Research Article - (2021) Volume 10, Issue 10
Introduction: Osteoarthritis (OA) represents a failure of the diarthrodial, synovial lined joints. It is a degenerative non-inflammatory joint disease. Osteoarthritis is the leading cause of chronic disability, affecting more than 80% of the human population above 55 years. It is due to an imbalance between the destructive and reparative processes involved in repairing and regenerating articular cartilage in the synovial joints. Many options for management of early OA knee are already established in previous literature. Autologous PRP injection in knee joint is an early method of management of early OA knee. The Supra-physiological release of platelet-derived growth factors directly at the site of diseased cartilage may stimulate the natural regenerative signaling cascade and enhance the healing of tissue with further mediation of the anti- inflammatory response. We did autologous PRP injection in knee joint and assessed for its long term outcome and also documented any complications after PRP injection.
Aim: To evaluate the effectiveness of Platelet Rich Plasma in the treatment of patients presenting with primary osteoarthritis of the knee joint in reducing pain and improving physical function. To document the side effects of PRP intraarticular injection and its long term outcome.
Materials and methods: patients with primary OA knee (Alhback score 1-2) received intraarticular PRP injection. Patients were assessed on variables, namely-stiffness and physical function using the WOMAC scale and pain using the Visual Analog Scale (VAS). Knee cap and tablet Paracetamol (for pain relief as required) were advised to the patients following the procedure.
Results: In final (6 months) follow-ups, we found significant improvement in both WOMAC score and VAS score after PRP injection in the knee joint. We also observed that four patients (12.5%) among the participants developed inflammatory reactions, like redness around the knee joint, intolerable pain not responding to the paracetamol, joint effusion, etc., in the knee joint intra-articular PRP was injected. Two patients developed mild inflammation which was treated with oral medication in out-patient basis. Another two patients developed moderate to severe inflammation which warranted surgical intervention. One patient was undergone arthrocentesis and other was undergone arthrotomy. Synovial fluid analysis was sterile, with increased inflammatory markers. Long term follow-up for those four patients were also satisfactory.
Conclusion: We found significant improvement in the final (6 months) of follow-ups after intraarticular PRP injection for the treatment of early OA. Four patients developed inflammatory reaction after injection. Though we found some early inflammatory reaction after PRP injection, we feel that this management line is safe and satisfactory for early arthritis of the knee joint.
Osteoarthritis • OA knee • Patients • Anti-inflammatory response
Osteoarthritis (OA) represents a failure of the diarthrodial, synovial lined joints. It is a degenerative non-inflammatory joint disease. Osteoarthritis is the leading cause of chronic disability, affecting more than 80% of the human population above 55 years. Symptomatic OA of the knee joint has a prevalence of around 22% to 39% in India. OA is a multifactorial entity, encompassing multiple contributory causative factors like trauma, mechanical force, biochemical reactions, and metabolic derangements in the body [1]. Osteoarthritis is due to an imbalance between the destructive and reparative or synthetic processes involved in repairing and regenerating articular cartilage in the synovial joints. Knee osteoarthritis is divided into two types, primary and secondary. In Primary OA, articular degenerate without any apparent underlying cause. Secondary OA is the consequence of any underlying pathology, such as trauma, rheumatoid arthritis. However, the source of pain is mainly derived from changes in the non-cartilaginous components of the joint, such as the joint capsule, synovium, subchondral bone, ligaments, and peri- articular muscles. Even though OA is a non-inflammatory entity, the synovial fluid has been found to contain multiple inflammatory mediators including plasma proteins like Prostaglandins (PGE2), Leukotrienes (LKB4), Cytokines (TNF, IL1β, IL6, IL15, IL17, IL18, IL21), growth factors (TGFβ, FGFs, VEGF, NGF), Nitric oxide, and Complement components [2].
Several treatment options are there for early OA knee, in the form of-rest, cold compression using ice, bracing, NSAIDs, intra-articular corticosteroid injection, Intra-Articular Hyaluronic Acid (IAHA) instillation, and intra-articular Platelet-Rich Plasma (PRP) injection. Platelet-rich plasma is a fraction of whole blood containing concentrated growth factors and proteins and has a higher concentration of platelets than whole blood. Connective tissue healing takes place in three phases: inflammation, proliferation, and remodeling. The unique combination and concentration of bioactive molecules within PRP profoundly affect the inflammatory, proliferative, and remodeling phases of wound healing [3]. Growth factors in PRP (PDGF, IGF, VEGF) promote matrix synthesis, cell growth, and migration, facilitating protein transcription. The Supra-physiological release of platelet-derived growth factors directly at the site of diseased cartilage may stimulate the natural regenerative signaling cascade and enhance the healing of tissue with further mediation of the anti- inflammatory response. PRP has some advantages, like autologous, natural, safe, and activates a normal healing process. In a clinical update by Cook et al., they have suggested that PRP should be the first choice to manage early OA knee. Several studies regarding PRP injection in the management of OA knee support this without any documented complications of PRP at the knee joint. At present few uncertainties still remain regarding the most suitable regimen for the most favorable outcome. Major complications like infections and allergies are reported to be very low although post-injection pain is slightly higher than with other intra-articular therapies for the OA knee.
With an increase in the life expectancy and obesity, occurrence of OA of the knee joint is also expected to rise, in such scenarios, newer and lesser invasive treatments like Intra-articular PRP injection if proven to be beneficial will be of significant importance. Further improvisation can be done in the therapy modality my combining PRP with other modes like Intra-articular Hyaluronic acid injection in order to benefit from the additive benefits of both, though some studies claim the added benefit, further research can be done in this field as well. In the current scenario, the PRP use and application along with standardization of treatment is yet to show its full efficacy and its full potential is yet to be determined. In order to have a more comprehensive modus operandi of PRP use, clinical studies like the one described here are needed [4].
The patients presented to OPD of the Department of Orthopaedics AIIMS, Raipur, between December 2019 to December 2020 with complaints of knee pain. They were screened both clinically and radiologically. Patients more than 40 years of age, with primary OA knee, grade 1-3 on the Ahlback scale, and those who gave consent to participate in the study following explanation regarding nature of treatment and need for follow up were included. Patients with secondary OA knee, history of intra-articular steroid injection in the same knee, and hemoglobin less than 10 mg/dl were excluded from the study. A total of 36 patients were enrolled in the study. 5-6 ml of Autologous platelet-rich plasma provided by the Department of Transfusion Medicine at AIIMS Raipur was injected intra-articularly into the affected knee. Patients were assessed on variables, namely-stiffness and physical function using the WOMAC scale and pain using the Visual Analog Scale (VAS). Knee cap and tablet Paracetamol (for pain relief as required) were advised to the patients following the procedure.
In our study, a total of 36 patients were enrolled with fulfilling inclusion and exclusion criteria. But we have lost the follow-up of 4 patients. Final statistical analysis on WOMAC and VAS score was done on 32 patients.
In our study, the mean age of the patients was 60.5 years, and Females had more predilection of OA knee than males. There wasn’t any specific side predilection for osteoarthritis of the knee joint. In final (6 months) follow-ups, we found significant improvement in both WOMAC score and VAS score after PRP injection in the knee joint. We also observed that four patients (12.5%) among the participants developed inflammatory reactions, like redness around the knee joint, intolerable pain not responding to the paracetamol, joint effusion, etc., in the knee joint intra-articular PRP was injected. Out of four knees with post-procedure inflammation, two had a mild reaction relieved by rest, ice pack application, oral analgesics (Aceclofenac), and prophylactic oral antibiotic. The other two patients developed severe inflammation and needed admission for supportive intravenous medications (I.V. analgesics, fluids, ice pack application) and further observation. One patient Out of the severe inflammatory reaction group needed arthrocentesis and was discharged following a 7 day admission period with subsidence of inflammation. Another patient with severe inflammation had persistent pain and effusion in the knee. Knee arthrotomy and debridement was done. The culture of the synovial fluid for both the severe knee were sterile. After 2 weeks of supportive treatment patient recovered. Final outcome of all four patients was satisfactory (Figure 1 and Tables 1-3).
| Score | Pre-injection | 6 weeks | 3 months | 6 months |
|---|---|---|---|---|
| <30 | 0 | 4 | 24 | 20 |
| 30-50 | 12 | 12 | 6 | 12 |
| >50 | 20 | 16 | 2 | 0 |
Table 1. WOMAC [Western Ontario and Mcmaster Universities] score.
| Score | Pre-injection | 6 weeks | 3 months | 6 months |
|---|---|---|---|---|
| 0-3 | 0 | 8 | 22 | 20 |
| 44350 | 12 | 18 | 6 | 10 |
| 44475 | 20 | 6 | 4 | 2 |
Table 2. Visual Analog Scale (VAS).
| Total patients | Mild inflammation | Moderate-severe inflammation |
|---|---|---|
| 32 | 2 | 2 |
Table 3. Patients developed inflammatory reactions post-injection.
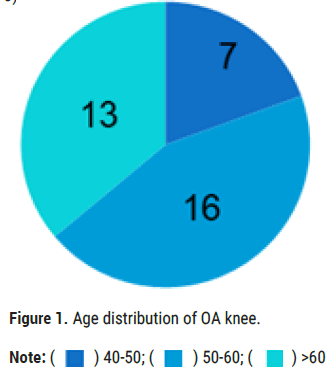
Figure 1: Age distribution of OA knee.
Osteoarthritis knee is a degenerative joint disease where several inflammatory markers have been found in the synovial membrane of the knee joint. Several treatment options are there for early OA knee, like- rest, ice, brace, NSAIDs, intra-articular corticosteroid, Intra-Articular Hyaluronic Acid (IAHA). Growth factors in activated PRP help to resolve inflammation in early OA Our study injected 5-6 ml of autologous PRP in the knee joint and assessed the outcome in WOMAC score and VAS score. In 6 months follow-up, both WOMAC score and VAS score showed significant improvement after PRP injection [5]. We have found that four patients developed early inflammatory reactions in knee after PRP injection. Two patients (6.25%) had mild inflammation, and two patients (6.25%) had a moderate-severe inflammatory reaction.
Many studies have reported satisfactory results with intraarticular injection of PRP for OA knee. Most of these studies report no or only mild adverse events following PRP injection that is usually self-limiting. Taniguchi et al. in a clinical trial for intra-articular PRP injection for the treatment of OA knee, observed only minor adverse events in 73% of patients, but all symptoms resolved within 48 hours. In a randomized clinical trial between PRP and Hyaluronic Acid (H.A.), Sanchez et al found the incidence of mild adverse events to be similar between the two groups and limiting to 48 hours. In another randomized controlled trial comparing PRP and HA, Filardo et al. observed a higher incidence of minor reactions such as pain following injection in PRP group than H.A. group. They considered proteases and reactive oxygen released from WBCs as the cause of acute reaction following PRP. In our study out of 36 patients 2 patients had mild inflammatory reaction and 2 patients had moderate to severe reaction. In the later 2 cases synovial fluid analysis yielded no growth after culture excluding any infective etiology.
Patel et al reported acute adverse events such as dizziness, syncope, tachycardia, headache, and nausea at the time of injection, but none too severe to cause concern. We have not found such adverse events in our study but keeping the patient under observation following intraarticular injection is recommended. All these studies report that the adverse events, if any subside within days and do not have any long term effect on the final outcome. Our study also supports this observation as all 4 patients had good functional outcomes at 6 months follow up.
Our study shows significant improvement in the final (6 months) of followups after PRP injection in the knee joint in WOMAC score as well as VAS score. PRP injection at knee joint for osteoarthritis is a good procedure for the treatment of early OA knee. We have found severe inflammatory reaction after injection in few patients, out of which one patient need arthrocentesis and other need surgical intervention. But final outcome was satisfactory for all patients. Though we found some early inflammatory reaction after PRP injection, we feel that this management line is safe and satisfactory for early arthritis of the knee joint. The study needs long-term follow-ups and more patients to conclude the efficacy of PRP to treat early OA knee. We didn’t have a regulatory system to measure the type and number of activated platelets in PRP, affecting the outcome after PRP injection.
Citation: Nayak B, et al. “Evaluation of Outcome of Intraarticular PRP Injection in Osteoarthritis Knee”. J Arthritis, 2021, 10(10), 001-003.
Received: 08-Oct-2021 Published: 29-Oct-2021
Copyright: © 2021 Nayak B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.