Research - (2019) Volume 1, Issue 1
Introduction: Force application to a tooth during orthodontic treatment evokes a biological response of the dental pulp. The aim of this systematic literature review was to investigate the relationship between orthodontic force level and pulp reaction in humans.
Materials and methods: The orated focused question, conforming to the PICO, was “Does orthodontic treatment influence the human dental pulp vitality?” It was established according to the preferred reporting items for systematic reviews and metaanalyses. An electronic database browsing was performed from the year 2000 to December 2018 including PubMed, the Cochrane Central Register of Controlled Trials (Central) and Science Direct databases.
Results: In this systematic review, we found 52 articles matching the inclusion criteria. The methodological quality of most studies was graded moderate to low.
Conclusion: Pulpal reactions which may occur during the different treatment stages are generally of small effect in the majority of cases which have commonly a reversible character.
Systematic review, Human pulp reaction, Orthodontic forces.
Orthodontics is a field of dentistry that corrects the malposition of the jaw bones and teeth in order to optimize occlusion for functional and aesthetic purposes [1]. Orthodontic forces are often followed by the biological response of dental pulp. The pulp’s sensory role is important, but it has other roles as well [2].
The pulp functions to form dentin, among other duties. It supplies nutrients and moisture the surrounding areas of the tooth.
When the nerve tissue is damaged, often bacteria begin to multiply in the pulp chamber, leading to infection. In fact, dental pulp maintains the biological and physiological vitality of the dentin [3]. In addition, it has a highly responsive sensory nervous system that generates unbearable pain when the tooth is inflicted by mechanical trauma.
Considering that, dental pulp insures many vital functions; it is legitimate to seek answers for the relationship between pulpal health safety and orthodontic forces [4].
Rarely, pulpal side effects may appear during an orthodontic treatment. They involve pulpal necrosis and pulpal obliteration by secondary dentin [5,6].
Pulpal oxygenation rates and blood flow are reduced in the early stages of the application of orthodontic forces. The aims of this review are to study the factors that influence the pulpal vitality, to show the immediate and long term effects of the engendered dental movement and finally to suggest therapeutic solutions and precautions to prevent the loss of pulpal vitality.
Focused question
According to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines, a precise question was constructed conforming to the PICO (Participants, Interventions, Control, Outcomes) principle [5].
The orated focused question was: Does orthodontic treatment influence the human dental pulp vitality?
• (P) Participants: It was imperative for participants to have undergone orthodontic therapies.
• Types of interventions: The interventions of significance were orthodontic procedures and provoked dental movement (extrusion, intrusion, tipping, retraction, mini-screw anchorage, maxillary expansion, bonding, debonding, low laser therapy, adhesive clean-up)
• (C) Control intervention: Teeth, which did either not receive orthodontic forces or pulp tissues which were administered with different antibodies from those in the test-groups, teeth that did not receive bonding or etching were considered controls.
• (O) Outcome measures: Human pulpal reaction to orthodontic process.
Search protocol
The identification of studies which are related to the PICO question was done by an electronic database browsing using the following Boolean equations:
Boolean equation 1: “human pulp” AND “orthodontics”
Boolean equation 2: “dental pulp reaction” AND “orthodontic forces”
The search included PubMed, The Cochrane Central Register of Controlled Trials (CENTRAL) and Science Direct databases.
The language limitation imposed consisted in English and French articles and if in other languages, with full paper translated to English.
Databases were searched from the January 2000 up to December 2018.
Articles selection
Study selection: Abstracts retrieved were reviewed according to the following.
Inclusion criteria: study on humans, analysis of an orthodontic procedure in relation with the pulp, description of orthodontic treatment, specification of duration of force application, and report of pulpal reaction. The following exclusion criteria were used: animal studies, historic reviews, commentaries, case-report and letters to the editor. The records were classified as included, excluded.
The selection of studies of our systematic review of literature took place in four steps.
We began with Pre-selection of articles depending on their titles, and then we read abstracts of pre-selected articles according to inclusion criteria. Once selected, the whole article is read. Finally, full-texts of studies selected were recalled and reviewed in agreement with the above described inclusion criteria (Figure 1).
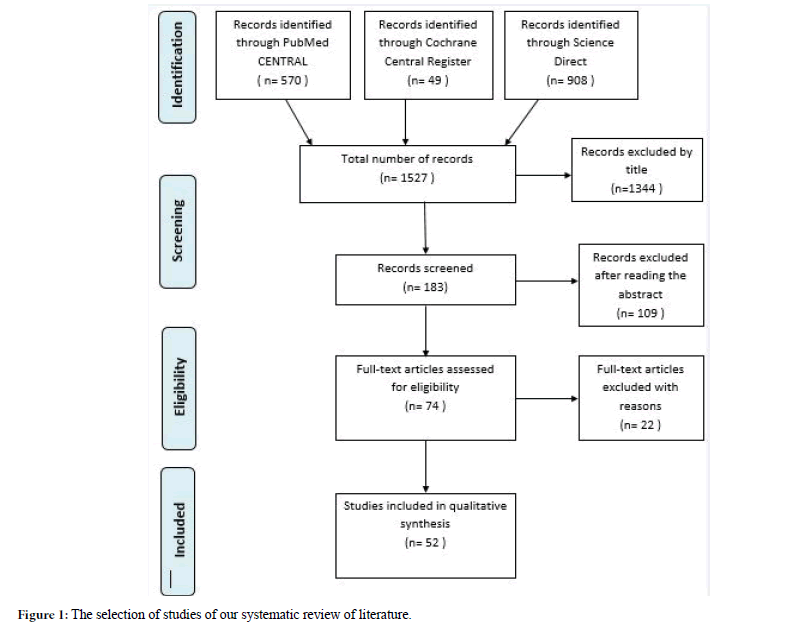
Figure 1. The selection of studies of our systematic review of literature.
Electronic search process: Several sources were used to identify all relevant studies. According to the words “human pulp” AND “orthodontics”, PubMed reveals 556 articles but with words “dental pulp reaction” AND “orthodontic forces” it reveals 38 articles. The filters used were: publication dates from 01/01/2000 to 31/12/2018. Only 19 articles were kept because they were conforming to our inclusion criteria. When words “human pulp” AND “orthodontics” were written on Cochrane, we found 52 articles. Words “dental pulp reaction” AND “orthodontic forces” only revealed one article. From this database, we only kept 5 articles. With Science direct, both equations resulted in 908 articles (694 for the first and 242 for the second) from which only 28 were selected according to our inclusion criteria.
Quality assessment: We evaluated the methodological quality of the included studies according to a grading system developed by the Swedish Council on Technology Assessment in Health Care [6].
The methodological quality standards were recorded as follow in the present review:
-Grade A (High): A randomized controlled trial or a prospective study, composed of a precise control group; defined diagnosis and end points; diagnostic reliability tests and reproducibility tests described; and blinded outcome assessment (all criteria should be met).
-Grade B (Moderate): A cohort study or retrospective study, containing a defined control group; defined diagnosis and end points; and diagnostic reliability tests and reproducibility tests described (all criteria should be met; or then, grade C).
-Grade C (Low): One or more of the following situations emerged; unclear diagnosis and end points, poorly defined patient material, and large attrition of the samples.
The articles that we selected were classified according to the pulp effecting factors to specify each type of pulpal response.
Repercussions of orthodontic forces on Pulpal Blood Flow (PBF)
Six studies [7-12] evaluated the alterations of PBF caused by orthodontic forces.: The numbers of study participants varied between 13 and 24 patients (Table 1).
| Authors et al. | Year | Design | Study subjects | Type of treatment | Control group | Force applied (N) | Duration of force | Pulpal blood flow measured by | Results | Quality grade |
|---|---|---|---|---|---|---|---|---|---|---|
| Ikawaet al. [10] | 2001 | Cross sectional study | 17 | Intrusion | None | 0.5, 1.5 | 20 s | LDF | Brief intrusive forces reduced PBF temporarily. | B |
| Sano et al. [13] | 2002 | Cohort Study | 13 | Intrusion | 13 vital teeth without orthodontic treatment | 0.5, 1.2 | 14 days | LDF | Intrusive forces reduced PBF temporarily. PBF changes rebounded to normal after stopping force application | B |
| Babacan et al. [2] | 2010 | Case series | 21 | RME | None | NR | Up to 84 days | LDF | PBF rised in the 1st week and declined significantly by the 3rd week of RME | B |
| Sabuncuoglu et al. [12] | 2014 | Cohort Study | 16 | Intrusion | 12 vital teeth without orthodontic treatment | 1 | Up to 6 months | LDF | PBF decreased with the begining of intrusive forces. PBF tended to return to baseline values by the end of the observation period. | B |
| Ersahan et al. [9] | 2015 | Cohort Study | 20 | Intrusion | 20 contralateral first molars of the same patients | 1.22, 2.45 | Up to 6 months | LDF | Important differences were observed between the 2 groups only at 3 and 7 days. PBF was more suppressed with the heaviest amount of force application. | B |
| Sabuncuoglu et al. [11] | 2016 | Cohort Study | 24 | Canine retraction | 12 participants without orthodontic treatment | 1 | Up to 4 months | LDF | By the end of observation PBF returned to pre-retraction levels. | B |
Table 1: Studies on the repercussions of orthodontic forces on pulpal blood flow.
In five studies [8-12] orthodontic forces were applied to perform intrusion and retraction of canine which is between 0.5 and 2.45 Newton (N). While in the study by Babacan et al. [5] a rapid maxillary expansion (RME) was performed and magnitude of orthodontic force applied to perform RME was not reported. The period of orthodontic forces application was between 20 weeks and 6 months. Four studies [8-12] revealed that intrusive forces temporarily reduced PBF.
Impacts of orthodontic forces on the cellular responses of the human pulp
Seventeen studies [13-28] underlined the effect of orthodontic forces on human pulpal cellular responses. In fifteen studies orthodontic forces were administrated to premolars. Orthodontic force magnitude varied between 0.25 N and 3 N and applied for 24 hours to 6 months. Rapid maxillary expansion, intrusion, extrusion, traction and tipping movements were respectively performed in two [4,26]; five [14-26]; five [13-23]; one [19]; and one [21] studies.
Seventeen studies [13-28] underlined the effect of orthodontic forces on human pulpal cellular responses. In fifteen studies orthodontic forces were administrated to premolars. Orthodontic force magnitude varied between 0.25 N and 3 N and applied for 24 hours to 6 months. Rapid maxillary expansion, intrusion, extrusion, traction and tipping movements were respectively performed in two [4,26]; five [14-26]; five [13-23]; one [19]; and one [21] studies.
Impacts of orthodontic forces on the pulp of traumatized teeth
Four studies [28-32] examined the traumatized teeth pulpal reaction in front of orthodontic -forces and concluded that pulp necrosis was more common in comparison with non-traumatized teeth.
Three studies [30-32] presented the value of orthodontic forces applied on traumatized teeth, ranged between 0.2 N and 0.15 N. In all these studies, the period of orthodontic treatment of previously traumatized teeth varied between 22.4 and 23.8 months.
Pulp response to thermal variation during different orthodontic procedures
Three studies [33-35] addressed the variation of heat level inside the pulp chamber during orthodontic bonding. This variation ranged between 2°C to 6.84 ± 2.44°C
They all concluded that the critical value for pulpal vitality (5.58°C) is not exceeded by the orthodontic bonding with lightcuring units.
Uzel et al. [36] reported that the increase in the pulpal temperature was more important with Halogen light-curing unit than the lightemitting diode (LED) and Xenon Plasma Arc (PAC). They also demonstrated the role of application distance and that the lower incisors were more likely to show such changement.
Concerning stripping, two studies [36,37] were evaluating the modification of pulp temperature during this procedure.
Baysal et al. [36] found that using tungsten carbide burrs caused intrapulpal temperature increase that overreached the critical level of 5.5°C when applied on lower incisors.
Pereira et al. [37] indicated that a double-sided perforated stripping disk (PSD) engendered a notable increase in pulp temperature, regardless the type of teeth.
At last, Influence of Mini-screws on pulpal vitality is no longer to be demonstrated.
Two studies [1,38] called attention to the potential risks and side effects of clinical usage of orthodontic anchor screws.
Alves et al. [1] concluded in his systematic review that miniscrews which perforated the pulpal space had fewer chances to show complete healing of periodontal tissues.
This systematic review had for purpose to explore the effect of orthodontic force application and dental pulp reaction in humans.
It focused on collecting data from researches published in the twenty-first century unlike other systematic reviews [39,40] that expanded their work up to the last century (Table 2). Those two systematic reviews only investigated the impact of orthodontic forces on the dental pulp; however, in this study we tried to pursue the pulp changes that may occur from the beginning of the orthodontic treatment and during its different stages. We tried to refine our search by reading full text studies instead of abstracts and by using strict inclusion criteria.
| Systematic reviews | Similarities | Differences |
|---|---|---|
| von Bohl et al. [39] | - Use of PRISMA flow diagram for the process of study selection. - Studied orthodontic forces relationship with : • changes of PBF • pulpal histologic and cellular changes |
- Including outdated studies belonging to the previous century. - Not studying orthodontic forces relationship with : pulpal vitality of traumatized teeth |
| - Not studying the adverse effects on pulpal vitality of orthodontic treatment as a whole or detailing its different aspects. | ||
| Javed et al. [40] | - Use of PRISMA flow diagram for the process of study selection - Studied orthodontic forces relationship with : • changes of PBF • pulpal histologic and cellular changes • pulpal vitality of traumatized teeth |
- Including outdated studies belonging to the previous century. - Not studying the adverse effects on pulpal vitality of orthodontic treatment as a whole or detailing its different aspects. |
Table 2: Comparison of the present systematic review with other recent ones.
In our study we gave more importance to histologic changes occurring on the pulp during orthodontic treatment.
When inspecting the repercussions of orthodontic forces on pulpal blood flow, force applied in the six reviewed studies [8-13] ranged between 0.5 N and 2.45 N for a period of time varying between 20 seconds and 6 months. Regardless of the differences of these parameters, orthodontic forces had a temporary incidence on the pulp irrigation.
The measurements of pulpal blood flow were achieved by Laser Doppler flowmetry in all six studies [8-13]. This technique is easily affected by environmental and technical elements, particularly flow meter characteristics, ambient temperature, gingival isolation device, probe position, rest status and patient position. Other factors linked to patients like those related with stress, medication and age can also affect LDF measurements of PBF [11].
A histologic study by Lazzaretti et al. [4] demonstrated that, after 3 weeks of application, orthodontic intrusion force resulted in vascular changes of the pulpal tissue such as pulpal nodules, as well as an increase in the presence of fibrosis and in the number of calcifications of the pulp. These events might be temporary considering the short observation period.
Selected studies [13-33] showed the susceptibility to radicular external resorption and pulp necrosis in teeth with trauma history when undergoing orthodontic treatment. External root resorption depended on type and intensity of trauma. Bauss et al. [32] reported the higher susceptibility to pulp necrosis of traumatized maxillary incisors, specifically lateral incisors, which was probably linked to the fragile anatomy of these teeth. Traumatized teeth whose pulp is completely obliterated were more exposed to pulp necrosis.
Along with the bonding composites, the photo polymerization lamps had evolved. Actually, only high intensity halogen lamps exceeded the critical threshold of 5.5°C (temperature change damaging to the pulp), they reach a temperature increase of 6.84°C ± 2.4 [34]. Higher temperature increase was recorded during the photo polymerization on lower incisors than on the premolars [41].
As a common alternative of non-extraction treatments in orthodontics practice, some studies reported the possible harmful incidence of inter proximal reduction technique on the dental pulp. Studies by Baysal et al. [37] and Pereira et al. [38] concluded that stripping can only be harmful to dental pulp when it is done without convenient measures such as cooling application especially for high-speed hand-piece stripping of mandibular incisors.
When teeth are subjected to orthodontic movement with or without Low level laser therapy, it is usual to detect a cell-rich area into the cell-free layer that is differentiated from the central pulp portion by the high number of cells per area unit, mainly fibroblasts and undifferentiated mesenchymal cells, as a result of its stimulating effects on fibroblasts and collagen fibers. It is also noted that this cell-rich zone is more abundant on irradiated teeth than in the control group.
The benefit of obtaining a high ARI (adhesive remnant index) is to avoid enamel prism tear damage. However, the disadvantage here is the risk of excess heating during the removal of the adhesive. The ideal was to use a tungsten carbide burr with water irrigation (for keeping pulp heating as low as possible below the threshold of 5.5°C). This way, pulpal histological changes were going to be avoided or at least reversible [2]. Other authors proposed the use of CO2 laser to decompose the bonding resin in order to reduce the forces required to remove the brackets [41]. The laser would significantly decrease enamel fractures, improve the ARI score and minimize the fracture of ceramic brackets, compared to brackets removal using conventional pliers.
The CO2 laser would not increase the temperature above the critical threshold 5.5°C [42].
The study of Kailasam et al. [43] proved that the pulp was mostly unaltered by this procedure with most of the changes being inconstant. After debonding, adhesive residue needs to be cleaned-up and enamel surface totally polished.
As for mini-screw impact, studies that we included about this anchorage technique [44], proved the irreversible nature of pulp damage resulting from it. More careful planning for placing these devices is mandatory to reduce the probability of root resorption.
To investigate the method of corticotomy, we included four studies [45-47] and they all agreed that corticotomy intervention/ process did not seem to cause side effects on the periodontium, and tooth health.
We also noticed that few studies, observed the dental consequences of corticotomy, probably because of the low clinical decline of this technique or because little pulpal damage had been observed.
The assessment of the complications following Lefort I osteotomy in the present study revealed that the prevalence of pulpal ischemia is proportional to the distance between dental apices and the incision site [48]. If the osteotomy is performed less than 5 mm above apices, vitality loss may occur.
The force applied to a tooth during orthodontic treatment induces a biological response of the dental pulp. This response causes initially changes in blood flow, increases the level of growth factors angiogenesis. It’s an inflammatory- like effect on pulp tissue,
Evidence based on the currently available studies showed that orthodontics does not represent a real danger for the pulp. The pulpal reactions which may occur during the different treatment steps are generally of small amplitude and in the vast majority of cases have a reversible character. When pulp necrosis is detected during or following orthodontic treatment, it is necessary to consider the origin of the necrosis. Further research is hence required to detect the long-term effects of orthodontic therapeutics on pulpal vitality.
Received: 30-Jul-2019
Copyright: ©2019 Dallel I, et al. This is an open access paper distributed under the Creative Commons Attribution License. Journal of Health and Medical Research is published by Lexis Publisher.