Journal of Multiple Sclerosis
ISSN - 2376-0389NLM - 101654564
Research Article - (2022) Volume 9, Issue 5
Objective: Bowel dysfunction is highly prevalent in patients with Multiple Sclerosis (MS). A tool to help decision-making of neurogenic bowel dysfunction treatment in this population is needed. We present a project to validate in this population the MENTOR tool, a three-dimensional instrument comprised of the Neurogenic Bowel Dysfunction (NBD) score, special attention (‘alarm’) symptoms and patient satisfaction. Methods: 69 individuals with MS completed the MENTOR tool prior to outpatient review. An expert Health Care Professional (HCP) blinded to the MENTOR outcome assessed the participants and made an independent treatment decision. We compared the tool outcome and therapeutic recommendation with the HCP opinion. Results: In our patient cohort, the MENTOR has a specificity of 80%, accuracy of 70% and a sensitivity of 60% with a positive and negative predictive value of 68% and 73% (respectively), a positive and negative likelihood ratio of 3 and 0.5 (respectively). Stronger concordance with HCP evaluation was found in patients that fall in the category “monitoring” (88%), and “change” (71%); the lowest concordance was in the individuals that need “further discuss” (38%). Of note, agreement with HCP evaluation was significant for total NBD score (especially incontinence symptoms of the NBD score) but not for patient’s satisfaction component or special attention symptoms. Conclusion: The MENTOR tool has potential utility in patients with MS with bowel dysfunction. The special attention symptoms and the patient’s subjective report had a less predictable relationship with HCP expert opinion than the NBD component. Optimizing the tool further will be the subject of future work.
Multiple sclerosis • Patient assessment tool • MENTOR tool • Neurogenic bowel dysfunction • Therapeutic management
Multiple Sclerosis is an autoimmune condition, causing demyelination of the Central Nervous System (CNS) leading to the formation of plaques in white matter and dysfunction of the neurological pathways affected [1]. MS is classified according to how symptoms present. It is one of the most common neurologic disorders and the leading cause of non-traumatic disability in young adults [2].
Bowel dysfunction with MS is highly prevalent and highly problematic for the patients. It is described that 29%-50% of patients experience Faecal Incontinence (FI), while 36%-54% report constipation [3]. Bowel dysfunction is a source of considerable psychosocial disability [4] and bowel care can take a long time and reduce the patient independence. Hence, a systematic assessment of symptoms and consequent management of bowel symptoms in MS is needed.
The management approaches of neurogenic bowel dysfunction include optimization of fluid and dietary habits, use of laxatives and suppositories, use of Loperamide, digital anorectal stimulation, manual evacuation, trans anal irrigation, percutaneous tibial nerve stimulation and stoma formation [5-6]. Treatment optimization is based on symptom management and understanding of pathophysiology, but it remains a challenge to know when it is best to make treatment adjustments in MS patients with bowel dysfunction [5].
Patients require detailed assessment of gut function, and -when necessary- modified in management over time [7]. Considering the limited access to specialist neurogastroenterology services and the chronic nature of the symptoms, management often occurs in the community and nonspecialist services. A tool that supports decision-making can facilitate this process for healthcare workers.
Followingconsensus evaluationofthe efficacy of different assessments available for Spinal Cord injury individuals, the Monitoring Efficacy of Neurogenic Bowel Dysfunction Treatment on Response (MENTOR) tool (https://www.coloplast.com/mentor-tool/) was developed. MENTOR Tool was validated in different settings gastroenterology outpatient clinics (UK, Denmark) SCI rehabilitation or spinal units (USA, Italy, The Netherlands, Germany) as well as non-hospital settings [8-10].
Aim
The aim of this project was to explore the utility of MENTOR in a patient population with bowel dysfunction associated with MS. We compared the tool recommendations with the HCP opinion and explored how each part of the tool performs in this patient group population.
Patient’s cohort
We enrolled individuals with MS from two specialist neurogastroenterology outpatient clinics in Denmark and UK. All individuals had confirmed diagnosis of MS and most patients were in a stable phase of the disease. In comparison with the initial MENTOR tool development, our cohort of patients is different both for the type of disease MS vs SCI, and expected more Gastroenterological Symptoms as it is a cohort of patients that has been referred to a specialist centre for neurogastroenterology expert review. The UK patients were recruited from a specialist neurogastroenterology service and comprised of a mix of routine review patients and some (2% of the UK cohort) urgent patients who initiated self-referral with a recent symptoms change. The Denmark patients were recruited from a specialist neurogastroenterology service and comprised of patients referred for bowel symptoms management, with both chronic and recent onsets of bowel symptoms.
All patients were aged above 18. MENTOR tool was used as part of clinical routine practice. Each participant was identified with initials, age, and sex. The MENTOR tool was self-completed before the patient saw the consultant. A member of the team was checking that the form was completed in all their parts. The consultation preceded as per usual practice and the consultant completed the data collection template for physicians at the end of the visit. The possible outcomes of the visit were “monitor”, “discuss”, and “change”. Data were entered in a pre-determined and locked Excel file before analysis.
MENTOR tool
MENTOR is a three dimensions tool comprised of
1. the Neurogenic Bowel Dysfunction (NBD) score [11],
2. patient perception of satisfaction with bowel function,
3. presence of ‘special attention’ symptoms.
The NBD score describes symptoms of constipation and faecal incontinence. Traditionally, three cuts off have been used for spinal injury patients, correlated with quality of life impairment [11].
Subjective patient satisfaction describes the patient’s own perception of satisfaction with their bowel function, categorised in four possible states "good", "adequate", "poor" and "very poor".
The special attention symptoms describe the elements of comorbidity that may be linked to poor bowel management.
These three factors are plotted in a grid corresponding to a “traffic light” system also called a decision matrix. These regions are the green “monitor” area which represents adequate treatment; the yellow “discuss” area which describes a suboptimal treatment where further discussion, symptoms education and close monitoring for 1-3 months are welcomed; and the red “act” area that describes an area of suboptimal treatment where a change in management is needed [8]. Descriptive statistic was performed; data were tested for normal distribution with quantile vs quantile plot test. We used parametric t-test for normal comparisons and chi-square test for associations. Statistical significance was accepted as a p-value<0.05. Standard properties of a diagnostic test like sensitivity and specificity were also described diagnostic accuracy was evaluated with a formula and exploring the likelihood ratio [10,12-14].
We recruited 69 individuals with MS (average age 47 years (range 25- 73), 40 of who were women (58%). The UK centre recruited 57 and the Danish centre 12 patients.
The distribution of our patients with MS on the MENTOR grid shows that 36% were classified as green, 23% as yellow and 41% as red. As shown in Table 1, the MENTOR tool in individuals with MS and the HCP assessment had an overall concordance of 62%. This compares with the spinal cord injury study, in which the MENTOR tool had an overall concordance of 79% [8, 15]. Concordance between the tool outcome and HCP opinion was highest for those subjects classified in the decision matrix as “green” 88% (where no change is needed) and those classified as “red” 68% (where a change in current bowel therapeutic approach is recommended). The highest level of concordance in these two groups is similar to the characteristic of MENTOR in the SCI study [8]. The concordance is lowest for those patients who fall in the “yellow” group 13% (where further discussion is needed).
Table 1. MENTOR results and agreement with health care professionals in patient with multiple sclerosis. Mentor assigned participants in three categories green, red, and yellow.
| Colour | Number | % |
|---|---|---|
| Green | 25 | 36 |
| Yellow | 16 | 23 |
| Red | 28 | 41 |
| Total Sample | 69 | |
| Concordance Green | 22 | 88 |
| Concordance Yellow | 2 | 13 |
| Concordance Red | 19 | 68 |
| Total Concordance | 43 | 62 |
| yellow+no change | 6 | 38 |
| yellow+change | 10 | 63 |
| Total Treatment Change | 30 | 43 |
As shown in Table 1, 43 individuals received an evaluation that agrees with MENTOR tool outcome and 26 individuals received an evaluation that disagrees with MENTOR tool outcome. Figure 1 describes the concordance in the different components of the tools as well. There was a statistically significant association between overall NBD score and MENTOR agreement with HCP decision (p<0.05, chi-square); when the FI sub-score of the NBD was similarly tested it also showed statistical significance (p<0.04, chi-square). Significance was not demonstrated for patient satisfaction (p=0.11) and special attention symptoms (p=0.47).
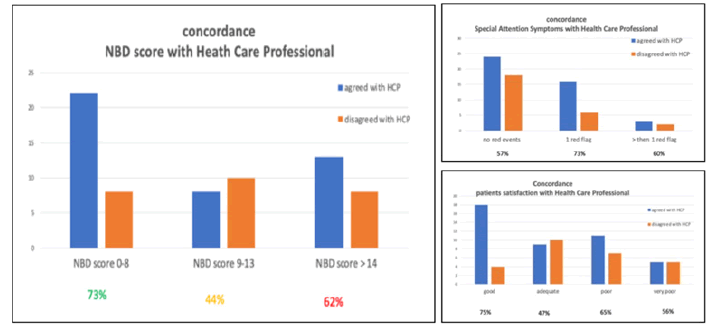
Figure 1: Concordance description in the three MENTOR tool components.
Overall, the MENTOR tool in MS population has an accuracy of 70%, this characteristic describes the ability of the tool to differentiate patients that require a change of bowel management from those that do not need it. The sensitivity is 60%, this characteristic describes the ability of the tool to determine correctly who needs changes in the current bowel therapeutic approach. The specificity is 80%, reflecting the ability of the tool to determine who does not need a change in bowel management and needs only monitoring correctly [12].
We also looked at MENTOR tool screening performances in MS population, these characteristics describe if a participant is classified in one of the three tool categories how likely it is to be correct [13]. MENTOR tool has a positive predictive value of 68% and a negative predictive value of 73%.
The likelihood ratio is considered one of the most reliable performance measures to describe diagnostic accuracy [16]. It describes how many times more (or less) likely patients with the need to change bowel care management are recognized than patients that don’t need the change [17]. The MENTOR positive likelihood ratio is 3 and the negative likelihood ratio is 0.5, this means that the test results are associated more with the absence of the need for change.
The data from this study suggests that the MENTOR tool has some utility in the assessment of MS patients with neurogenic bowel dysfunction but further optimization is needed to consider it suitable for implication in clinical routine. Usually tests with 0.1
The patients in the intermediate (“yellow”) group are predictably the most complex to assess. When patients present with, at one extreme, stable symptom, or at the other new and worrisome ones, it is often clear what needs to be done most appropriately. It is to be expected the MENTOR would perform well in these situations, as shown. This is similar to what was observed in the validation study of MENTOR in SCI, but to a more pronounced degree. However, the poor utility in these intermediate patients may reflect the fact that the MENTOR was developed for patients with SCI [8]. The pathophysiology of neurogenic bowel dysfunction in patients with MS is distinct from that in SCI [18-19]. Hence the constituent components of the MENTOR may not all be suitable for MS patients.
The mean NBD score in patients where there was concordance between the MENTOR score and HCP opinion was significantly less than when there was no agreement (NDB average 10 when there was concordance vs NDB average 15 when there was disagreement). This suggests that there is validity in using the NBD score component of the MENTOR in MS patients. With that in mind, we analysed the component of the NBD score which related to constipation separated from the components related to faecal incontinence. We compared these components with the agreement outcome and found that the faecal incontinence component of the NBD score (described by the last 4 questions of NBD) was the one that contributed to this relationship.
Faecal incontinence in MS can arise from a variety of pathophysiological mechanisms. Patients may have pelvic floor dyssynergia with weak or incomplete relaxation of the puborectalis and anal sphincter on defaecation [20-22]. In addition, there may be abnormal control of the voluntary component of the anal sphincter, analogous to detrusor sphincter dyssynergia in the bladder [23]. Or, it may be an acquired behavioural problem present as in patients with functional constipation [24]. Some individuals with MS may have structural sphincter abnormality (especially if they have had an obstetric history), weak anal sphincters or reduced anorectal sensation [18, 22]. In addition to these anal disturbances, there may be altered rectal function contributing to symptoms. Rectal compliance is known to be higher in MS patients with major lower limb dysfunction compared to MS patients with more minor dysfunction [25]. Furthermore, MS patients with a major disability had higher urge volumes to rectal balloon distension, and also high thresholds to anal electro-sensitivity [19, 26]. Alterations in rectal compliance can cause both faecal incontinence and constipation [27,28]. In some individuals, reduced rectal compliance contributes to faecal incontinence, while in others increased rectal compliance contributes to constipation-like symptoms [18]. This suggests that altered sensory mechanisms within the anus and the rectum may contribute to the pathophysiology of both incontinence and constipation. Finally, there may be abnormalities of the Recto-Anal Inhibitory Reflex (RAIR) in MS patients. Diminished relaxation of the anal sphincters is seen in some patients with constipation, while in faecal incontinence there is a correlation between symptom severity and prolonged duration of RAIR and recovery phase [19,26]. Understanding of the possible mechanisms underlying bowel dysfunction in MS patients is critical to being able to offer supportive lifestyle advice and tailor treatments as appropriate.
There is no literature on the impact of psychological factors on bowel symptoms in people with MS. The relationship between psychological status and level of activity of extrinsic gut innervation has been discussed in patients with functional gut disorders [29]. Anxiety scores have been shown to be higher in MS patients than in the general population [30], again highlighting a role for patient-HCP discussion as an important management strategy.
Looking at the other components of MENTOR, there are five special attention symptoms: intense pain in the abdomen or rectum, new or increased bleeding from the anus, hospitalisation due to bowel problems, and reduction in independence with regard to bowel care and autonomic dysreflexia related to bowel care. We think that most are appropriate for patients with MS but not all, for example, autonomic dysreflexia is not common in patients with MS. Future qualitative work will detail the most frequent alarm symptoms indicative of bowel dysfunction. Similarly, an analysis of the utility of the subjective assessment will be undertaken to see if the tool can be improved and revalidated for MS patients. Another focus of refinement work on the tool in MS patients will include more detailed exploration of the intermediate (‘yellow’ categorised) patient cohort.
The tool performs better when patients fall in the cohort where there is less need for intervention which means that at present, patients that require further discussion (and to a lesser extent those who need optimization of current bowel management) may be missed. A tool that facilitates decision-making is needed considering the absence of a gold standard strategy for optimization of bowel management and the complexity of multifactorial causes of symptoms in MS patients. This study indicates that further work on the current MENTOR instrument needs to be done to improve the tools’ sensitivity in MS patient population, to identify the more symptomatic patients.
Acknowledgement
Lia Walhagen, Associate Medical Specialist, Coloplast A/S, Denmark for the work coordination. Marko Kerac and Karine Le Roch for sharing their passion of the importance of using a good tool in clinical practice.
Sources of Funding
The manuscript construction was supported by an educational grant from Coloplast, Denmark.
[Crossref]
Citation: Brugaletta C., et al. Validation of the Monitoring Efficacy of Neurogenic Bowel Dysfunction Treatment on Response (MENTOR) Tool in Individuals with Multiple Sclerosis. J Mult Scler. 2022, 09(5), 441.
Received: 25-Apr-2022, Manuscript No. jmso-22-61751; Editor assigned: 27-Apr-2022, Pre QC No. jmso-22-61751(PQ); Reviewed: 30-Apr-2022, QC No. jmso-22-61751(Q); Revised: 03-May-2022, Manuscript No. jmso-22-61751(R); Published: 10-May-2022, DOI: DOI: 10.35248/2376-0389
Copyright: ©2022 Brugaletta C., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.