Research Article - (2025) Volume 15, Issue 1
Background: Antenatal care, one of the pillars of safe motherhood, is a proven a concept aimed at reducing maternal and neonatal morbidity and mortality. It is a largely a health preventive and promotive activity. In order to foster its utilization and the desired benefits, the males who are largely key decision makers especially in patriarchal societies have to be involved. This concept of Male Involvement (MI) is essential in curtailing the gender inequality and improves the family livelihood. Although different strategies have been employed to woe males into ANC clinics, their involvement is largely lacking in Uganda. This study reports level of males’ involvement, their knowledge and attitudes of ANC and influencing factors.
Materials and methods: This was a cross sectional community descriptive study that employed quantitative and qualitative methods. Our qualitative data study was based on the phenomenological design and rooted into the grounded theory. For quantitative study, 135 adult males were recruited and collected data analyzed using SPSS software (version 24) while for qualitative data collection, Focus Group Discussions (FGDs) were held for 60 males and each transcript was analyzed by two researchers using NVIVO software version 12. Coding was done and themes developed.
Results: Male involvement as assessed based on different activities was between 51.1% and 85.2%. Although 77.8% had ever accompanied their partner for ANC, only 9.6% did so on at least 4 occasions and 88.9% never received any supplementary service during the visit. Significantly males were generally knowledgeable and had positive attitude towards ANC. Also 65.4% reported their partner felt comfortable once accompanied. However, during FGDs, males described ANC as a room for checking pregnant women, time wasting and unpleasant for the males with no privacy and rude staff. They were further wary of being tested as a couple for HIV. Despite challenges, ANC couple attendance was credited with potential of fostering unity.
Conclusions: Male involvement is improving in Uganda but more needs to be done in educating men about their importance in ANC. Couple friendly infrastructure that ensures privacy, staff training that ensures customer care tailored towards being more sensitive and responsive to couples’ may improve MI.
Male involvement • Antenatal care • Buyende • Uganda
Male Involvement (MI) is an all-encompassing term, referring to the various ways in which men relate to reproductive health problems and programs, reproductive rights and reproductive behavior. It is considered to be an important cornerstone for improving maternal health globally. It calls for the need to change men’s attitude and behavior towards women’s health, make them more supportive of women to and during use of health care services and sharing childbearing activities. Furthermore, it emphasizes that men’s understanding of their responsibility for their sexual and reproductive behavior as well as their social and family role is essential in curtailing the gender inequality and improve the family livelihood [1]
The recognition of the need to involve men in Maternal and Child Health (MCH) programmes has been realized since the mid-1990's, given the important role men have as partners/husbands, fathers and community members and as a way of promoting egalitarian decisions about reproductive and maternal health and more so in patriarchal societies [2].
Antenatal care is one of the pillars of safe motherhood: A concept aimed at reducing maternal and neonatal morbidity and mortality and to improve the maternal and neonatal health through preventive and promotive activities as well as by addressing avoidable factors that cause death during pregnancy, childbirth and postpartum period. Antenatal care in Uganda and beyond has proven to reduce mortality and is considered as a public health necessity. Moreover, male involvement is seen to improve attendance and intended results of antenatal care [3].
In 2015 during the 70th United Nations general assembly, the Millennium Development Goals (MDG) were replaced by the more robust, Sustainable Development Goals (SDG). SDG 3.1 specifically focuses on reduction of global Maternal Mortality Ratio (MMR) to less than 70 per 100 000 live births by 2030, and to have no country with MMR above 140. Yet in 2015, about 303000 women died of maternal causes and maternal mortality emerged as the second leading cause of death only bettered by human immune virus among women aged 15-49 yrs. Whereas globally the lifetime risk of dying due to maternal death is 1 in 180, Africa’s high MMR of 540 per 100000 live births coupled with high fertility levels translate into a lifetime risk of dying from maternal causes of 1 in 37. Not surprising therefore, more than 99% of maternal deaths occur in the developing world with almost half occurring in Sub-Saharan Africa (SSA) [4].
Each year, almost a third of maternal deaths worldwide are directly related to inadequate care during pregnancy. Empowering women in and increasing male involvement in sexual and reproductive health are both seen as significant strategies to reduce preventable maternal morbidity and mortality worldwide. MI does not only improve maternal outcomes but also reduces perinatal mortality and morbidity, improves successful implementation of prevention of mother to child human immune deficiency transmission, improves uptake of family planning services, increased access to postnatal and antenatal care, enhancement of healthy maternal practices such as good nutrition, improved maternal mental health, increased likelihood of contraceptive usage and allayment of stress, pain and anxiety during delivery and postpartum depression. In fact, male involvement during pregnancy and pueperium appeared to have greater benefits than male involvement during delivery in developing countries compared to the developed countries. Among the black women, paternal involvement has the capacity to prevent excess mortality by about 65-75% [5].
Studies in different parts of the world and even same country show heterogeneity regarding the level of MI its facilitators and barriers. In a study to assess determinants of male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda, 65.4% of males had attended at least one skilled antenatal care visit with factors such as knowledge of 3 or more ANC services, obtaining health information from facility health workers and if spouse had skilled attendance at last childbirth were seen as facilitators of male involvement whereas male partners intending their spouse to carry another pregnancy and living more than 5 km from a health facility were barriers to male involvement. A study in central Uganda showed an appallingly low level of male involvement with 6% of male consistently involved while 94% were inconsistently involved. A study in Ghana also found low levels of ANC involvement with only 35% of males accompanying their wives. Male involvement in antenatal care and delivery was influenced by sociodemographic (partner’s education, type of marriage, living arrangements, and number of children) and enabling/disenabling (distance to health facility, attitude of health workers, prohibitive cultural norms, unfavorable health policies, and gender roles) factors, unfriendly antenatal care environment with lack of space to accommodate the couple, longer waiting tine at ANC clinics due to administrative bureaucracy, charging of unofficial ANC extra fees by health workers, use of critical harsh language and in Nepal it was revealed that low education status, high income status ,and age above 25 years positively affected male involvement [6].
We therefore set out to study level of male’s involvement, their knowledge and attitudes of ANC services in Kidera sub-county, eastern Uganda.
Theoretical framework
In a bid to understand the subject of male involvement in ANC, we based our qualitative data study on the phenomenological design.
Grounded theory formed the basis of our study in which we presupposed that behaviors and social relationships were key to influencing men’s involvement in Antenatal Care (ANC).
The level/extent by which men feel involved coupled with their attitude and knowledge of ANC would influence their involvement.
Study setting
The study was conducted in Kidera sub-county of Buyende district. Buyende district located in eastern Uganda. It covers an area of 18,880.7 km2, a population of 158,615 males and 164,452 females giving a total of 323,067 with males to female ratio of 96:100 and density 141km2. Buyende district has 5 sub counties namely Bugaya, Buyende, Kagulu, Kidera and Nkondo. Kidera was chosen by random sampling. Kidera has six parishes namely Bukungu, Buyanja, Kasiira, Kidera, Miseru and Ntaala and has a population of males 42,100 and females 42,300 (Uganda Bureau of Statistics 2020). Kidera sub county is the only sub county with a health facility that provides Comprehensive Emergency Obstetric Care (CEMOC) services.
Study design, participants and sampling procedure
We did a community-based descriptive cross-sectional study using both quantitative and qualitative approaches between June and July 2019. Study participants were adult males (at least 18 years of age) who had had a partner or wife currently gravid and attending antenatal care or had attend ANC in the past 1 year prior to the study period and lived in Kidera sub county. Sample size was estimated using the modified Kish Leslie survey sampling formula with a 95% confidence interval (Z score on the normal distribution curve corresponding to 95% level of confidence=1.96), a precision of 5%, and an estimated proportion of male partners attending ANC of 6% [7].
Therefore sample size, N=(1.96)2 × 0.06 × 0.94/ (0.05)2=0.217/0.0025=87 participants. We however increased our sample size by 50% to increase power. Therefore, we interviewed 135 participants.
Number of services received at ANC
Whereas most women have the opportunity to interact with the health care system during ANC, most men only do so once ill. Involvement in Sexual and Reproductive Health (SRH) during ANC has been seen as a ‘doorway’ into the health care system. We asked these males about a service they had ever received from a Data management and analysishealth facility once they accompanied their partner.
Data management and analysis
For quantitative study method, we used purposive sampling to selected adult male participants were who had had a partner or wife currently gravid and attending antenatal care or had attend ANC in the past 1 year prior to the study period and lived in Kidera sub county. This was done with the help of the Village Health Team (VHT). Data was collected using semi-structured pretested face to face interviewer administered questionnaires. This data included sociodemographic, knowledge and attitude towards ANC, activities that are indicative of male involvement in their partner’s ANC services and services they had ever received at the antenatal care clinics. A 14 point knowledge scale was used to measure the respondents’ knowledge of ANC. A correct response attracted a score of 1 point while a wrong knowledge one, zero. A score of ≤ 5 points was considered poor while scores of 6-10 and 11-14 points were considered moderate and good knowledge, respectively. We used three parameters to measure the men’s attitude towards ANC. These included: Would use ANC, necessity for male partner involvement and finally partner’s comfort when escorted to the ANC clinic. After completion of quantitative data collection, each questionnaire was assigned a number in form of codes so that the questionnaire could be rechecked if the need arose. The data collected from the 135 respondents were entered into Microsoft excel processed and analyzed using SPSS software (version 24). Simple proportions were used to describe categorical data at univariate level and presented in frequency and percentage distributions [8].
For the qualitative study phenomenological study design was used. Researchers who had been trained in qualitative data collection and had not interacted with this community before the research collected data through Focus Group Discussions (FGDs). We used Village Health Team (VHT) members to help mobilize the participants. In all circumstances the VHT member introduced us and a village meeting place nearby was used. During the FGDs, participants were grouped into those for young men (below or equal to 35 years) and older man (above 35 yrs. of age). In order to freely achieve our target, we visited the recreational facilities such as football grounds for the youth and venues for social gatherings such as bars for older participants. Each FGD comprised of 5-10 men and lasted 1-1.5 hours. We held 3 FGDs for males older than 35 years and 4 FGDs for those below. The number of FGDs was determined by the saturation point.
In we approached 73 participants but only 60 consented to take part. The 13 declined on the basis of not having time. Unique numbers were then assigned to each participant to ensure anonymity. We used interview guide questions that were developed in English but translated also in Lusoga (local language) and pretested before data collection began.
Each focus group discussion group had 2 researchers. Interviews were largely carried out in Lusoga, audio recorded and field notes written in a hand book. After each Focus Group discussion, each transcript was analyzed by two researchers working independently to reduce bias using NVIVO software version 12.Coding was done manually based on the key words and phrases developed from the data. The codes were then grouped together into higher order headings. Accordingly on a higher logical level of abstractions codes, subcategories, categories and themes were formed. The themes were categorized according to the ANC as a small room for only midwife and pregnant woman, ANC as a couple serving centre, male’s role as providers, couple ANC attendance as determinant of family direction and ANC as unpleasant place. together into higher order headings. Accordingly, on a higher logical level of abstractions codes, subcategories, categories and themes were formed. The themes were categorized according to the ANC as a small room for only midwife and pregnant woman, ANC as a couple serving centre, male’s role as providers, couple ANC attendance as determinant of family direction and ANC as unpleasant place [9].
Sociodemographic characteristics
The study involved 135 males, 8.9 %( 12/135) were young men between 19 to 24 years and were 51.1 %( 69/135) were aged 35 years and above. Furthermore, majority of the participants, 71.9% (97/135) were Christians while 25.9% (35/135) were Muslims. Moreover, 98.5% (133/135) were currently staying with their female partners and of these, 94.4% (122/135) were officially married. Significant to note too, is that 94.8% (128/135) had had some formal education with 45.9% (62/135) attaining at least secondary school education and only 5.2% (7/135) had not attained any formal education.
Regarding the number of children, 75/135 (55.6%) had 0-5 children while about 5.2% (77/135) had 15 or more.
Furthermore, 99.3% (134/135) were engaged in some form of employment with the informal sector accounting for 97.1% (131/135) while 2.2% (3/135) were formally employed. (Table 1)
| Variable | Frequency (N=135) | Percentage (%) |
| Age | ||
| 19 to 24 years | 12 | 8.89 |
| 25 to 29 years | 25 | 18.5 |
| 30 to 34 years | 29 | 21.5 |
| >=35 years | 69 | 51.1 |
| Religion | ||
| Christians | 97 | 71.9 |
| Moslem | 35 | 25.9 |
| Others | 3 | 2.2 |
| Marital status | ||
| Cohabiting | 11 | 8.2 |
| Married | 122 | 90.4 |
| Divorced | 2 | 1.5 |
| Level of education | ||
| No formal education | 7 | 5.2 |
| Primary | 66 | 48.9 |
| Secondary | 58 | 43 |
| Tertiary/college | 4 | 3 |
| Occupation | ||
| Informal | 7 | 5.3 |
| Civil servant | 3 | 2.2 |
| Peasant | 77 | 57 |
| Others | 48 | 35.56 |
| Number of children | ||
| (0-5 children) | 75 | 55.56 |
| (6-10 children) | 40 | 29.63 |
| (11-15 children) | 48 | 9.63 |
| Above 15 children) | 77 | 5.19 |
| Living with partner | ||
| Yes | 133 (98.5) | |
| No | 2 (1.5) | |
| Services ever received | ||
| HIV testing | 132 (97.9) | |
| Only 1 supplementary service | 10 (7.4) | |
| More than 1 supplementary service | 5 (3.7) | |
| No service received at all | 120 (88.9) | |
| Average number of ANC | ||
| At least 4 | 13 (9.6) | |
| 3 times | 31 (23) | |
| 1-2 times | 68 (50.4) | |
| None | 23 (17) | |
Table 1. Sociodemographic characteristics of the 135 male participants.
Regarding, male involvement, no parameter measured was below 50%. Moreover, the majority, 85.2% (115/135) self-reported participating by making sure that the necessary requirements in regards to pregnancy were available. Furthermore, 77.8% reported having ever accompanied a partner to the ANC clinic while 22.2% had not. Of the 20 men that had never accompanied their partners, 30% (6/20) did not know about ANC, 25% (5/20) did not do so because they were not staying together while 45% (11/20) stated that they were too busy to accompany their partners for ANC (Figure 1).
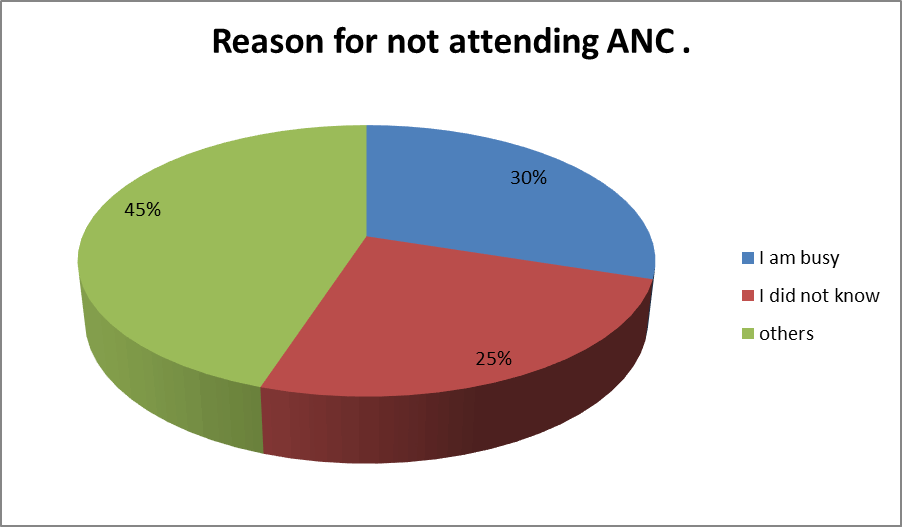
Figure 1. Reasons for males not attending ANC with partner.
Significantly, males were largely positive about ANC and thus scored over 90% for all the parameters assessed. Moreover, 95.6 % (129/135) emphasized that they would have used ANC had they been women, agree to use ANC, 95.6% (129/135) agreed it was necessary for men to get involved in ANC while 93.3% (126/135) believed that their partners would be comfortable being accompanied for the ANC. Furthermore, men were largely knowledgeable of ANC. Significantly, 8.9% scored 11-14 (Sufficient knowledge), 61.5% scored 6-10 (Moderate knowledge) while 29.6% scored 0-5 (poor knowledge) (Table 2).
| Knowledge levels scores | Number, n | Percentage, % |
| Sufficient knowledge (11-14) | 12 | 8.9 |
| Moderate knowledge (6-10) | 83 | 61.5 |
| Poor knowledge (0-5) | 40 | 29.6 |
| Would use ANC | ||
| Agree | 129 | 95.56 |
| Disagree | 2 | 1.48 |
| Neutral | 4 | 2.96 |
| Find it necessary for men to be involved | ||
| Agree | 129 | 95.56 |
| Disagree | 4 | 2.96 |
| Neutral | 2 (1.5) | |
| Partner feels comfortable when accompanied | ||
| Agree | 126 (93.3) | |
| Disagree | 5 (3.7) | |
| Neutral | 4 (3.0) | |
Table 2. Knowledge and attitudes of males towards antenatal care involvement.
Several areas were assessed to determine the level of male partner involvement in the utilization of ANC services. Also, whereas the majority of males, 83% ever attended ANC only 50.4% attended 1-2 visits and as the contacts increased there after the percentage attending declined. Noteworthy is that only 9.6% (13/135) ever attended at least 4 ANC clinics. Moreover, only 51.1% took part in the various activities at the clinic (Table 3).
Variable of male involvement |
Yes number, (%) |
N number, (%) |
 No (%) |
I accompanied her to ANC clinic |
105 (77.8) |
30 (22.2) |
30 (22.2) |
I provided her with transport to attend ANC |
81 (60.0) |
54 40) |
54 (37.8) |
I provided her with food and money to feed her during pregnancy |
107 (79.3) |
28 (20.7) |
28 (10.7) |
I brought for her the necessary requirements in regards to pregnancy for example the baby’s clothes and delivery (mama) kit |
115 (85.2) |
20 (14.8) |
20 (14.8) |
I accompanied her to the ANC clinic and took part in the various activities at the ANC clinic |
69 (51.1) |
66 (48.9) |
66 (48.9) |
Average number of ANC visits |
|||
At least 4 times |
13 (9.6) |
122 (90.4) |
|
3 times |
31 (23) |
104 (77) |
|
1-2 times |
68 (50.4) |
67 (49.6) |
|
Never attended ANC |
23 (17) |
112 (83) |
|
Table 3. Variables that define male involvement in antenatal care.
The services that were provided included taking their blood pressure, body weight, nutritional status assessment (by measuring Mid Upper Arm Circumference (MUAC)) and Human Immune Virus (HIV) testing. HIV serology testing was the major service offered to men, 97.9% (132/135). Significantly, 88.9% (120/135) never had any supplementary services provided during ANC. However, 15/135 males (1.1%) received at least a supplementary service with 3.7% (5/135) receiving more than one service (Figure2).
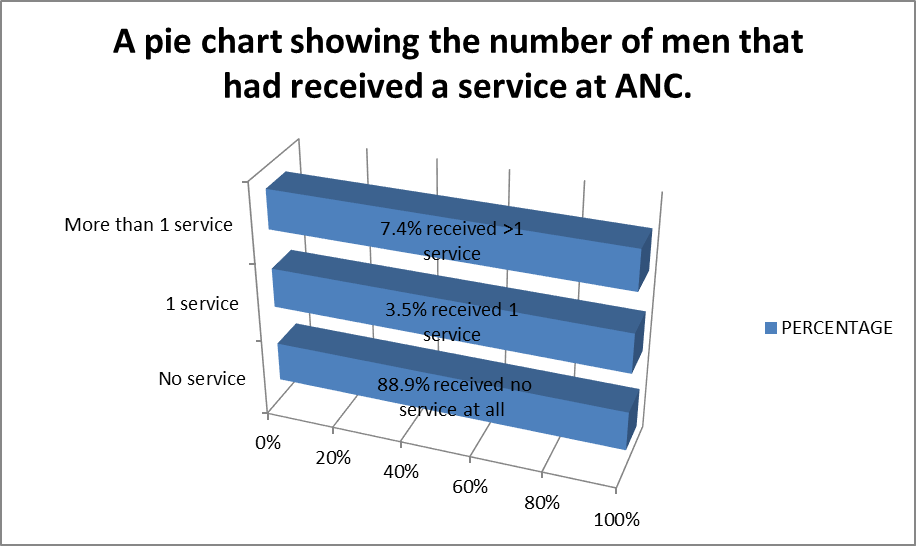
Figure 2. Percentage distribution of men who had ever received a service when they went for ANC with their spouses other than HIV testing.
Qualitative data results
This was done through a phenomenological approach with inductive thinking. Focus group discussions were used to explore what the males thought of ANC and the services provided and to understand the level of their participation using an interview guide that was specifically designed to conduct this study (Supplement).
Sociodemographic characteristics of participants
Sixty males participated in the Focus Group Discussions (FGDs). The majority of the participants were below 35 years of age 44/60 (73.3%). Moreover 75% were Christians. Significant to note, is that 93.3% tayed with partners, 91.7% were informally employed while 76.7% had either had no formal education or had only attended primary school (Table 4).
| Variable | Number, n (%) |
| Age (years) | |
| 18-24 | 5 (8.3) |
| 25-29 | 21 (35) |
| 30-34 | 18 (30) |
| 35-39 | 10 (16.7) |
| >40 | 6 (10) |
| Occupation | |
| Fishermen | 5 (8.3) |
| Peasant | 35 (58.3) |
| Boda boda cyclist | 15 (33.3) |
| Formal | 5 (8.3) |
| Level of education | |
| No formal/primary education | 46 (76.7) |
| Secondary | 12 (20) |
| Others | 2 (3.3) |
| Religion | |
| Christians | 45 (75) |
| Muslims | 14 (23.3) |
| Others | 01 (1.7) |
| Marital status | |
| Married/cohabiting | 56 (93.3) |
| Single/divorced | 04 (6.7) |
Table 4. Sociodemographic characteristics of participants in the focus group discussions.
Theme 1: ANC as a small room for only midwife and pregnant woman? Whereas they were mixed answers to what men thought ANC was, majority submitted that ANC was a small room where the midwife enters with the pregnant woman and the latter is checked.
15 males described it as a small room where the midwife takes your wife and you are told to wait from outside.
“During ANC your wife is taken into a small room and the midwives tell you to wait outside,” said a 26-year-old participant
However, 10 males described it as a room where the midwife checks the status of the baby and the mother.
“ANC is a place where you take your wife so that the midwife can check on the status of the baby and the mother.” said 25 year old respondent
Theme 2: ANC as a couple serving centre: With regards to male involvement in the ANC clinics, respondents reported that pregnant women and their spouses who were not sure of their HIV status were afraid of going together for ANC services. The respondents revealed that one of the basic services provided at the clinic during the first ANC visit was HIV counseling and testing. According to our respondents, the majority of men did not want to take HIV testing. To them, testing for HIV was soliciting for problems.
“15 participants said, they were afraid of testing for HIV status with their female partners.”
However, others appreciated it since they could get to know together and get necessary treatment.
“You are asked as a couple to test your HIV status and in case one of you is positive you are given ARVs (antiretroviral drugs)” They also reported.
“During ANC you are given health education as a couple and thereafter the wife is given some tablets to take to ensure that the baby grows well.”
Theme 3: Males’ role as providers: During the discussions, males expressed several ways in which they are involved.
“We are involved,” said 27 years’ old
“Involvement! …paused..What do you call male involvement? “All men are involved in one way or the other”, replied 35 year
“So we are involved”, said 29-year-old
“I ensure that the mother sleeps in a mosquito net,” said a 57-year old respondent
“The man should buy clothes and delivery kit,” said 42-year-old
“A man should escort the mother for ANC or provide transport in case you are busy, “said a 35-year-old
“Provide a balanced diet for the mother to make sure she is healthy’, said a 27-year-old
Theme 4: Couple ANC attendance as determinant of family direction: Majority agreed that attendance of ANC as a couple may help foster unity and build stronger family ties although others expressed fear of the end of marriage in case during HIV testing, one turned out seropositive.
“As a couple it creates unity and my wife feels really loved when I escort her.” All said,
ANC “It is a good thing because it helps us as a couple knows the status of the baby hence prepare accordingly.”
And 12 said, “In case I test positive that could be the end of our marriage.”
“It is a risky idea because of the mandatory HIV testing; we could part ways in case I turned out positive.”
Theme 5: ANC as unpleasant place: Most males decried the environment and mood at the facilities.
15 of the responses were “The mid wives are so rude; you can’t even think of going for another visit.” “You sit from 8 am till 3 pm and sometimes even 5 pm”
17 of the men said, “The men are never attended to, it’s only the women, we stay idle the entire time.”
“The midwives are so rude; you can’t even think of going for another visit.” said 36-year-old participant
“The men are never attended to, it’s only the women, we stay idle the entire time’’, 29 old said
“We are fishermen; we work during night and sell off our catch in during day so our work schedule cannot allow us to take part consistently.”
“My wife is disabled and whenever I walk with her in public I am laughed at”, said a 27-year-old
This study shows that male partner involvement in ANC is high with parameters used for assessment scoring between 51.1 (Iescorted/accompanied her to the ANC clinic and took part in the various activities at the ANC clinic) to as high as 85.2% (I brought for her the necessary requirements in regards to pregnancy for example the baby’s clothes and delivery kit (Mama Kit)). These findings are similar to a study in Tanzania that showed a high proportion of males getting involved in different antenatal activities and in Ghana by Maxwell, et al. who revealed that 67.2% scored high for male involvement while only 32.8% scored low for male involvement and in Nepal where it was reported that only 39.3% had ever accompanied their partners [10].
In our study although 77.8% (105/135) of the males had ever accompanied their partners for antenatal, only 9.6% had done so on 4 or more ANC contacts. This finding contrasted the one by Jennings, et al. in Uganda, Atuahene, et al. in Ghana and in Kyela district, Mbeya reported that only 49.7%, 8.4% and 56.9% of males accompanied their partners respectively [11,12]. However, Jennings et al study analyzed demographic and health survey data 2010-2011 from different countries while the difference in Ghana may be that it is a western African country where culture may be different to that of our study population. Moreover, the Ghananian community was largely a fishing community.
However, the findings showed 50.4% accompanied a partner to at least to one ANC contact. This is lower than that reported in a study in northern Uganda where at least 65.4% and in neighboring Tanzania in which 63% did so. Moreover, the study agreed with findings in Ghana by Atuahene, et al. in that only 8.5% of the 8.4% of those males that accompanied partners for ANC did so 4 or more times compared to our 9.6%. However, more men are involved in buying the requirements for antenatal and food for better nutrition of the expectant mother. This may be explained by the fact that while many men may consider it their responsibility to provide and support their wives during pregnancy, they may not see accompanying them to ANC as part of their obligation or responsibility. Therefore, in African setting male involvement should go beyond just escorting one partner to the ANC clinics but include aspects like support at home during pregnancy that will enhance the good health outcome of the mother and baby. This was echoed during the FGDs in which males agreed that they all supported their partner in one way or the other during pregnancy. This study, however, corroborated with findings of a study conducted in the central region of Ghana where it was reported that although men were generally involved in ANC activities at the household and community level, they were not directly involved in activities such as accompanying their partners to the ANC clinics. The authors concluded that in order to understand well the subject of MI, the matriarchal and patriarchal nature of our societies together with religious differences, educational demarcations must be taken into consideration.
In this study males were inconsistently involved in ANC just like in a study in Central Uganda. In this study only 9.6% had accompanied partners 4 or more times. In a study in central Uganda, 94% of males did not consistently take part in ANC while only 6% did. The three top reason the males gave for their inconsistence were being busy (27.4%), not being their responsibility (19.7%) and long waiting times at the facility (14.7%). In our study, the top reasons the males gave for having never attended ANC were: Being busy at 30% followed by not knowing about ANC at 25%. During the FGD, men reduced ANC to a small room where the midwife goes to check your wife and you are told to wait from outside in addition to the environment being an unpleasant place in which midwives were considered rude, characterized by long waiting hours while one was idle and not being attended to and insensitive to men with disabled partners. These findings are echoed in a studies in Ethiopia, western Kenya by Ongolly, et al., Tanzania by Peneza, et al. a cochrane review by Ditekemena, et al., and in eastern Uganda by Byamugisha, et al. and in India [13-15].
The lack of involvement in the facility activities may be evidenced by the fact that 88.9% had never received a service other than the mandatory HIV testing. HIV testing during ANC is mandatory in Uganda at the first interface with gravid mother. In a study in New Papua Guinea the involvement of men in sexual and reproductive health services and support of their wives was shown to be hampered by inappropriate services yet other studies have shown that such services are an incentive to MI. Whereas others regarded HIV testing as a unifying factor, others reasoned that it would be divisive if one turned positive. Many men expressed fear of disclosing their HIV status to their spouses as this poses a risk of family break up. Similar findings were echoed elsewhere in Uganda and Tanzania [16].
This notwithstanding, services such as testing for HIV need to be better packaged to make them more acceptable to the couple. In our FGDs, several males branded HIV testing as a cause of trouble in most families.
Furthermore, some males believe that ANC is a female’s place.”ANC is a place where you take your wife so that the midwife can check on the status of the baby and the mother.” said 25 year old respondent. This finding has been supported by studies in Moshi ,Tanzania[49] and in South Africa[50].This clearly shows that some men have not yet realized a reason as to why they should attend ANC with spouses.
Moreover, in this study men complain about long waiting hours caused by the burdensome administrative procedures: A deterrent especially for the employed male partners is in tandem with findings elsewhere. In a study South Africa, males proposed use of weekends and early morning hours as the better times for ANC. Research has proven a correlation between the average number of visits attended per child and the occupation of the male partner as evidenced by the fact that more peasants showed up compared to the business men who said they are always busy and others claimed that the kind of work they engage in can only allow them to be free during night when it is unfavorable to attend ANC.
Men acknowledged that attending ANC together may determine family direction. Males generally had good attitude towards ANC as 95.6%agreed not only to use the service but also agreed that it was important to involve males. This is in agreement with a study in India where 96% of male respondents agreed that ANC was valuable that they would utilize the service. Moreover, males scored well on knowledge. The majority knew that ANC was very important for the pregnant woman, as it ensures the well-being of the mother and the child. This finding was similar to one found by Yargawa et al. [17].
Majority, 67.4% of the men strongly agreed that their partners felt very comfortable and loved whenever they escorted them to the clinic and this prompted them to further engage in the practice. This is supported by findings in a study in northern Uganda in which 96% of the males thought attending spousal ANC was beneficial while in South Africa 92% of the women expressed willingness to have their partners attend ANC with them [18]. During the FGD, males appreciated that ANC is a couple service centre and they appreciated services extended such as HIV testing, care services and treatment services This finding was similar to findings of other studies in East Africa [19]. However, studies elsewhere have indicated that women are uncomfortable with their male partners accompanying them as ANC clinics are considered female places and males’ presence limits free expression and honesty [20].
In terms of medication during pregnancy, the respondent’s knowledge was poor. Most men didn’t know that pregnant women receive Tetanus vaccine during pregnancy. Knowledge of services received at the ANC was equally good. Much as a study in Kenya revealed that most men were less knowledgeable about HIV prevention in regards to ANC, this study showed that high percentage of the men 96.7% knew that HIV testing was important for the health of the mother and the unborn baby and an unborn baby can be prevented from getting HIV from its mother if its mother is HIV positive. This finding supports the evidence that increasing male partner's knowledge of safe motherhood is positively associated with attendance of ANC.
From this study, males are generally involved in ANC although inconsistently. They have moderate knowledge and a good attitude towards ANC however their consistent involvement in ANC is still low as evidenced by low 4+ ANC attendances. The major barriers cited are infrastructural challenges, poor attitude and disrespectful language directed towards them by health workers, longer waiting time and the limited service package for men that only emphasizes themandatory HIV testing for couples. Heavy investment into infrastructure, human resources (in terms of numbers and improved conduct) and broadening the service package for men (such as including random blood sugar testing, nutritional assessment et cetera) will be handy in improving male involvement.
In order to promote male involvement in ANC and to address the barriers to their participation, the following strategies were recommended:
An active role of educating men on the importance of their involvement in ANC by all stakeholders needs to be undertaken.
The need for the midwives, physicians and other stakeholders maternal, neonatal and child health sector should be proactive in advocating for infrastructure and human resource investments that are accommodative of men, disabled clients and use of non judgmental, client-friendly language should be emphasized since men are key shareholders in women’s and children’s health. On the other hand, the ministry of health should invest in better infrastructure-with future designs of health facilities could be made more couple-friendly, that guarantees all clients their privacy at the clinic during service delivery and as they wait for their services. Also, there will be the need for better planning and the institutionalization of and sticking to booking/appointment regime and instituting a functional referral system-currently absent in most public health facilities in Uganda-in a bid to reduce queues and long waiting times before care is received. Lastly, the government should come up with policies that are all-inclusive and involve men as key stakeholders Sexual and Reproductive Health (SRH), introduce male tailored services to reduce on male redundancy during ANC and consider extending ANC services to weekends.
Ethical clearance was obtained from the department of Community Education Research and Services (COBERS). Informed written consent was obtained from each participant. For purposes of confidentiality, interviews were held in privacy and codes rather than names of participants.
The authors extend their gratitude to the department of community and public health, faculty of health sciences, Busitema University, Community Based Education and Research Services (COBERS) coordinator and Directorate of Graduate Studies, Research and Innovations, Busitema University, Buyende district health workers and respondents who participated on this study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Nteziyaremye J, et al. "Male Partner Involvement in the Utilization of Antenatal Care Services in Kidera, Buyende District, Uganda: A Cross-Sectional Mixed Methods Study". Primary Health Care: Open Access, 2025, 15(1), 1-9.
Received: 10-Jan-2024, Manuscript No. JPHC-24-124882; Editor assigned: 12-Jan-2024, Pre QC No. JPHC-24-124882 (PQ); Reviewed: 26-Jan-2024, QC No. JPHC-24-124882; Revised: 19-Feb-2025, Manuscript No. JPHC-24-124882 (R); Published: 26-Feb-2025, DOI: 10.35248/2167-1079.25.15(1).494
Copyright: © 2025 Nteziyaremye J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.