives, only 28.1% did so from a parent/parent-figure and other source. Contraceptive use was significantly associated with parent/parent-figure-teenage communication (AOR=6.95% CI 1.3-34.5, p=0.023).
Conclusions: Contraceptive use was reinforced by teenage-parent/ parent-figure communication. Parent/parent figures may be important in unlocking the misconceptions and fallacies about adolescent sexuality and ease access to adolescent sexual and reproductive health services.
Adolescent • Contraceptive use • Parent/parent-figure teenage communication • Uganda
Adolescence is a period of transition from childhood to adulthood rather than an extended childhood period. It is described as a critical stage in one’s development full of not only opportunities but also risks. It is therefore a period of natural experimentation, abstract thought, contemplating the future, empathy, and idealism yet characterized by immature decision making. Moreover, whereas adolescence is characterised by abstract thinking and contemplating the future, for empathy and idealism, these attributes are largely shaped by the environment in which these adolescents live. There are about 1.3 billion adolescents in the world and make up about 16% of the world’s population and 85% are resident in the developing countries. In Uganda the population of adolescents is 25%. Given the fact that what happens or does not happens during adolescence has lifetime implications, the investments in adolescence are timely individual and public health investments [1].
Every year approximately 21 milliion of 15-19 year olds get pregnant in the developing countries. Data related to the 10-14 year olds is scare. Despite Adolescent Birth Rate (ABR) declining, it is still unacceptably high in Africa and the Latin America countries at 100 and 53.2 birth per 1000 women respectively. The number of actual birth to adolescents is still very high especially in SSA with estimates putting it at 611400 as of 2021.
Overall Teenage Pregnancy (TP) in Africa is high and higher in the east African sub region. In a meta-analysis by Wado, et al. 19.3% TP was noted in Sub-Saharan African (SSA). Adolescent pregnancy and early motherhood is common in the five east African countries, ranging from 18% among adolescents in Kenya to 29% in Malawi and Zambia. It is associated with increased odds of maternal and perinatal adverse outcomes. For example, in Sub Saharan Africa and Asia, mortality rates of children born to mothers aged <16 years, 16-17 years and 18-19 years at first birth were about 2-4 times, 1.5-2 times and 1.2-1.5 times higher, respectively, then among firstborn children of mothers aged 23-25 Other studies have reaffirmed the above findings [2]. A more recent analysis of data of 38 countries estimated that the risk of death while giving birth for adolescents 15-19 years is 28% higher than that of women aged 20-24 years. Furthermore, neonatal mortality is inversely proportional to the maternal age.
Additionally, WHO estimates that about a half of all human immune virus infections occur in people below or equal to 25 years. Every year, an estimated 1.7 million youths lose their lives prematurely due to preventable accidents and pregnancy related complications. Literature also shows gender disparities with the more females affected than the male s irrespective of the background [3].
Moreover, despite efforts to reduce global maternal and perinatal mortality and morbidity, it has remained high and inevitably threatens attainment of sustainable development goals 1,3,4,5 and 8. From 2000 to 2017, the global Maternal Mortality Ratio (MMR) declined by 38% from 342 deaths to 211 deaths per 100.000 live birth. Furthermore, developing countries continued to account for 99% of the deaths, Sub-Saharan Africa (SSA) and Asia alone accounting for 87% of the deaths [4]. It is therefore a clear manifestation that to achieve sustainable development goals 1,3,4,5 and 8, adolescents’ health needs, need a focussed investment. This is so because the adolescent population continues to face the wrath of the detrimental effects of child birth.
Uganda’s MMR stands at 336 deaths per 100,000 live birth. Maternal deaths represented 18% of all deaths among women reproductive age group (15-49) during the 7-year period preceding the 2016 with adolescents (15-19 years) contributing 17% of all pregnancy related mortality rate in Uganda. Noteworthy is the fact that the adolescent mortality ratio of 18 per 1000 children aged 15 is on a higher end of the spectrum. Additionally, HIV mortality associated rates stand between 11-17% for the adolescents. These poor life indicators do not only threaten Uganda’s third National Development Plan III (NDPIII) 2020/21-2024/25 vision, goal and theme (NDPIII) but also the internationally launched Sustainable Development Goals (SDGs).
One of the renowned direct interventions geared at reducing MMR, HIV infections and indirectly perinatal mortality is contraception. As reported by Ahmed, et al. 272,000 maternal deaths are averted worldwide each year due to contraceptive use and Family Planning (FP) and contraceptive uptake averted over 1 million maternal deaths between 1990-2005 due to a decline in Total Fertility Rate (TFR). Furthermore, by reducing high-risk births, family planning reduced more MMR indirectly. No wonder data shows that the rate of contraceptive use is inversely proportional to maternal mortality [5]. Abstinence only programs are ineffective because they not only stop or delay adolescents from having sex but increase the risk of pregnancy as a result of unprotected sex when opportunity is availed.
When parents neglect the aspect of contraception in sex education, the risk of risky sexual behaviour amongst adolescents and its related complications increases [6,7]. Several inter-related factors hinder adolescent uptake of contraceptive services for example social cultural norm, lack of knowledge on contraceptive methods among adolescents, inadequate adolescent friendly services, health worker’s incompetence to work with adolescents and parent attitude on adolescent contraception usage consequently end up with unwanted pregnancies. Adults influence young people’s access to Adolescent Sexual and Reproductive Health (ASRH) information and services, as well as their ability to make healthful decisions. To ensure sustained positive behaviours among adolescents, the community must view these behaviours as beneficial, and community members must support change.
Although Uganda’s Total Fertility Rate (TFR) has declined from 7.4 to 5.4 children per woman between 1988/89 and 2016 respectively it is one of the highest. Yet still there is unmet need of family planning amongst married adolescents of 30.4% in Bukedi (Busia is part of this region) and with median age of first sexual intercourse at 16.4 years, the lowest in east Africa, there is need to think about a talk on ASRH. The overall estimated prevalence of adolescent pregnancy in Uganda is at 25%. Eastern Uganda registering rates higher than the national average, ranging from 28% in Busia to as high as 35.8% in Kibuku. Of concern is that contraceptive use in Uganda continues to be suboptimal at 33.7% in eastern Uganda despite Uganda having a high TP rate with dire consequences.
Conceptual framework
This was informed by the theory of Elaborate Likelihood Model (ELM) and Theory of Planned Behaviour (TPB) as postulated by Ajzen, et al. [8]. In TPB, this theory of planned. The TPB presupposes that individual behaviour represents conscious reasoned choice and shaped by social pressures and cognitive thinking. Furthermore, this is guided by the ELM theory. The attitude influenced by TPB is shaped by central and peripheral routes (Figure 1).
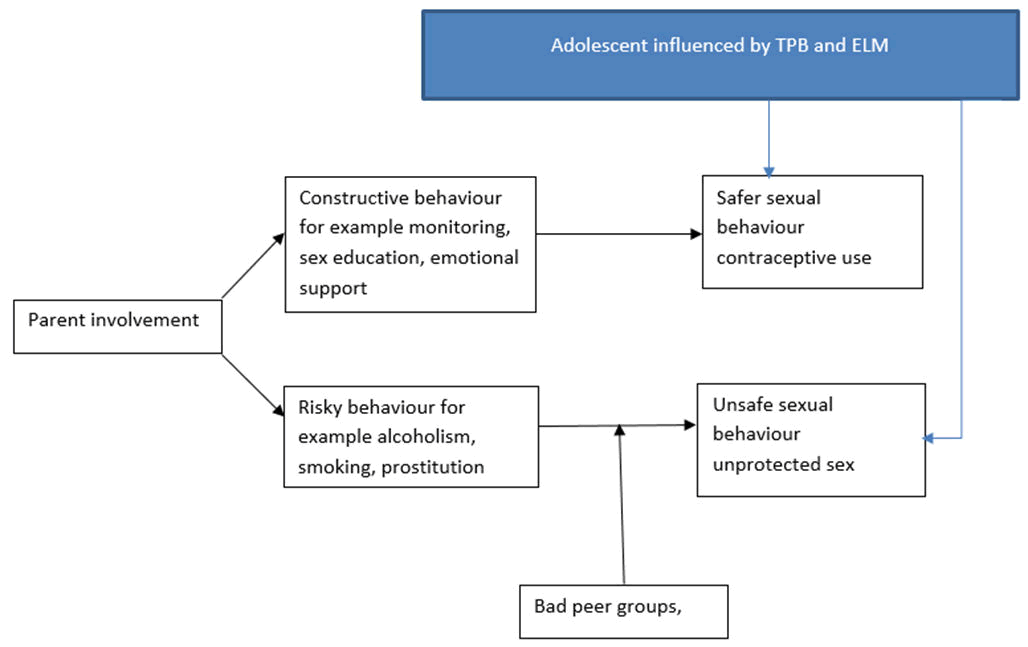
Figure 1. Adolescent influenced by TPB and ELM.
Constructive parental behaviour such as monitoring teenagers, parent sex talks and emotional support encourage adolescents to engage in safer sexual behaviour such as usage of condoms to avoid consequences involved. The external influences such as good peer groups, contraception advertisements also positively enforce the adolescents to avoid risky sexual behaviour such as unprotected sex. However, the un-exemplary risky parental behaviours such as alcoholism, smoking and prostitution alongside bad external influences such as bad peer groups exert an opposite effect to contraceptive uptake indicating that parents play a centre stage role in sexual behaviour of their children.
Study area
The study was carried out in Busia district in Eastern Uganda. It is bordered by districts of Tororo in the North, Bugiri and Namayingo in the West, Lake Victoria in the South, and the Republic of Kenya in the East. Busia district has one municipal council (Busia municipal council), 14 sub-counties, two divisions (Eastern and Western), 63 parishes and 537 (509 rural and 28 urban) villages. Busia has a total population of 323,662 persons of whom 87, 412 (27%), are adolescents. Of these adolescents, the percentage ever married ranges from 9.4-13.7% and 15.9% of adolescent female age 12-19 yrs have ever given birth.
Busia is one of the districts that hosts Busitema University Faculty of Health sciences (BUFHS) Community Based Education and Research Services (COBERS). Under this arrangement as research has elaborated, students are placed in the communities which simulate the likelihood populations they will serve. This has been explained in the earlier report (not published) by Nekaka, et al. We chose this district because it carries a teenage pregnancy rate higher than the national average of 25%
Study population
This constituted of adolescents aged 15-19 years both married and single. For those that were married, we asked them about sex and contraceptive use a year prior to marriage.
Study design
A cross-sectional descriptive design was employed in the communities of Busia district. We used mixed methods of quantitative and qualitative methods of data collection.
Sampling strategy
Multistage sampling strategy was used. Busia district is made up of one county, one municipality with fourteen rural sub-counties, no town council and two town divisions.
For sub counties, 7 rural sub-counties and one town division were chosen by simple random sampling without replacement. This helped eliminate the bias of choosing sub-county more than once. Villages were then randomly sampled form these sub-counties.
For selecting adolescents, a snow balling non-probability sampling technique was used. The first home was purposively selected. This was done with the help of the health assistants and village health teams (cadres that are very conversant with the villages). The teenager encountered would lead us to our next subject.
Sample size
We calculated the sample size using the Leslie and Kish formula N=Z2Pq/e2 where N=sample size, Z is the z-score for 95% confidence interval=1.96, P-probability of parents in influencing sexuality and contraceptive uptake by an adolescent is a half 50% (since to the best of our knowledge, no study had been done in this area), q=(1-p) and e-e is the desired level of precision, =5%
N=(1.96)2(0.5) (1–0.5)/(0.05)2
N=0.9604/0.0025=384
Assuming a 10% non-probability, actual sample size taken N0=384 +3.8=388 participants.
Ethics and consent
The study and all protocols were reviewed and cleared by Busitema University Faculty of Health Sciences (BUFHS) higher degrees and research and ethics committee as part of the Community Based Education and Research Services (COBERs) program for academic year 2019-2020. We further sought administrative clearance from Busia district local government.
Informed consent was obtained from all adolescents above or equal to 18 years and from the parents/parent-figures of adolescents <18 years. Adolescents below 18 years of age had to provide assent. However, adolescents 15 years and above with a baby or history of a birth were taken as emancipated minors and therefore provided consent. These are legal requirements of Uganda National Council of Science and Technology. Significantly, privacy and confidentiality of participant/s was respected. It was made clear to the participants that participation in the study was voluntary and one was free to opt out at any time without any negative consequences. Modest transport and lunch refund were provided to the participants.
Study procedure and data collection
To collect qualitative data, we relied on a structured questionnaire was used to capture respondents’ demographic characteristics, family background, education status, occupational status, role of parent in influencing contraceptive uptake among teenagers. This was developed by the research group and tested on 10 adolescents who had come to attend Mbale regional referral hospital. Data was entered into micro-soft excel and transferred to STARTA 4 for analysis. In univariate analysis, categorical variables were summarized as proportions, while continuous variables as means, median and Standard Deviations (SD). In the bivariate analysis, the chi-square test (for categorical variables) was used. Multivariable analysis using logistic regression, backward stepwise procedure was used to select variables to be included in the final model to determine the factors that were independently influenced contraceptive uptake among the teenagers. A P-value <0.05 was considered for statistical significance.
For qualitative data we collected it using Focus Group Discussions (FGD). The researchers had prior training in this kind of data collection. Each focus group consisted of 9-11 participants of same sex drawn from different villages and lasted for about 1 hour. In order to maximise confidentiality and openness, the village health teams, health assistants and parents/parent-figures took no part in the FGDs and used local council meeting venues for convenience.
The major languages used were Samia and English. This is ensured by the faculty allocating a student from the local area whenever possible to ease on the communication. The questionnaires and interview guides were developed by the COBERS group. We held 5 Focus Group Discussions (FDGs) that involved 53 adolescents. The number was influenced by the saturation point. Care was also taken to involve teenagers who had not been part of the quantitative study in order to get a local perspective of the subject matter. A purposive sampling technique was used. The groups involved teenagers in the age group 15-19 years, separate groups were made for boys as well as for girls in order to allow free expression of views.
The discussions were moderated by the researcher and notes taken by a rapporteur. After every focus group discussion, the recorded discussions were fully transcribed and translated verbatim into English. Each transcript was analyzed by two researchers working independently to reduce bias using NVIVO software version 13. Coding was done manually based on the key words and phrases developed from the data. The codes were then grouped together into higher order headings. Accordingly, on a higher logical level of abstractions codes, subcategories, categories, and themes were formed. The themes were categorized according to the experiences in relation to pregnancy, child bearing, child care, parental views, and reactions. +e data was sorted out thematically by clustering material with similar content. At this stage, we used a creative and analytical reasoning to determine categories of the meaning (Figure 2).
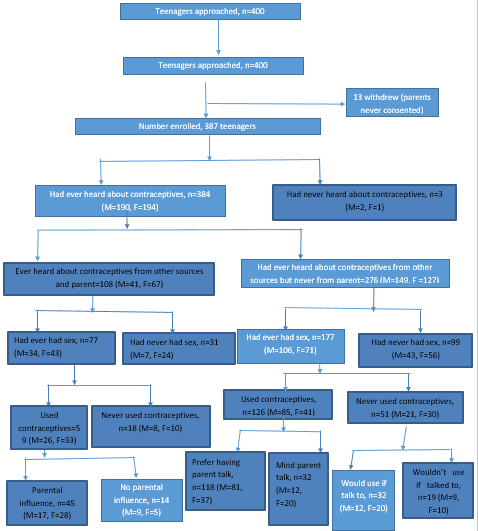
Figure 2. Study schema among the 387 participants.
Sociodemographic characteristics of the participants
Out of the 400 sample potential participants, 13 were non respondents while a total 387 adolescents aged 15-19 were enrolled into the study giving a response rate of 96.75%. Of these, 50.4% (195/387) were females while 49.6% (192/387) were males. Moreover, the majority, 85.5% were from rural counties of Majanji, Masafu, Masinya, Buhehe, Dabani and Masaba while 14.5% of the participants were from urban centre, Busia town.
A large number of adolescents 97.1% had had formal education with 44.4% of them having attended the basic seven years of primary level education. Notably 52.7% had had secondary level education. Furthermore, 72.1% (279/387) were single while only 27.9% (108/287) were married. Moreover, slightly above half, 52.5% (202/387) were still in school whereas 47.8% had stopped schooling. Of the adolescents that were out of school, 93% (172/185) were unemployed while only 7%(13/185) are employed.
Regarding the nature of family setting, the majority of the adolescents 63.8% were from nuclear family, 30.2% were from extended family while only 5.9% were from single parent families.
The majority of the adolescents were affiliated to the Christian faith, 84.2% (40.3% catholic, 34.1% protestant, 9.8% born again/ Pentecostal), 10.1% were Muslims while 5.7% belonged to others (Table 1).
| Variable | Sex | Total, n (%) | |
| Female (F), n (%) | Male (M), n (%) | ||
| Age | |||
| 15 | 13 (3.5) | 27 (6.8) | 40 (10.3) |
| 16 | 24 (6.2) | 40 (10.1) | 64 (16.3) |
| 17 | 48 (12.4) | 48 (12.4) | 96 (24.8) |
| 18 | 57 (14.7) | 34 (8.8) | 91 (23.5) |
| 19 | 53 (13.7) | 43 (11.1) | 96 (24.8) |
| Residence | |||
| Urban-Busia town | 30 (7.8) | 26 (6.7) | 56 (14.5) |
| Rural-Majanji | 27 (7.0) | 30 (7.8) | 57 (14.7) |
| Rural-Masafu | 35 (9.0) | 33 (8.5) | 68 (17.5) |
| Rural-Masinya | 26 (6.7) | 26 (6.7) | 52 (13.4) |
| Rural-Buhehe | 27 (7.0) | 26 (6.7) | 53 (13.7) |
| Rural-Dabani | 20 (5.2) | 20 (5,2) | 40 (10.3) |
| Rural-Masaba | 30 (7.8) | 31 (8) | 61 (15.8) |
| Marital status | |||
| Married | 69 (17.8) | 39 (10.1) | 108 (27.9) |
| Single | 126 (32.6) | 153 (39.5) | 279 (72.1) |
| Occupation | |||
| Currently student out of school | 96 (24.8) | 106 (27.4) | 202 (52.2) |
| Unemployed | 94 (24.3) | 78 (20.1) | 172 (44.4) |
| Employed | 5 (1.3) | 8 (2.1) | 13 (3.4) |
| Education status | |||
| No formal education | 4 (1.0) | 1 (0.3) | 5 (1.3) |
| Primary | 88 (22.7) | 84 (21.7) | 172 (44.4) |
| Secondary | 98 (25.3) | 106 (52) | 204 (52.7) |
| Tertiary | 5 (1.3) | 1 (0.3) | 6 (1.6) |
| Family setting one was raised in | |||
| Extended family | 45 (11.6) | 72 (18.6) | 117 (30.2) |
| nuclear family | 139 (35.9) | 108 (27.9) | 247 (63.8) |
| Single parent/parent-figure | 11 (2.8) | 12 (3.1) | 23 (5.9) |
| Religion | |||
| Born again | 23 (5.9) | 15 (3.9) | 38 (9.8) |
| Catholic | 88 (22.7) | 68 (17.6) | 156 (40.3) |
| Islam | 16 (4.1) | 23 (6.0) | 39 (10.1) |
| Protestant | 56 (14.5) | 76 (19.6) | 132 (34.1) |
| Other | 12 (3.1) | 10 (2.6) | 22 (5.7) |
| Total | 195 (50.4) | 192 (49.6) | 387 (100) |
Table 1. Socio-demographic characteristics of the 387 adolescent participants in Busia district, Eastern Uganda.
Prevalence of parent/parent-figure communication about contraceptives
Out of the 387 interviewed adolescents, only a few 27.9% (108/387) have ever had parent talk about contraceptives. More females 67/108 (62.1%) compared to males 41/108 (37.9%) had had the parent talk about contraceptives (Table 2).
Sexual intercourse rate and contraceptive use among adolescent participants in Busia
Noteworthy is the fact that 71.3% (77/108) of the adolescents that had ever heard about contraceptives from their parent’s/parent figures had ever had sex compared to 71.2% (177/276) of those that had not. In terms of contraceptive use, 76.6% (59/177) had used contraception in the talked to group versus 71.2% (126/177) in the category that had not been talked to.
Out of the 387 interviewed adolescents, 65.6% (254/387) had ever had sex with higher proportion of 71.3% (77/108) amongst those that had had parent/parent-figure talk compared to 61.1% of those that had not. Moreover, more males 55.1% (140/254) than females 44.9% (114/254) had had sex in the past year preceding the study.
Out of the 245 adolescents who had had sex, 72.8% (185/254) admit using contraceptives during sex. More males 60% (111/185) 40% (74/185) admitted using contraceptives. There was a higher proportion of contraceptive users, 77% (59/77) the group that had had parent/parent-figure talk compared to 71% (126/177) amongst those that had not (Table 2).
The need for parent talk among those that use contraceptives
The need for parent/parent-figure-teenage talk was 93.7% (118/126) among the 177 adolescents who had heard about contraceptives from other sources and used contraceptives. 71.2% (126/177) had had sex and admitted using contraceptives. More males 81/118 (68.6%) expressed this fact compared to females 37/118 (31.4%). However, a small number 8/126 (6.3%) expressed disinterest in parent talk about contraceptive usage. Equal number of females 4/8 (50%) and males 4/8 (50%) laid this fact bare (Table 2).
The need for parent talk among those that don’t use contraceptives
Amongst those that heard had about contraceptives from other sources and had sex and had not used contraceptives, 28.8% (51/177) did not use contraceptives. More females 30/51 (58.8%) than males 21/51 (41.1%) testified to this fact. More adolescents, 62.7% (32/51) expressed positivity about contraceptive use had parent/parent-figures talked to them (Table 3).
| Variable | Total n=254 (%) | Use contraceptive during sex | COR (95% CI) | P-value | |
| No, n=69 (%) | Yes, n=185 (%) | ||||
| Parent talked to one about contraceptives | 77 (30.3) | 18 (26.1) | 59 (31.9) | 1.3 (0.7, 2.5) | 0.371 |
| Which parent talked to you about contraceptives | |||||
| None | 177 (69.7) | 51 (73.9) | 126 (68.1) | 1 | 0.505 |
| Both | 2 (0.8) | 0 (0.0) | 2 (1.1) | 2.0 (0.1, 43.1) | 0.648 |
| Father | 30 (11.8) | 6 (8.7) | 24 (13.0) | 1.5 (0.6, 3.9) | 0.363 |
| Guardian father | 4 (1.6) | 0 (0.0) | 4 (2.2) | 3.7 (0.2, 69.3) | 0.387 |
| Guardian mother | 4 (1.6) | 2 (2.9) | 2 (1.1) | 0.4 (0.1, 2.4) | 0.323 |
| Mother | 37 (14.6) | 10 (14.5) | 27 (14.6) | 1.1 (0.5, 2.3) | 0.872 |
| Parent encouraged one to use contraceptives | 53 (68.8) | 5 (27.8) | 48 (81.4) | 11.3 (3.3, 38.5) | 0 |
| Prefer a parent talking to them about contraceptives | 219 (86.2) | 48 (69.6) | 171 (92.4) | 5.3 (2.5, 11.3) | 0 |
| Used contraceptive because parent told one | 69 (27.2) | 0 (0.0) | 69 (37.3) | 2.0 (0.03, 100.7) | 0.738 |
| Would use contraceptive if a parent encouraged to use | 43 (16.9) | 43 (62.3) | 0 (0.0) | 0.6 (0.01, 31.6) | 0.806 |
| Ever been pregnant | 45 (17.7) | 19 (27.5) | 26 (14.1) | 0.6 (0.3, 1.3) | 0.03 |
| Ever impregnated a woman | 27 (10.7) | 7 (10.1) | 20 (10.8) | 0.7 (0.3, 1.8) | 0.459 |
| Think contraceptive use is important | 234 (92.1) | 54 (78.3) | 180 (97.3) | 10.0 (3.5, 28.8) | 0 |
| Parents talked to one about relationship with people of opposite sex | 124 (48.8) | 22 (31.9) | 102 (55.1) | 2.6 (1.5, 4.7) | 0.001 |
| Parents know one’s usual whereabouts | 130 (51.2) | 34 (49.3) | 96 (51.9) | 1.1 (0.6, 1.9) | 0.711 |
| Parent’s religion affect one’s contraceptive uptake | 77 (30.3) | 19 (27.5) | 58 (31.4) | 1.2 (0.7, 2.2) | 0.193 |
Table 2. Relationship between parent/parent figure talk and contraceptive use on bivariate analysis.
| Variable | COR (95% CI) | P-value | AOR (95% CI) | P-value |
| Parent talked to one about contraceptives | 1.3 (0.7, 2.5) | 0.371 | 6.7 (1.3, 34.5) | 0.023 |
| Prefer a parent talking to them about contraceptives | 5.3 (2.5, 11.3) | 0 | 0.4 (0.03, 4.3) | 0.422 |
| Ever been pregnant | 0.6 (0.3, 1.3) | 0.03 | 1.5 (0.3, 7.8) | 0.616 |
| Parents talked to one about relationship with people of opposite sex | 2.6 (1.5, 4.7) | 0.001 | 2.7 (0.5, 13.2) | 0.226 |
Table 3. Relationship between parent/parent-figure talk and contraceptive use on multivariate analysis.
Contraceptive knowledge and use
The higher the number of sources of contraceptive knowledge one is exposed to, the greater the level of exposure. The sources of contraceptive knowledge considered here included; parent/parent figures, peers, print and digital media, health workers, teachers (N Number of contraceptives exposed to, 0 none, 1 at least one, 2 at least 2, 3 at least 3, 4 at least 4, 5 at least 5.
Significantly, a large number of adolescents 99.2% (384/387) had ever heard about contraceptives while 0.8% had not. Moreover, of the 99.2%that had ever heard about contraceptives, 50.5% were males while 49.5% were females. Additionally, close to half of the adolescents 48.6% (188/384) had ever heard about contraceptivesfrom multiple sources. Those that had ever heard about contraceptives from single source, did so largely from radio, 10.3%.
Notwithstanding, 4.9% (19/384) of the adolescents reported to have heard about contraceptives from their parent’s/parent figures only. Noteworthy still is the fact that 89.5% (17/19) had heard from the mother/mother figure while only 10.5% (2/19) had ever heard from both genders.
Of the 108 teenagers/adolescents that had heard about contraceptives from the parent’s/parent figure and another source, only 1.9% (2/108) did so from both genders. Moreover, in both categories less than 50% of the participants had ever had a talk on contraceptives with the parent (females, 34.4%, 67/195 compared to males, 21.4%, (41/192) (Table 4).
| Number of sources of information adolescent was exposed to | Female, n | Male, n | Total, n |
| 1 | 85 | 54 | 139 |
| 2 | 49 | 42 | 91 |
| 3 | 30 | 59 | 89 |
| 4 | 26 | 39 | 65 |
| 5 | 9 | 2 | 11 |
| Source | Female, n (%) | Male, n (%) | Total, n (%) |
| Parent/Parent figure only | 8 | 11 | 19 |
| Parent/Parent figure+other sources | 67 | 41 | 108 |
| Health worker only | 33 | 12 | 45 |
| Peers only | 6 | 7 | 13 |
| Print and digital media | 25 | 16 | 41 |
| Teachers only | 13 | 8 | 21 |
| multiple sources (more than two source) | 74 | 108 | 188 |
| If parent/parent-figure, who in particular? | |||
| Parent/parent figure | Female | Male | Total |
| Both | 2 | 0 | 2 (1.9) |
| Father | 7 | 30 | 37 (34.3) |
| Father parent figure | 4 | 2 | 6 (5.6) |
| Mother | 48 | 9 | 57 (52.8) |
| Mother parent figure | 6 | 0 | 6 (5.6) |
| Total | 67 | 41 | 108 |
Table 4. The number and sources of information about contraceptives to the adolescents in Busia, eastern Uganda.
Knowledge and contraceptive use
We further graded knowledge depending on the number of participants that had ever heard about a contraceptive method: 0 none, 1 one contraceptive, 2 wo contraceptives, 3 three kinds of contraceptives 4 kinds of contraceptives and 5, for 5 methods.
Significantly only 1% (4/384) of the adolescents could not recall any contraceptive method and all were females. Moreover, all and the 99% (380/384) that could recall a contraceptive method, mentioned only modern methods. The single commonest method recalled was the condom, 48.7% (187/384) (Table 5).
| N | Contraceptive method | Female, n (%) | Male, n (%) | Total, n (%) |
| NA | Never heard | 1 (33.3) | 2 (66.7) | 3 |
| 0 | None | 4 (100.0) | 0 (0.0) | 4 (1.0) |
| 1 | Implants | 3 (100.0) | 0 (0.0) | 3 |
| Condom | 75 (40.1) | 112 (59.9) | 187 | |
| Injectable | 1 (100.0) | 0 (0.0) | 1 | |
| IUDS | 1 (100.0) | 0 (0.0) | 1 | |
| Pills | 4 (80.0) | 1 (20.0) | 5 | |
| Subtotal | 84 (42.6) | 113 (57.4) | 197 (51.3) | |
| 2 | Condom+implant | 1 (33.3) | 2 (66.7) | 3 |
| Condom+injectable | 15 (48.4) | 16 (51.6) | 31 | |
| Condom+pill | 13 (46.4) | 15 (53.6) | 28 | |
| Injectable+implants | 1 (100.0) | 0 (0.0) | 1 | |
| Pill+injectable | 5 (60.0) | 1 (40.0) | 6 | |
| Subtotal | 35 (50.7) | 34 (49.3) | 69 (18.0) | |
| 3 | Condom+implant+injectable | 9 (81.8) | 2 (18.2) | 11 |
| Condom+pill+injectable | 33 (60.0) | 22 (40.0) | 55 | |
| Subtotal | 42 (63.6) | 24 (36.4) | 66 (17.2) | |
| 4 | Condom+pill+injectable+implant | 25 (64.1) | 14 (35.9) | 39 |
| Pills+injectable + implant+IUD | 1 (100.0) | 0 (0.0) | 1 | |
| Condom+pill+implant+IUD | 3 (50) | 3 (50) | 6 | |
| Subtotal | 29 (65.0) | 17 (35.0) | 46 (12.0) | |
| 5 | Condom+pill+injectable+implant+IUD | 0 (0.0) | 2 (100.0) | 2 |
| Subtotal | 0 (0.0) | 2 (100.0) | 2 (0.5) | |
| Total | 194 | 190 | 384 | |
| Note: NA: Applies to those that have never heard about contraceptives; None: Applies to those who have ever heard about contraceptives but do not remember any example | ||||
Table 5. Contraceptive methods mentioned/recalled by the 384 adolescents that heard ever heard about contraceptive method in Busia district eastern Uganda.
Level of contraceptive encouragement
Of the 108 adolescents that had ever heard about contraceptive use from their parent’s/parents figure, 65.7% (71/108) felt encouraged to use contraceptives during sex with 61.9% (44/71) being females while 38.1%(27/77) were males. Significantly 34.3% (37/108) did not feel influenced by the parent/parent figure talk (Table 6).
| Did adolescent feel encouraged by the parent/parent figure talk to use encourage contraceptives? | |||
| Response | Female, n (%) | Male, n (%) | Total, n (%) |
| Felt encouraged | 44 | 27 | 71 (65.7) |
| Felt discouraged | 23 | 14 | 37 (34.3) |
| Total | 67 | 41 | 108 |
| Contraceptive method one felt encouraged to use | |||
| Contraceptive | Female, n (%) | Male, n (%) | Total, n (%) |
| Abstain only | 23 | 14 | 37 (34.3) |
| Condoms only | 1 | 1 | 2 (1.9) |
| Contraceptive pills only | 4 | 0 | 4 (3.7) |
| Implants only | 2 | 0 | 2 (1.9) |
| Injectables only | 6 | 0 | 6 (5.6) |
| IUDS only | 1 | 0 | 1 (0.9) |
| Condoms+injectables | 1 | 0 | 1 (0.9) |
| Contraceptive pills+implants | 2 | 0 | 2 (1.9) |
| Pills+condoms+injectables | 6 | 0 | 6 (5.6) |
| Condom+implants+injectables | 1 | 0 | 0 (0) |
| Pills+condoms+implants+injectables | 1 | 0 | 1 (0.9) |
| Pills+condoms+implants+IUDS | 12 | 24 | 36 (33.3) |
| Any | 8 | 2 | 10 (9.3) |
| Total | 67 (62) | 41 (38) | 108 (100) |
Table 6. Perceived parental/parental figure influence on contraceptive use.
Qualitative findings
Qualitative information generated from the FGDs were analyzed manually using thematic analysis according to emerging themes. Transcribed data were coded and main emerging themes were identified and presented as text quotes.
Sociodemographic characteristics of the study participants
Majority of the participants were Christians 84.8% and single 86.0%. Importantly, only 30.2% were students and 12/47 (25.5%) of those that were out of school were employed (Table 7).
| Variable | Sex, n (%) | Total, n (%) | |
| Female | Male | ||
| Age | |||
| 15 | 8 (15.1) | 4 (7.5) | 12 (22.6) |
| 16 | 6 (11.3) | 3 (5.7) | 9 (17) |
| 17 | 7 (13.2) | 4 (7.5) | 11 (20.7) |
| 18 | 5 (9.4) | 7 (13.2) | 12 (22.6) |
| 19 | 5 (9.4) | 4 (7.5) | 9 (17) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Residence | |||
| Majanji | 5 (9.4) | 4 (7.5) | 9 (17) |
| Rural-Masafu | 6 (11.3) | 3 (5.7) | 9 (17) |
| Rural-Masinya | 4 (7.5) | 4 (7.5) | 8 (15) |
| Rural-Buhehe | 5 (9.4)) | 4 (7.5) | 9 (17) |
| Rural-Dabani | 6 (11.3) | 5 (9.4) | 11 (20.7) |
| Rural-Masaba | 5 (9.4) | 2 (3.8) | 7 (13.2) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Marital status | |||
| Married | 4 (7.5) | 3 (5.7) | 7 (13.2) |
| Single | 27 (50.9) | 19 (35.8) | 46 (86.7) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Occupation | |||
| Currently student | 7 (13.2) | 9 (17) | 16 (30.2) |
| Currently out of school | 0 (00) | 0 (00) | 0 (00) |
| Unemployed | 16 (30.2) | 9 (17) | 25 (47.2) |
| Employed | 8 (15.1) | 4 (7.5) | 12 (22.6) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Education | |||
| Never | 3 (5.7) | 4 (7.5) | 7 (13.2) |
| Primary | 15 (28.3) | 5 (9.4) | 20 (27.7) |
| Secondary | 10 (18.9) | 9 (17) | 19 (35.9) |
| Tertiary | 3 (5.7) | 4 (7.5) | 7 (13.2) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Family | |||
| Extended | 10 (18.9) | 2 (3.8) | 12 (22.7) |
| Nuclear family | 15 (28.3) | 13 (24.5) | 28 (52.8) |
| Single parent | 6 (11.3) | 7 (13.2) | 13 (24.5)) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
| Religion | |||
| Born again | 8 (57.1) | 6 (11.3) | 14 (68.4) |
| Catholic | 10 (18.9) | 7 (13.2) | 17 (32.1) |
| Islam | 2 (3.8) | 3 (5.7) | 5 (9.5) |
| Protestant | 9 (17) | 5 (9.4) | 14 (26.4) |
| Other | 2 (3.8) | 1 (1.9) | 3 (5.7) |
| Total | 31 (58.5) | 22 (41.5) | 53 (100) |
Table 7. Social demographics for 53 adolescents that participated in the Focus Group Discussions (FGDs) in Busia district Eastern Uganda.
To determine the enablers and hindrances of parent role on contraceptive uptake amongst adolescents in Busia
Majority of teenagers had multiple reasons why they thought parent’s/parent figures do not talk about or encourage them about contraceptive use. The majority of the adolescents thought parent’s/ parent figures were too shy to confront their children (45%), 43%, did not know why the parent/parent figures did not engage in talks to do with contraceptive use while 12% thought that they didn’t want their children to know since they are too young (teenagers would experiment with contraceptives after hearing their parents (Table 8).
| Variable | Number, n (%) |
| parents/parent-figures are shy to confront us and talk about contraceptives | 24 (45) |
| Parent/parent figures do not want us to know because they perceive us being very young | 23 (43) |
| I don’t know why they don’t engage us | 6 (12) |
Table 8. Summary of the teenagers’ perceptions as to why parent/parent figures did not talk to them about contraceptives.
Enablers
Family background: “I am the 3rd born in a home of 10 children, my father has 3 wives but he cannot take care of all of us. Some of my siblings got married at a young age because there was no food at home. When I grow up, I want to marry one husband and have few children. I have heard this is possible with birth control methods like “empiiso”, said 29-year-old female.
Parents as role models: In a focus group discussion, most male teenagers believed that they are more likely to use a condom when their fathers encourage its use.
“My father is a role model to me, I look up to him. Whatever he says I can do. If he ever tells me to use contraceptives during sex, I will use because I know he is always right” ………narrated by 17-year old male.
“My father has ever told me to use condoms during sex, he said all girls in my village are sick and he is not ready for grandchildren.” ‘For this reason I use a condom whenever I decide to do the act’, Narrated by 18-year-old male student.
Hinderances
Poverty: Most parents in the village are very poor. “The poor parents encourage their children to become pregnant so that they can be exchange for dowry money and relieve their family of a financial burden.” …. narrated the 18-year-old male.
Unknown reasons: In an interview, a 17-year-old male mentioned that “I don’t know why my parents don’t tell us about contraceptives. I don’t even know whether my parents use them. I also shy away from using them because I don’t want my parents to find out”
Corporal punishments: ‘Most parents cane their sons if they talk about sex or find condoms in their bedrooms. They conclude that they have been engaging in premarital sex even before you explain. I cannot open up to my parent to discuss contraceptive issues, they will abuse me” …18-year-old male student.
Parents are less informed: Some teenagers said that their parents discourage contraceptives because they might never produce again. “My parent told me that if I use injectaplan before ever giving birth, I will become barren forever. I also don’t know if it is true” ………18 year-old female housemaid.
Parents fear to talk to their children: Most teenagers were not talked to by their parents about contraceptives because they didn’t want their children to know since they consider them too young.
“I heard about condoms from my friend at school. I have never asked my parents about it. I think parents fear to talk to their children because they might also not be knowing or they think we are too young to know. They say we might get spoilt” …16-year-old male student.
Parents emphasise abstinence only: Other teenagers said it is not good for a parent to talk to their children because it would encourage teenagers to experiment early sex instead of abstaining.
“My father is a pastor; he says God condemns sex before marriage. He only tells me to avoid bad groups and abstain from sex to avoid getting pregnant when am still young. He has never talked about contraception. I heard it from my friends” …16-year-old female student.
Parents discourage the children: “I cannot use injectable and pills because my parent told me they caused her prolonged bleeding especially during menstruation” ……….19-year-old female student.
Some teenagers on family planning complained of reduced libido, stress and excessive weight gain wishing that they had been foretold of the consequences by their parents.
“I agreed with my husband to only have sex during my safe days. I do not like implants because I experienced throbbing headaches when I last used them. Besides, my parents had fore warned me against their use. I now know why she had done so” …………19-year old female housewife.
“My parent told me that if I don’t see menses after a month blood would have accumulated in the uterus”. I fear using family planning because such occasions are common…….16-year female old student.
Negative community perception about contraceptives: The teenagers also urged that the community had negative perception of a teenager who would be seen buying a contraceptive.
“It is very hard for me to collect condoms from the hospital when old people and other parents are looking at me. I feel uncomfortable them looking at me as badly behaved. They utter insultingly rude comments such as “oyo omwaana mwenzi (literally meaning that child is a harlot”. He continued, ‘I would suggest that the hospital should put a youth corner where we can get these materials without being noticed’’………18-year-old male brick layer.
Adolescents’ misconception about sex with barrier method
Some perceived sex with a barrier method as a barrier to sweetness.
“Sex is not sweet when using a condom, there is no feeling… pause,” “Have you ever eaten sweets when they are still in a kaveera (literally meaning polythene paper!” ….16-year-old male student.
Although there is a dire need for investment in adolescent sexual and reproductive health, appreciation of the interlocking familial relations and adolescent development has to be made to facilitate a productive discussion on Adolescent Sexual and Reproductive Health (ASRH). From earlier reports, the family is known to operate as a multilevel social system with interlocking relationships, in which parent-child and spousal subsystems are multiply interlinked by a network of interdependencies that reliably influence one another rather than a just a collection of members independently functioning. It therefore spells a dynamic interplay among the dyadic relationships.
This adolescent development from an agentic perspective highlights how the adolescents are contributors to their lives not just by-standers. The best predictors of sexual risk taking among adolescents include but not limited to perceived self-efficacy, or belief in one’s ability to exert control over one’s sexual behavior [9]. Reinforcing contexts supportive of positive youth development, such as the family and in particular parents, and the prevention of adolescent problem behaviour will decrease the likelihood of significant disease burden during adolescence and in later life.
It is inevitably clear that today’s investment in the adolescent is a life-time investment. Adolescent Sexual and Reproductive Health (ASRH) is not only critical to the adolescents’ today’s health but also has serious implications for shaping future adult health. Adolescence behaviours practices are thus linked to health burden in the latter life.
This study purposed to explore the impact of parent/parent figure-teenage communication on contraceptive use. The response rate in this study was over 96.75% a good response rate that is comparable to other studies in the same geographical and subject area. This may be due to a good relationship established by the COBERS programme at the faculty and the community.
In this study, the prevalence of parent/parent-figure-teenage talk on contraceptive use was 27.9% (108/387). A study amongst the Dutch adolescents found that 75% of parents reported having ever had a sexual related discussion with their adolescents and romantic relationships were discussed most. This Dutch study on parent adolescent communication on protection and contraceptive use further revealed a positive influence on contraceptive pill use. A study amongst the African-Americans revealed same finding. It may seem a more open practice in some parts of the West than Africa.
In this study, 65.6% (254/387) were found to have had intercourse within the past 1 year. This compares with the study done in Nairobi, Kenya (Uganda’s neighbour to the east) in which 60% of the adolescents were reported to have been engaged in sex in the 1 year prior to the survey [10]. A study in Nigeria revealed a low rate of 14.1%. However, this may be explained by the study that reported significantly higher early sexual debut in Eastern Uganda than elsewhere with males more affected that their female counterparts.
Of the adolescents that had had sex in the past 1 year, 74.8% (185/254). This is higher than has been reported in studies in Uganda about contraceptive use may be explained by high levels of HIV prevalence of in neighbouring Busia Kenya of 9.9% and thus many taking extra caution.
At multivariate level the statistically significant factor associate with use of contraception was the parent/parent-figure talk about it with the adolescent (AOR=6.95% CI 1.3-34.5, p=0.023). In this study, more females were talked to than males (34.4% versus 21.4%) and more adolescents seemed to be talked to by a female parent/ parent-figure. These findings are in agreement with findings by a study amongst the Yoruba in Nigeria that reported adolescents being closer to their mothers than fathers a result of warmth and affection the former accords them compared to the latter and in the USA amongst African American males received as teenager [11].
Also in a study in Nigeria, fathers were reported to be more authoritarian while mothers were reported to be more permissive and this had a positive and negative attitude on premarital sex respectively. Other studies have collaborated the findings that authoritarian parenting in contrast to permissive parenting and liberal parenting is likely to discourage premarital sex and sex debut.
The relationship between family structure and effect on sexual debut. Female and male youth sexual activity is associated with a dysfunctional or impaired family system in the absence of parental supervision [12]. Moreover, Achema, et al. reported in their study on perceptions of secondary school teens on teenage pregnancy, the teenagers, 60%, largely blamed them woos on a polygamous family setting. Evidence reveals that male youth raised by men and girls raised by grandmothers are less likely to engage in sex and if they do so are likely to have less sexual partners. Maternal disapproval of premarital sex and satisfaction with the mother-child relationship have been reported to significantly lead to abstinence from adolescent sexual activity, less frequent sexual intercourse and more consistent use of contraceptives among sexually active youth. This underscores further the role of social support in protection of both genders.
Additionally, a study in SSA found family structure to be a strong determinant of delay of sexual debut with odds of delay being higher in females with parents. Moreover, a study in Kenya, revealed a positive association between parent-child connectedness and sexual behaviours such as condom use and less likelihood of multiple sexual partners, and much more if the adolescent lived with the biological parent. Furthermore, higher levels of mother-daughter sexual risk communication have been associated with fewer episodes of sexual intercourse and unprotected intercourse at 3 month follow-up. Moreover, adolescent girls in Spain who were found to be in a good relationship with their mothers were less likely to engage in risky sexual behaviour such as having multiple sexual partners or a history of Sexually Transmitted Illness (STI). Relatedly a retrospective study that examined maternal demandingness (Odds Ratio (OR)=0.77) and maternal responsiveness (OR=0.89) independently predicted adolescent abstinence from sex [13]. Furthermore, a study conducted in Uganda posited that the absence of both parents from the household was associated with earlier sexual debut in female youth and the father figure was the dominant protective parental figure.
In a review of literature by Subedi, et al. the group reported various socio-cultural and traditions, lack of comprehensive knowledge on contraceptives, lack of adolescent friendly services with proper skilled persons to run them. Similar concerns were raised by another study by Nandyose, et al. and in addition, Munakampe, et al. reported adolescents shunning parents for information yet they were considered trusted sources.
In our study, adolescents revealed hesitance by parents/parent figures to engage them in sex talk. The majority of the adolescents 45%, thought parents/parent-figures feared to confront their children while 12% thought their parent’s/parent figures thought they were still young to engage in sex and contraceptives use talk. This agrees with the findings by Muhwezi, et al. who reported that in Uganda, there was fear by the female adolescents to engage in sex talk as this would signal active sexual engagement. Therefore, discussing about sex was perceived as culturally inappropriate and when it does occur, is normally parent-led, vague, unidirectional, and authoritarian leading to a closed dialog. Furthermore, a study in Masaka and Kampala in Uganda Marjorie, et al. reported that parents had resorted to using frightening their daughters into avoiding sex; being “strict”; and relying on mothers rather than fathers to “counsel” daughters about sex and transactional sex [14]. to engage in sex talk as this would signal active sexual engagement. Therefore, discussing about sex was perceived as culturally inappropriate and when it does occur, is normally parent led, vague, unidirectional, and authoritarian leading to a closed dialog. Furthermore, a study in Masaka and Kampala in Uganda Marjorie, et al. reported that parents had resorted to using frightening their daughters into avoiding sex; being “strict”; and relying on mothers rather than fathers to “counsel” daughters about sex and transactional sex [14].
These challenges notwithstanding, parental communication, monitoring, and closeness have been associated with reduced sexual risk taking among young people, including delay of sexual debut, safer sex practices and fewer sexual partners and other health benefits beyond sexuality such as greater emotional ell being, less substance abuse, less eating disorders and obesity outside Africa [15]. Moreover, studies undertaken in Sub-Saharan Africa (SSA) have also intimated similar findings that parent adolescent connectedness is associated with safer sexual practices and better mental health, educational, and developmental outcomes albeit with challenges such as parents lacking the time, confidence, knowledge and or skills to deliver age-appropriate sexual and reproductive health messages.
In our study, 99.2% adolescents had ever heard about contraceptives and majority had done so from other sources. Only 4.9% had heard from parents/parent-figures only. These corroborated findings in Bududa in eastern Uganda that reported 92% of the adolescents had ever heard about contraceptives and health workers were the major source of information. Only 8% had done so from parents compared.
In this study majority of the adolescents had heard about a single contraceptive 51% (196/384) and condom was the best known of the contraceptives. This is in line with a study in Bududa that reported poor contraceptive knowledge although in contrast, more adolescents knew of pills. The difference could be explained by the study population differences. Whereas in this study we had almost as many females as males, the study in Bududa recruited only females.
Moreover, in our qualitative analysis, the adolescents felt parents were not knowledgeable enough, were fearful or for unknown were not empowered to empower their children. These findings corroborate ones in a study in Ethiopia that reported the adolescents that perceived their parents not knowledgeable about issues of ASRH were three times more likely to engage in risky sexual behaviour compared to ones that considered parents knowledgeable.
Another barrier that came out was the misconception about use of barrier method condom yet it is the one they seemed to know most. They equated using it to eating sweet from a Kaveera (polyethane paper). These misconceptions about contraceptives have been reported in a study in Uganda, Nigeria and even among adults in a met-analysis in African urban centres and even in Pakistan (condoms were alleged to spread infections and lead to impotence [16].
Other barriers highlighted in this study were negative perception by parent/parent figures if adolescents started any discussion to do ASRH. Additionally, adolescents cannot easily access contraceptives because community would perceive them in same spirit. Adolescents narrated that they would be taken as prostitutes and harlots. This has been documented in other studies as a negative influencer of an open discussion. These sentiments have been voiced by studies in Uganda and elsewhere [17].
In this study most parent/parent figures advised their children to abstain. This corroborates earlier finding in a study in Bududa in Uganda. However, Nandyose, et al. in Uganda reported about the ineffectiveness of abstinence only messages as did other studies. Societal norms that are rooted in Ugandan and African culture and religion contribute to limiting access to contraceptive information and services for adolescents. Religion considers premarital sex as sinful, and adolescents are culturally obliged to abstain from sexual intercourse until they are married. Moreover, community perceives exposure to contraceptives would encourage promiscuity and early contraceptive knowledge by adolescents which tantamount to moral decadence [18].
Another prominent barrier that was highlighted was the corporal punishments adolescents would face if they were found with contraceptives by those that wield power over them. Uganda is fairly a religious country or largely Christian (over 85%) for that case as reported in demographic surveys. This is further clearly demonstrated in the background characteristics of our respondents. Religiosity has profound effect on contraceptive use and sexuality as it sets norms that discourage premarital, extramarital and transactional sex but also promote family unity all factors that would delay sex debut and lead to safer sex practices. These norms could result in exclusion and stigmatization of adolescents who need contraceptive services. Societal and policy and stigmatization of adolescents who engage in premarital sex is a major contributor to underutilization of reproductive health services and teenage pregnancies [19]. Community dialogue and focus group discussions involving key stake holders such as parents, policy makers and community leaders could be useful for deconstructing societal norms and misconceptions about adolescent sexuality and access to contraception.
Literature reports that the level of exposure/sources of information can correlate with improved knowledge and have influence on the adolescents depending on the quality and content. In this study at least, 49% (188/384) adolescents had been exposed to at least three sources of information on contraception Wado, et al. reported that exposure to at least three media house was protective in Kenya, Malawi and Uganda but not in Zambia and Tanzania. L’ Engel, et al. reported the negative influence of sexual content laden media exposure to adolescents in the United States of America (USA) [20]. Amongst the African American males, it was reported that the amount of information one gets impacts on the frequency of us of birth control.
Finally, there is clear need to educate the adolescents especially through school programmes and parents and other society members about sexuality, STIs and HIV and the topic of contraception. However, since African cultures and religion are very conservative about the topics, well-tailored, calculated non inflammatory messages need to be designed
Parent-teen communication is a vital part of adolescent development and greatly affects sexual behaviour and other aspects of development including mental and psychological well being. In this study, it was the most significant factor that influenced contraceptive use amongst the teenagers in Busia district.
Given Uganda’s high teenage pregnancy rate coupled with high fertility rate, high maternal mortality ratio, perinatal mortality and high adolescent HIV associated mortality, fostering family core values and ensuring parent/parent-figure involvement in the adolescents lives and contraceptive investments would be a sensible public health measure to curtail such issues.
The study sought retrospective data and this can generate recall bias especially for those that were married. There also a component of the teenagers wanting to mention what they think the researchers should hear such as parent/parent-figures being more responsible. This study should therefore be interpreted in the context of these limitations.
Ivan Lyagoba (IL), Edrine Waibi (EW), Joan Namatovu (JN), Walter Atwijukire (WA), Irene Manakhe (IM) and Julius Nteziyaremye (JN) conceptualised the idea and wrote the proposal.
IL, EW, JN, AW, IM and JN collected the data.
IL, EW, JN, AW, IM and JN curated the data.
IL, EW, JN, AW, IM and JN and RN wrote the manuscript. All authors read and approved the final manuscript.
We are indebted to the leadership of Busia district and the people of Busia for the good reception and working relationship as Busitema University students.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Lyagoba I, et al. "The Role of Parent/Parent-Figure-Teenager Communication on Sex and Contraceptive Use: A Case Study of Busia in Eastern Uganda". Primary Health Care: Open Access, 2025, 15(1), 1-14
Received: 10-Jan-2024, Manuscript No. JPHC-24-124886; Editor assigned: 12-Jan-2024, Pre QC No. JPHC-24-124886 (PQ); Reviewed: 26-Jan-2024, QC No. JPHC-24-124886; Revised: 19-Mar-2025, Manuscript No. JPHC-24-124886 (R); Published: 26-Mar-2025, DOI: 10.35248/2471-8556.25.15(1).495
Copyright: © 2025 Lyagoba I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.