Research Article - (2023) Volume 12, Issue 1
Background: Percutaneous radiofrequency nucleoplasty is a true minimally invasive technique for treatment for radiculopathy caused by contained disc protrusions. This minimally invasive procedure uses termocoblation technology for coagulating and ablation the intervertebral disc to reduce pressure on a compressed nerve.
Methods: Our study is a prospective analysis conducted of 27 patients aged from 30 years to 64 years, with lumbar disc protrusion who were treated with percutaneous radiofrequency disc decompression from May 2018 to May 2019. Clinical follow up was done at 1 month, 3 months and 6 months. The outcomes were assessed using a Visual Analogue Scale (VAS) and MacNab criteria.
Results: Of all 27 patients, 14 were women and 13 were men and their mean age was 53 years ± 2 years. In all 27 patients percutaneous radiofrequency nucleotomy was performed. An excellent outcome in terms of the MacNab criteria was observed in 17 patients (63%), a good outcome in 8 patients (29.7%) and a poor outcome in 2 patients (7.3%). Preinterventionaly the back and leg VAS scores were 7.95 and 7.82 and on sixth month the back and leg VAS scores were 3.17 and 3.04. Patients with a poor outcome developed early recurrent disc prolapse and this cases required revision surgery.
Conclusion: Percutaneus radiofrequency nucleoplasty, as part of minimally invasive procedures, is effective and safe method for the treatment of disc protrusion, and it is a good alternative to surgery. These procedures significantly increase quality of life of patiens with lumbar radiculopathy.
Percutaneous disc decompression • Nucleotomy • Laser disc decompression • Resonance imaging • Radio frequency
Lumbar back pain is a big socio economic problem. Most usual cause of lumbar back pain and radiculopathy are disc herniations. Patients may also develop neurological deficit of the lower limbs or cauda equina syndrome. Protrusions of the intervertebral disc as contained disc herniation can be confirmed by Magnetic Resonance Imaging (MRI) of the spine. Management in patients with contained disc protrusions is mostly conservative which includes analgesics, physical therapy and psychotherapy [1].
Percutaneous Radiofrequency Disc Decompression (PRFD) is a true minimally invasive technique for treatment for radiculopathy caused by contained disc protrusions. This minimally invasive procedure uses termocoblation technology for coagulating and ablation the intervertebral disc to reduce pressure on an inflamated and compressed nerve. The effect is that intradiscal and nerve root pressure is significantly reduced [2].
For presented study a prospective design was done on 27 patients with lumbar disc herniation who underwent PRFD from May 2018 to May 2019. All participants sign and completed the informed consent. After neurosurgical examination and MRI verification of contained lumbar disc protrusion, they have been introduced for PRFD. There were 13 males and 14 females patients aged from 30 years to 64 years. All patients presented with clinically symptomatic disc herniation with significant radicular symptoms (mean Lasagne sign was 40 degrees). The indication for PRFD was defined through neurosurgical standards based on existing radicular symptoms with or without neurological deficit. Fifteen (15) operations were performed at the level of L5/S1, 24 on L4/5 disc level in local anesthesia (Table 1) [3].
| Age | 53 ± 2 | |
|---|---|---|
| Gender | Male | 13 (48.1%) |
| Female | 14 (51.9%) | |
| Types of DH | Protrusion | 27 (100%) |
| Lesion level | L5-S1 | 5 (18.5%) |
| L4-L5 | 24 (81.5%) | |
| Lazarevic/Lasegue (degrees) | 40 | |
| GMS<4 | 9 (33.4%) | |
Table 1. Descriptive variables.
Clinical follow up was done at 1 month, 3 months and 6 months. The outcomes were assessed using a Visual Analogue Scale (VAS) and the MacNab criteria [4].
Inclusion criteria
• The diagnosis of LDH confirmed by magnetic resonance imaging and clinical examinations.
• Patients aged from 30 years to 64 years.
• Unilateral radiculopathy unresponsive to conservative therapy for 3 months.
• Patients were willing to accept PRFD.
Exclusion criteria
• Spinal mechanical instability, spondylolisthesis or congenital deformity.
• Infection, trauma, hemorrhagic disorders, mental diseases.
• Patients refusing the PRFD.
Technique was performed under local endotracheal anesthesia. All patients received antibiotic prophylaxis (2 g Azaran) before PRFD. The level of lesion was identified with guidance of fluoroscopy. The interventions were performed with needle placed in intervertebral space and use of ABRO radiofrequency termocoblator [5].
Of all 27 patients, 14 were women and 13 were men and their mean age was 53 years ± 2 years. In all 27 patients PRFD was performed. An excellent outcome in terms of the MacNab criteria was observed in 17 patients (63%), a good outcome in 8 patients (29.7%) and a poor outcome in 2 patients (7.3%). Patients with a poor outcome developed early recurrent disc prolapse and this cases required revision surgery (Table 2).
| MacNab outcome | |
|---|---|
| Excellent | 17 (63%) |
| Good | 8 (29.7) |
| Poor | 2 (7.3) |
Table 2. MacNab outcome.
Preinterventionaly the back and leg VAS scores were 7.95 and 7.82. After PRFD, the VAS scores for the back and leg decreased significantly in both groups. Postinterventionaly, the back and leg VAS scores were 4.1 and 3.43 first month, 3.21 and 3.21 third months and 3.17 and 3.04 on sixth months (Figure 1) [6].
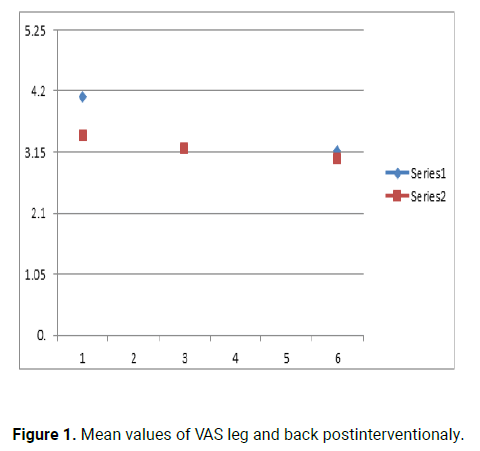
Figure 1: Mean values of VAS leg and back postinterventionaly.
Six patients complained of synesthesia on the poster lateral thigh, which spontaneously improved month after PRFD. Nerve injury and spondylodiscitis was not present as complication. There were no serious complications like cauda equine syndrome or postoperative thrombosis in our group of patients. Patients with a poor outcome developed early recurrent disc prolapse and this case required revision surgery (full endoscopic discectomy) (Figures 2-4) [7].
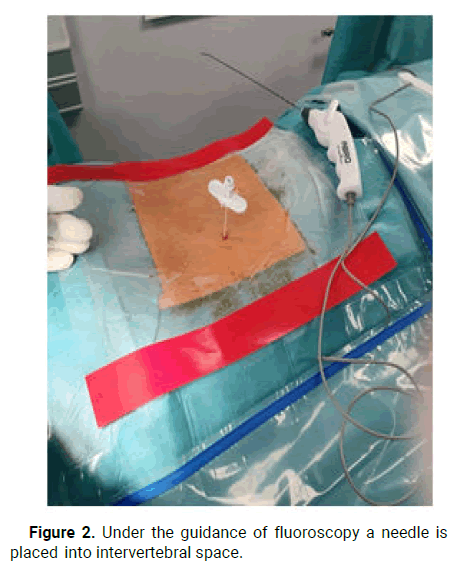
Figure 2: Under the guidance of fluoroscopy a needle is placed into intervertebral space.
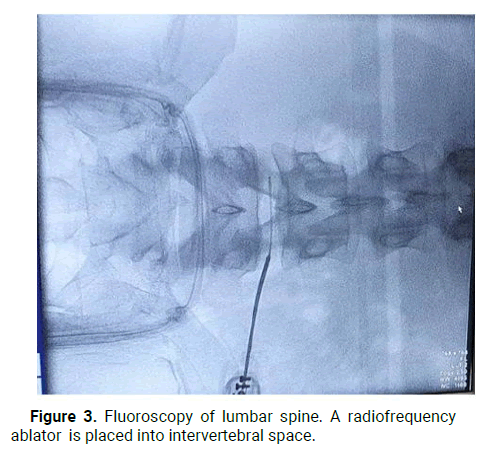
Figure 3: Fluoroscopy of lumbar spine. A radiofrequency ablator is placed into intervertebral space.
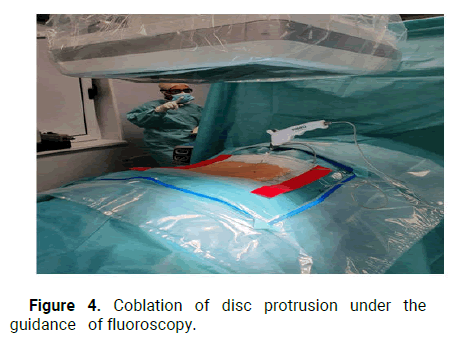
Figure 4: Coblation of disc protrusion under the guidance of fluoroscopy.
The usual cause of radiculopathy and low back pain are contained disc protrusions of the intervertebral discs. The spinal disc pressure nerve root and causes back pain or sciatic pain. Protrusion of the intervertebral disc can be diagnosed with magnetic resonance imaging of lumbar spine. Tendency to shift from operative treatment of disc herniation to non-operative minimal invasive techniques are increasing over the last decade. If conservative treatment failed after six weeks, neurosurgeon should consider doing one of minimal invasive intradiscal procedures. Percutaneous radiofrequency disc nucleoplasty is minimally invasive technique to reduce the volume of protrusion of herniated disc. Internationally, more than 200,000 patients have already been treated with nucleoplasty; with an international success rate was greater than 80% in more than 200,000 patients treated with PRFD [8].
Gerges, et al. reported VAS scores in published nucleoplasty studies and found the highest recovery rate in the study of Mirzai, et al. as 72%. In a one year follow up study, Mirzai, et al. presented the nucleoplasty results of 52 patients and found a decrease in VAS score from 7.5 to 2.1 in the twelfth month. In our prospective analysis of 27 patients who underwent PRFD nucleoplasty, there was a significant difference in VAS and MacNab pretreatment and post-treatment scores. Our prospective study of 27 patients showed a decrease in VAS score, after 1, 3 and 6 months. Preinterventionaly the back and leg VAS scores were 7.95 and 7.82 and on sixth month the back and leg VAS scores were 3.17 and 3.04 [9].
This prospective study performed at the Atlas clinic, found results for the use of percutaneous nucleoplasty with radiofrequency for the treatment of contained disc protrusions, very similar to results obtained in Germany and the United States by doctors Sebastian Ruetten, Chiu and Yeung. An excellent outcome in terms of the MacNab criteria was observed in 17 patients (63%), a good outcome in 8 patients (29.7%) and a poor outcome in 2 patients (7.3%). Patients with a poor outcome developed early recurrent disc prolapse and this cases required revision surgery. This study also demonstrated immediate reduction of radicular or low back pain, good clinical response, absence of intraoperative bleeding and short hospital stay. This study has several limitations such as the relatively small sample size. Big series are needed for future investigation of PRFD effectiveness [10].
The usual cause of radiculopathy and low back pain are contained disc protrusions of the intervertebral discs. The spinal disc pressure nerve root and causes back pain or sciatic pain. Protrusion of the intervertebral disc can be diagnosed with magnetic resonance imaging of lumbar spine. Tendency to shift from operative treatment of disc herniation to non-operative minimal invasive techniques are increasing over the last decade. If conservative treatment failed after six weeks, neurosurgeon should consider doing one of minimal invasive intradiscal procedures. Percutaneous radiofrequency disc nucleoplasty is minimally invasive technique to reduce the volume of protrusion of herniated disc. Internationally, more than 200,000 patients have already been treated with nucleoplasty; with an international success rate was greater than 80% in more than 200,000 patients treated with PRFD [8].
Gerges, et al. reported VAS scores in published nucleoplasty studies and found the highest recovery rate in the study of Mirzai, et al. as 72%. In a one year follow up study, Mirzai, et al. presented the nucleoplasty results of 52 patients and found a decrease in VAS score from 7.5 to 2.1 in the twelfth month. In our prospective analysis of 27 patients who underwent PRFD nucleoplasty, there was a significant difference in VAS and MacNab pretreatment and post-treatment scores. Our prospective study of 27 patients showed a decrease in VAS score, after 1, 3 and 6 months. Preinterventionaly the back and leg VAS scores were 7.95 and 7.82 and on sixth month the back and leg VAS scores were 3.17 and 3.04 [9].
This prospective study performed at the Atlas clinic, found results for the use of percutaneous nucleoplasty with radiofrequency for the treatment of contained disc protrusions, very similar to results obtained in Germany and the United States by doctors Sebastian Ruetten, Chiu and Yeung. An excellent outcome in terms of the MacNab criteria was observed in 17 patients (63%), a good outcome in 8 patients (29.7%) and a poor outcome in 2 patients (7.3%). Patients with a poor outcome developed early recurrent disc prolapse and this cases required revision surgery. This study also demonstrated immediate reduction of radicular or low back pain, good clinical response, absence of intraoperative bleeding and short hospital stay. This study has several limitations such as the relatively small sample size. Big series are needed for future investigation of PRFD effectiveness [10].
Percutaneus radiofrequency nucleoplasty, as part of minimally invasive procedures, is effective and safe method for the treatment of disc protrusion and it is a good alternative to surgery. These procedures significantly increase quality of life of patients with lumbar radiculopathy.
Citation: Zivkovic N, et al. "Percutaneous Radiofrequency Disc Decompression (PRFD): A Study of 27 Patients". J Arthritis, 2023, 12(1), 1-3.
Received: 01-Nov-2022, Manuscript No. JAHS-22-78757; Editor assigned: 03-Nov-2022, Pre QC No. JAHS-22-78757 (PQ); Reviewed: 17-Nov-2022, QC No. JAHS-22-78757; Revised: 20-Jan-2023, Manuscript No. JAHS-22-78757 (R); Published: 27-Jan-2023, DOI: 10.35248/2167-7921.23.12.1.103
Copyright: © 2023 Zivkovic N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.