Journal of Multiple Sclerosis
ISSN - 2376-0389NLM - 101654564
Case Report - (2021) Volume 8, Issue 10
Background: Patients with rheumatoid arthritis (RA) may have central nerve system (CNS) comorbidities such us demyelinating lesions. In current practice, this clinical situation raises an etiological problem of this demyelination; is it linked to treatments; anti TNF drugs, which is the most frequent case? or is it a primary demyelination of the CNS?.
Case report: We reported the case of a 52-year-old woman followed for seronegative Rheumatoid arthritis (RA) treated with methotrexate that presented clinical and radiological multifocal inflammatory demyelinating lesions. No etiology related to RA or its treatment could explain the radioclinical presentation of the patient. Magnetic resonance imaging lesions fulfilling MC Donald’s criteria for Multiple Sclerosis (MS) and analysis of cerebrospinal fluid showed intrathecal synthesis of oligoclonal IgG band (OCB). All the difficulty of this medical condition lies in the etiological assessment. The diagnosis of primary demyelination, specifically multiple sclerosis associated with RA, was retained.
Conclusions: Certainly it is an infrequent case associating MS and RA in the absence of anti-TNF treatment which makes the originality of our case.
Rheumatoid Arthritis • Multiple Sclerosis • Demyelination • Case report
Patients with Rheumatoid Arthritis (RA) may have Central Nerve System (CNS) comorbidities such us demyelinating lesions. In current practice, this clinical situation raises an etiological problem of this demyelination (1). Is it linked to treatment with anti TNF or other drugs, which is the most frequent case? or is it a primary demyelination of the CNS?.
A 52-year-old woman followed since the age of 37 years for seronegative Rheumatoid Arthritis (RA). She was initially treated with corticoid and methotrexate and achieved remission. 2 years ago, she suffered from recurrent symptomatology associating weakness of the lower limbs, dizziness, paresthesia of the face as well as progressive numbness of the lower limbs. Neurological examination showed paraparesis with a muscle strength rated at 3 for each muscle of the 2 lower limbs and minimal motor deficit in the upper left limb with muscle strength at 3 for each muscle. The Medical Research council scale (MRC scale) was at 45. She had sharp osteotendinous reflex in 4 limbs and central vestibular syndrome. No extraneurological signs were found except those related to her RA (Arthralgia with morning joint stiffness). Cerebral Magnetic Resonance Imaging (MRI) revealed several hyperintense FLAIR signals in the periventricular and sub-cortical white matter with gadolinium enhancement of one lesion (Figure 1). Medullary MRI also showed hyperintensities on T2 images in cervical and dorsal lateral spinal cord (Figure 2), which were not enhanced by gadolinium. She underwent several investigations including Serological studies for Lyme, Human immunodeficiency virus, Hepatitis and Syphilis that were negative. Immunological assessment containing Rheumatoid Factor (RF), antinuclear antibody, anti- NMO antibodies were also within the normal range. Cerebrospinal Fluid examination (CSF) revealed normal cytology and biochemistry, but evidenced of oligoclonal IgG band (OCB) with IgG index at 1, 36. Visual evoked potentials were normal. According to The Mc Donald’s criteria 2017, the diagnosis of Multiple Sclerosis (MS) was made. The patient was treated with highdose of intravenous methylprednisolone (1g/day IV during 5 days) with good improvement of neurological symptoms. The Methotrexate was stopped after mutual agreement between neurologist and rheumatologist because of the remission of RA in our case and immunomodulatory drug (Interferon-beta-1b) was initiated.
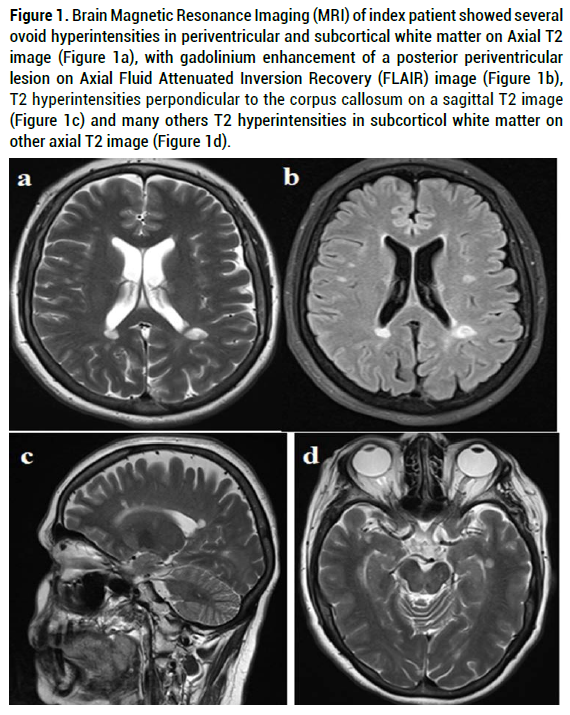
Figure 1. Brain Magnetic Resonance Imaging (MRI) of index patient showed several ovoid hyperintensities in periventricular and subcortical white matter on Axial T2 image (Figure 1a), with gadolinium enhancement of a posterior periventricular lesion on Axial Fluid Attenuated Inversion Recovery (FLAIR) image (Figure 1b), T2 hyperintensities perpondicular to the corpus callosum on a sagittal T2 image (Figure 1c) and many others T2 hyperintensities in subcorticol white matter on other axial T2 image (Figure 1d).

Figure 2. Spinal MRI with sagittal T2 image (Figure 2a) and axial T2 image (Figure 2b) showed hyperintensities in cervical (C3 to C6) and dorsal lateral spinal cord (D10).
The involvement of the central nervous system was rarely associated with RA especially if it is a primary demyelination of the central nerve system type MS. According to literature,a, RA was found as a comorbidity in 0.6% of registred MS cases in a Norwegian study from 2008 to 2017 [1], and in 2% of 3000 MS cases in an Australian study [2]. Although this association between RA and MS has been described, the diagnosis remains difficult: Neurological manifestation of RA? Iatrogenic demyelination? Authentic MS? RA and MS are both autoimmune diseases that share similar pathogenesis particularly a T cell mediated process [3]. Although there are increasing reports that MS develops in patients with RA treated with anti-tumor necrosis factor-alpha (anti-TNF-alpha) [4]. It involves onethird of demyelinating cases under TNF-alpha inhibitors [5]. In fact, in CNS, TNF-alpha type 2 receptors are abundant. They are activated by TNF-alpha, a cytokine produced by microglia, neurons, and astrocytes to insure inflammation resolution and tissue regeneration. Anti-TNF-alpha blocks TNF-alpha type2 receptors of the brain cells, causing tissue injury and demyelinisation. Luckily, the iatrogenic CNS inflammation seems to heal with corticosteroid and the stop of anti-TNF-alpha [5]. The average interval between administration of TNF-α inhibitors and the occurrence of CNS demyelination varies from 5 months up to 6 years [6]. As well, other agents as Tocilizumab, an interleukin (IL)-6 inhibitor indicated in RA, has been linked to iatrogenic demyelination in two RA cases with incertain causality due to the prior use of anti-TNF-Alpha [5]. Also, Tofacitinib is an oral Janus kinase (JAK) inhibitor that was approved for treatment of RA. It activates T cells which produce Interleukin 17, a pro-inflammatory factor implicated in myelin injuries. clinical CNS demyelination in animals has been reported in association with tofacitinib, but only one case of reversible multifocal CNS demyelination in a human patient with RA treated with tofacitinib was described in 2020 [6]. JAK inhibitors-related demyelination may have been caused by the same intracellular signaling pathway as TNF-α inhibitors, via direct interaction between TNFR1 and JAK/STAT [6]. The comorbidity of RA and MS in patients with no anti- TNF-alpha or other treatment has been rarely reported [7,8]. In our case, diagnosis of MS was made according to clinical features and exclusion of other autoimmune diseases. Furthermore, multifocal inflammatory demyelinating lesions revealed by MRI and fulfilling MC Donald’s criteria, were suggestive of MS. In RA, MTX is given in small doses and no demyelinating anomalies on brain and medullar imaging have ever been reported. Moreover, the development of MS after the onset of RA is rare, especially in patients being treated commonly with medications such as methotrexate that have potential immunosuppressive effects [9]. Thus, the development of ambiguous neurologic symptoms consistent with MS in patients with RA whether or not they are receiving anti-TNF α should lead to consider in this context the possibility of associated MS disease.
For refractory RA, in which corticosteroid and metotrexate are inefficient, recourse to anti-TNF thearapy is recommanded. But since anti-TNF is contraindicated with the coexistance of MS, rituximab was prescribed in some cases in the litterature. In fact, even if the physiopathological mecanism suggest a major role of T cell, the B cell implication is also certain in both diseases [10,11]. Rituximab as a monoclonal antibody against CD20 antigen of B cell-surface has shown good result in the treatment of these two pathologies according Tamirou and al study [10]. For our patient, since Metotrexate and corticosteroid were sufficiently effective to get the remission of RA, we have initiated the Interferon-B-1a. Rituximab was kept as a 2nd line alternative in case of failure of current treatment.
Some agents as anti-TNF-alpha, Tocilizumab and Tofacitinib have proven effectiveness against systemic inflammatory conditions due to RA. Otherwise, clinicians should be aware of their risk of iatrogenic CNS demyelination. Our case is certainly an infrequent association of MS with RA in the absence of anti-TNF Tocilizumab and Tofacitinib treatment, which makes the originality of our case. Since the prescribtion of these molecules can aggravate Brain injuries, the use of other immunomodulating agents such as rituximab may be the best option in these situations.
Thank you for all the authors for their contribution in analysis this case report.
The authors declare that there is no conflict of interest regarding the publication of this Case Report.
Ethical approval is not required at our institution to publish an anonymous case report.
Citation: Ghachem, Ichrak, Fray, Jamoussi, Mahmoud, Ali, et al. A Case Report of Central Nervous System Demyelinaion in a Patient with Rheumatoid Arthritis: Is it Multiple Sclerosis? J Mult Scler (Foster City), 2021, 8(10), 271.
Received: 28-Jul-2021 Published: 04-Oct-2021, DOI: 10.35248/2376-0389.21.8.271
Copyright: © 2021 Ghachem I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.