Research - (2021) Volume 11, Issue 10
Background: Nutrition is valuable for disease resistance, physical wellbeing, maturation and mental development as well as it breaks intergenerational malnutrition. However, in most developing countries, under nutrition is one of the common public health problems, especially in lactating mothers. Therefore, this study was conducted to assess prevalence of under nutrition and associated factors among lactating mothers in Mizan Aman Town,Bench Sheko Zone, Southwest Ethiopia.
Methods: A community based cross-sectional study was conducted from April 01 to May 03, 2020 among randomly selected 548 lactating mothers. Binary logistic regression was done to assess association between independent and dependent variable. Adjusted Odds Ratios with its 95% confidence interval were estimated to identify factors associated with the outcome variable in multivariable logistic regression.
Results: A total of 527 lactating mothers were participated in this study with response rate of 96.5%. The prevalence of under nutrition was 23.7%. Identified Factors associated with under nutrition among lactating mothers were educational status of women[AOR=7.53,CI:(1.237, 25.373)],women dietary diversity score[AOR=4.461,CI:(1.732,11.492)], age of first pregnancy [AOR=1.660,CI: (1.321,3.466)],and family size status [AOR=1.83,CI:(1.026,3.271)].
Conclusion: According to WHO classification, the prevalence of under nutrition among lactating mothers in the study area was high. Thus, strengthening health education on proper maternal and child dietary practices and adequate dietary intake during lactation is beneficial, multi-sectorial collaboration targeted at improving women’s status in community is very
Under nutrition, Lactating Mothers, Mizan Aman, Southwest, Ethiopia
Under nutrition and poor health from preventable causes excessively affect in the developing country in the world. Under nutrition among women have a major impact on their health, and their children’s health [1,2]. Under-nutrition is result of the interaction of food, care, and health. Proper nutrition during lactation is important for optimum growth, maturation, physical wellbeing, mental development, and disease resistance, also breaks intergenerational of malnutrition [3-6]. In Sub- Saharan Africa (SSA), under-nutrition during pregnancy and lactation is a widespread problem due to monotonous, plant-based diet which is not meets the requirement [7].According to WHO cut off point values for the public health significance of prevalence, if adults with BMI<18.5 was 5-9% low prevalence,10-19%: Medium prevalence,20–39% High prevalence and if ≥40%Very high prevalence [8]. In Ethiopia, the prevalence was 22% based on 2016 EDHS [9].
Globally, every year reported 14 million girls enter to lactation. Which is more than 90% live in developing countries [10]. Under nutrition causes more than 3.5 million deaths among women and children every year and accounts for 11% of disability-adjusted life years globally [3]. In developing countries specifically in sub-Saharan Africa (SSA), south-central and south-eastern Asia, more than 20% of women were underweight. In Ethiopia, 22% of reproductive age women are undernourished [9]. Among the regions, more than one-third of women found in Afar,Gambella,Somali,and Tigray were undernourished [2].
Evidence done in Ethiopia reported that under nutrition was significantly associated with age, marital status, and occupation of the women [2]. Variable like safe drinking, hand hygiene before and after prepare and eating, knowledge on nutrition, wealth status and dietary diversity are not fully included in previous studies, but we are included in this study. Furthermore, there was few studies documented on under-nutrition among lactating women in Ethiopia, and no documented study is found in the study area. Therefore, this study aims to assess the prevalence of under-nutrition and associated factors among lactating mothers in Bench Sheko Zone, Southwest Ethiopia.
Study design, setting, and area
Community-based cross-sectional study design was conducted, and conducted from April 01 to May 03, 2020 in Bench-Mizan Aman Town, Sheko Zone, Southwest Ethiopia. Mizan Aman is the zonal Town of Benchsheko Zone and, found 561 km from the capital city Addis Ababa. The total population of Mizan Aman Town is estimated of 49,590, of which 11,554 are women in the 15-49 age groups. From this, 4019 are lactating mothers [11]. All lactating women who have 6-23 months of age child in Mizan Aman Town were included in the study. On the other hands, lactating women who are ill during data collection and who are pregnant were excluded from the study.
Sample size determination
Sample size was estimated using Epi InfoTM7 by using the formula for estimation of a single population proportion for under nutrition and two population proportion formulas for associated factors with the following assumptions: prevalence of under nutrition among lactating mothers 38% [12], 95% confidence level, 5% margin of error, 1.5 design effect and adding a contingency for a non-response rate of 10%. Thus, a total of 548 lactating mothers were included.
Sampling procedure
In this study cluster sampling method was employed by considering Kebeles as clusters, from the total six Kebele, three were selected randomly by lottery method. Health extension workers have already documented a number of lactating women found in each Kebele in a family folder and also the number of household which has lactating women lived in each kebele are known. Finally, Proportional allocation to the sample size was done ,and the lactating mothers was selected using a simple random sampling by reference the community health worker family record book as a sampling frame.
Data collection instruments and procedure
Questionnaire was developed in English and then translated into the Amharic language for simplicity then back-translated to the English language for its consistency by two different language expert individuals who speak both Amharic and English fluently. Socio-demographic data, nutritional knowledge, Anthropometric, dietary diversity score, maternal health care and feeding practices were assessed.
Anthropometric measurements: A height measurement was done using a wooden height measuring board with a sliding head bar. The subjects was asked to stand straight on leveled surface with heels together and their heads positioned and eyes looking straight ahead (Frankfort plane) without shoes. Heels, Buttocks, shoulder blades should touch the vertical surface of the Studio-meter. The moving head piece of the Studio-meter was applied to lower to rest flat on the top of the head and read to the nearest 0.1cm. Weight was measures using electronic digital weight scale with light clothing and without shoes and then record to the nearest 0.1kg [13].
Dietary Diversity Score (DDS ): It was conducted consuming of lactating women within 24 hours from the nine food groups such as starch, vegetables, fruits, fish , tubers, meat, honey, milk, egg and legumes. Then the food groups are categorized into low dietary diversity (≤ 3 food groups), medium dietary diversity score who consumed four and five food groups and high dietary diversity (≥ 6) [14].
Data processing and analysis
Collected data were entered into Epi data then exported to Statistical Package for Social Sciences (SPSS) software. Descriptive statistics was used to give a clear picture of background information and determine the prevalence of under nutrition. Normality of continuous variables (anthropometric, and food groups) was checked using graphic methods. Bi-variate and multivariate logistic regressions were used to assess the association of various determinant factors of under nutrition. Multivariable logistic regression analysis was used to control the possible confounding effects of variables. In a multivariate logistic regression analysis all variables are significant at p-value of 0.25 and 95% CI in the bi-variate logistic regression was entered into the model. Variables which are significant at p-value <0.05 level and 95% CI are considered to be the determinant factors of under nutrition. Fitness of the model was check by HosmerLemeshow goodness of fit test.
Data quality assurance: Questionnaires from English was translated to Amharic and again back to English, and 5% pre- test was performed in semen bench woreda to check the validity and completeness of data collection tool before the actual data collection period. Training was given for data collectors and supervisors. Continuous and supportive supervision was given.
A total of 527 lactating mothers were involved in this study with a response rate of 96.5%.The prevalence of under nutrition among lactating mothers was 23.7% with (95%CI:18.9,28.8). Almost half, 308 (58.7%) of the respondents were in the age group of 26–35 years. The mean (± SD) age of respondents was 27.6 (± 6.2) years. Majority of 448 (85%) of the lactating mothers were married, and three fourth (27.9%) of lactating mothers were attained high school level, 136 (25.8%) lactating mothers were college and above and sixty three (12.0%) of lactating mothers were Illiterate. Around half (52.5%) of lactating mothers were Housewife’s, whereas 193(35.6%) of lactating mothers were government employees. Concerning family’s economic condition, 223(42.3%), 145(27.5%) and 159(30.2%) were found to be poor, medium and rich respectively (Table 1).
| Variables | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age category | 15-25year | 84 | 17,9 |
| 25-35 year | 308 | 58.7 | |
| ≥ 36 year | 125 | 23.4 | |
| Religion | Orthodox | 195 | 22.8 |
| Muslim | 120 | 37.0 | |
| Protestant | 156 | 29.6 | |
| Catholic | 56 | 10.6 | |
| Ethnicity | Bench | 154 | 29.2 |
| Amhara | 135 | 25.6 | |
| Oromo | 119 | 22.6 | |
| Keffa | 99 | 18.8 | |
| Others*(Hadiya.Gurage& Wolayta) | 20 | 3.8 | |
| Living arrangement | Living husband | 287 | 54.5 |
| Living with parents | 179 | 34.0 | |
| Live with friends | 61 | 11.6 | |
| Marital status | Married | 448 | 85.0 |
| Single | 79 | 15.0 | |
| Educational status of husband | Illiterate | 53 | 11.1 |
| Read and write | 86 | 16.3 | |
| Primary school | 103 | 19.5 | |
| Secondary school | 126 | 22.9 | |
| College and University | 159 | 30.2 | |
| Educational status of Mother | Illiterate | 63 | 12.0 |
| Read and write | 81 | 15.3 | |
| Primary school | 100 | 19.0 | |
| Secondary school | 147 | 27.9 | |
| College and University | 136 | 25.8 | |
| Occupation of husband | Daily labor | 39 | 10.4 |
| Farmer | 188 | 32.7 | |
| Merchant | 261 | 46.5 | |
| Government Employed | 39 | 10.4 | |
| Occupation of Mother | Housewife | 282 | 52.5 |
| Merchant | 52 | 11.9 | |
| Government Employed | 193 | 35.6 | |
| Family size | >5 | 173 | 32.8 |
| ≤ 5 | 354 | 67.2 | |
| Wealth index | Poor | 223 | 42.3 |
| Medium Rich |
145 | 27.5 | |
| 159 | 30.2 |
Table 1: Distribution of socio-demographic and economic characteristics among family of lactating mothers in Mizan Aman Town, southwest Ethiopia, 2020. (N=527).
Maternal Health Care and Feeding Practices
Regarding to dietary diversity, 371 (70.4 %) had DDS of ≥ 5 and 156 (29.6%) of lactating women had <5 DDS. Most of respondent, (73.1%) got their first pregnancy in less than 18 years old. The 348(66.0%), lactating women received antenatal care (ANC) at least once during their last pregnancy and 97 (18.4 %) of study subject had ANC visits of ≥ 4 times, from the total respondent, eighty six (16.3% of respondents had experienced illness in the past two weeks preceding the study time. Regarding to latrine availability, 367(69.6%) of the house hold uses pit latrine without slab. Regarding drinking water source, half (51.0%) of study respondents used protected spring as well as three hundred-sixtyseven (69.6%) of participant uses piped water source as a major source of drinking water (Table 2).
| Variables | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Breastfeed child age | 6-11 Month | 277 | 20.5 |
| 2-18 month | 142 | 26.9 | |
| 9-24 month | 108 | 52.6 | |
| Nutritional education | Yes | 426 | 80.8 |
| No | 101 | 19.2 | |
| Number of feeding | <3 feed | 418 | 79.3 |
| ≥ 3 feed | 109 | 20.7 | |
| Additionally food consumption | Yes | 107 | 20.3 |
| No | 420 | 79.7 | |
| Avoiding food during lactation | Yes | 147 | 27.9 |
| No | 380 | 72.1 | |
| Women dietary diversity | <5DDS | 156 | 29.6 |
| ≥ 5DDS | 371 | 70.4 | |
| House hold food security | food insecure | 87 | 18.0 |
| food secure | 397 | 82.0 | |
| Day of last menstruation seen | last 30 days | 235 | 44.6 |
| More than 30 days ago | 178 | 33.8 | |
| I didn't remember | 114 | 21.6 | |
| Age at first pregnancy | <18 years | 142 | 26.9 |
| ≥ 18 years | 385 | 73.1 | |
| Birth interval | First birth | 85 | 16.1 |
| 1-2 year | 189 | 35.9 | |
| >2 year | 253 | 48.0 | |
| Number of ANC visits | No visit | 82 | 15.6 |
| <4 visit | 348 | 66.0 | |
| ≥ 4 visit | 97 | 18.4 | |
| Place of delivery | Health facility | 117 | 77.8 |
| Home delivery | 410 | 22.2 | |
| Contraceptive use | No | 320 | 60.7 |
| Yes | 207 | 39.3 | |
| History of illness | Yes | 86 | 16.3 |
| No | 441 | 83.7 | |
| Availability of toilet | Yes | 434 | 82.4 |
| No | 93 | 17.6 | |
| Type of toilet | Ventilated improved pit latrine | 93 | 17.6 |
| Pit latrine with slab | 67 | 12.7 | |
| Pit latrine without slab | 367 | 69.6 | |
| Drinking water source | Piped water source | 176 | 33.4 |
| Protected spring | 269 | 51.0 | |
| un Protected spring | 82 | 15.6 |
Table 2: Maternal health care and feeding Practices of study participant in Mizan Aman Town, Southwest Ethiopia, 2020(n=527).
Maternal nutritional status and Knowledge
The nutritional status of lactating women was measured by Body Mass Index (BMI). Accordingly, from the total participants, 125(23.7%) had BMI of <18.5 Kg/m2 and 379 (71.9 %) were in normal range and 23(4.4%) of the participant were overweight. Regarding to nutritional knowledge, around three- fourth of lactating mothers heard about under nutrition. Fortyfive percent of lactating mothers responded that loss appetite related to illness and thirty- eight percent of lactating mothers responded that lack of nutrient in the diet or eating too little were the causes of under nutrition. Sixty -nine (33.7%) of lactating mothers responded that feeding nutrient-rich foods could be taken as the prevention methods of under nutrition (Figure 1).
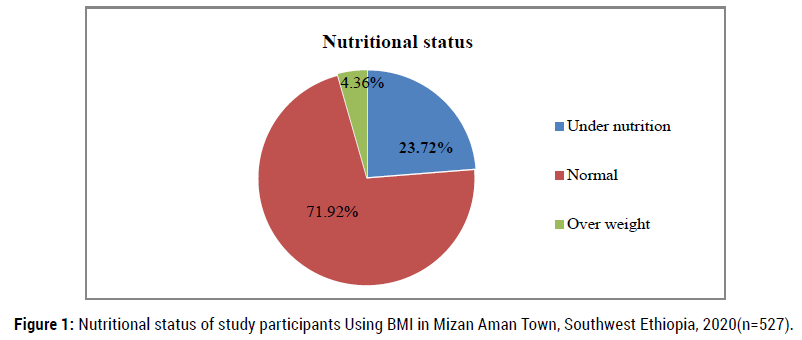
Figure 1. Nutritional status of study participants Using BMI in Mizan Aman Town, Southwest Ethiopia, 2020(n=527).
Factors associated with under nutrition among lactating mothers
There is association between nutritional status of lactating mothers and variables in bivariate analysis such as, Occupational status of husband, Education status of lactating women, Living arrangement, Family size, Place of delivery, Wealth status of family, House hold food security status, Women dietary Diversity score, Age of first pregnancy, and Birth interval. In multivariable logistic regression analysis, variables like: educational status of women, age of first pregnancy, family size and women dietary diversity were statistically significant predictors of under nutrition among lactating women in the study area. Those women who are Illiterate were seven times more likely to be undernourished than women who had collage and above [AOR=7.53CI: (1.237, 25.373)]. Those with dietary diversity score below the mean (<5) were 4.5 times more likely to be undernourished than women with the score a greater than or equal the mean (≥ 5) [AOR= 4.461 CI: (1.732, 11.492)]. Lactating women whose age of first pregnancy was less than eighteen years old were two times more likely to be undernourished than women whose age was greater than eighteen years [AOR=1.660CI: (1.321, 3.466)]. those lactating women from greater than five family member were two times more likely to be undernourished than those living with less than five family member [AOR=1.83 CI:( 1.026, 3.271)] (Table 3).
| Predictor | Category | Nutritional status | COR 95%CI | AOR 95%CI | P –value | |
|---|---|---|---|---|---|---|
| Under nutrition (%) | Normal (%) | |||||
| Occupational status of husband | Daily labor | 14(35.9) | 25(64.1) | 1.24(0.50,3.10) | 2.711(0.783, 9.380) | 0.115 |
| Farmer | 31(16.5) | 157(83.5) | 3.52(1.67,7.42)* | 9.089(2.970, 27.817) | 0.101 | |
| Merchant | 64(24.5) | 197(75.5) | 2.14(1.07,4.30)* | 7.663(2.328, 25.223) | 0.061 | |
| Employed | 16(41.0) | 23(59.0) | 1 | 1 | ||
| Education status of lactating women | Illiterate | 18(28.6) | 45 (71.4) | 1.11(0.58,2.15) * | 7.53(1.237,25.373) ** | 0.001 |
| Reade and write | 12 (14.8) | 69(85.2 ) | 2.57 (1.26,5.24) | 3.90(0.339, 11.257) | 0.103 | |
| Primary school | 17 (17.0) | 83(83.0) | 2.18(1.15,4.12) * | 3.85(0.584, 9.400) | 0.113 | |
| Secondary school | 36 (24.5) | 111(75.5) | 1.37(0.0.82,2.32) | 2.58(0.295, 5.134) | 0.107 | |
| Collage and Above | 42 (30.9) | 94(69.1) | 1 | 1 | ||
| Living arrangement | Living husband | 71(24.7) | 216(75.3) | 0.46(0.21,1.01) | 0.529(0.192, 1.457) | 0.218 |
| Living with parents | 46(25.7) | 133(74.3) | 0.68(0.19,0.98)* | 0.314(0.107, 0.919) | 0.234 | |
| Live with friends | 8(13.1) | 53(86,9) | 1 | - | ||
| Family size | >5 | 30(17.3) | 143(82.7) | 1.75(1.10,2.76)* | 1.83(1.026, 3.271)** | 0.041 |
| ≤ 5 | 95(26.8) | 259(73.2) | 1 | 1 | ||
| Place of delivery | Home delivery | 85(20.7) | 325(79.3) | 1.98(1.27,3.12)* | 1.186(0.646, 2.178) | 0.581 |
| Health institution | 40(34.2) | 77 (65.8) | 1 | |||
| Wealth Index |
Low | 75(33.6) | 148(65.4) | 0.22(0.12,0.39)* | 0.133 (0.065,1.270) | 0.105 |
| Medium | 34(23.4) | 111(76.6) | 0.36(0.19,0.69) | 0.323(0.152, 1.687) | 0.203 | |
| High | 16(10.1) | 143(89.9) | 1 | 1 | ||
| Age of first pregnancy | <18yr | 54(38.0) | 88 (62.0) | 0.36(0.24,0.56) * | 1.660(1.321, 3.466) ** | 0.000 |
| ≥18 yr | 71(18.4) | 314(81.6) | 1 | 1 | ||
| House hold food security status | Food secure | 90(22.7) | 307(77.3) | 1.89(1.15,3.11)* | 1.816(0.901, 3.660) | 0.095 |
| Food insecure | 31(35.6) | 56 (64.4) | 1 | 1 | ||
| Women dietary Diversity score | <5 | 40 (25.6) | 116(74.4) | 0.86(0.56,1.33) * | 4.461(1.732,11.492)** | 0.002 |
| ≥5 | 85(22.9) | 286(77.1) | 1 | 1 | ||
| Birth interval | first birth | 49(38.9) | 77(61.1) | 0.43(0.27,0.71)* | 0.228(0.108, 1.484) | 0.101 |
| 1-2 year | 27(15.3) | 149(84.7) | 1.54(0.92,2.58) | 1.377 (0.732, 2.590) | 0.321 | |
| >2 year | 49(21.8) | 176(78.2) | 1 | 1 | ||
Table 3: Factors associated with under nutrition among lactating women in Mizan Aman Town, Southwest Ethiopia, 2020 (n=527).
The prevalence of under nutrition was 23.7%. Education status of lactating women (Illiterate), age of first pregnancy, women dietary diversity and family size were significantly associated with under nutrition.
This prevalence was in line with studies in Tigray, 24.6 % (15) and also in Amhara region of Wombera district 25.6% (16). Similarity, studies reported in Oromia region, Adama 19.5% (17), Nekemte 20.5% (18) and Ambo district 21.5% (19). When this figure is compared with the result of Bible 41.7% (20), and Jimma 40.6% (21) it is much lower. Additionally, the prevalence is higher than studied in Indonesia 9%, (22) Tibet 10.3% (23), Myanmar 11.9% (1) and Nigeria 5% (24). The difference in the prevalence might be due to socio-demographic factors like education status of women, sample size difference and economic differences between the studies areas.
Lactating mothers who were Illiterate seven times more likely to be undernourished than those mothers who had college and above. Similar studies from India (25) and also in Ethiopia Ambo district (19) this might be related with an increased awareness of self-care, health service utilization and recognizing the importance of increasing dietary frequency at the time of lactation among educated mothers.
Age of women first pregnancy was another factor associated with under nutrition. Mothers who got pregnant before their eighteenth birthday were two times more likely to be undernourished compared to those whose age is greater than 18 years during the first pregnancy. This finding agrees with a study done in Amhara region, Womberma, and Nepal (16, 19, 26). This could be because of the immature anatomical structure and physiological conditions in younger women.
Those mothers whose dietary diversity score below the mean (< 5) were 4.5 times more likely to be undernourished than mothers with the score a greater than or equal the mean (>= 5), implying that eating diverse food groups as a protective to under nutrition. This finding supported with a study done in Dedo and Seqa, Jimma Zone (21). This might be because mothers with low dietary diversity may not get enough balanced diets which are essential for the human body to be immune and perform metabolic activities and also diversified food reflects dietary quality, improves daily nutrient and energy intake.(27).
Family size affects the intake of adequate quantity and quality of diet that in-turn contributes to maternal under nutrition. In the present study, lactating mothers from greater than five family members had two times more likely to undernourished than those mothers from less than five family members. This finding agrees with study in Ziway, Kenya and Bangladesh, which revealed that women in greater than five family members have a higher risk of under nutrition than mothers less than five family member (28, 29, 30). This may be due to, when food is in short supply; one coping strategy may be for mothers to eating less reserving more food for men and boys. Those all could be leading to lack of access to adequate, safe, and nutritious food resulting in mothers under nutrition.
The prevalence of under nutrition among lactating mothers was high prevalence. The predictors of under nutrition among lactating women were: educational status of the mothers, age of first pregnancy, dietary diversity, and family size status. Which should be required integrated governmental and NGO intervention to control the burden. Therefore it is important knowing and managing of identified determinant factors, prevention, and control of rout causes and nutrition-related problemsolving strategies is very important to control under nutrition among lactating women and they need more diversified diet and education on how and when use food.
Citation: Berhe, G.B., Atimo, A.A., & Adisu, S.E. Prevalence of Under Nutrition and Associated Factors among Lactating Mothers in Mizan Aman Town, Southwest Ethiopia, 2020. Prim Health Care, 2021, 11(10), 409.
Received: 16-Oct-2021 Published: 29-Oct-2021
Copyright: © 2021 Berhe G.B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.