Case Report - (2020) Volume 11, Issue 5
To describe the clinical presentation and imaging features of a patient with optic nerve leukemic infiltration as the first site of relapse after complete response to systemic treatment. We report the case of a 23yr old man with history of Acute Lymphoblastic Leukemia (ALL) in complete remission. Six months later, the ocular examination revealed decreased visual acuity. Fundus examination showed a pale optic disk with blurred margins and multiple flame-shaped and dot and blot retinal hemorrhages in his left eye. A diagnosis of leukemic infiltration to the optic nerve was made by Magnetic Resonance Imaging (MRI). Cytological analysis of the cerebrospinal fluid did not show any abnormal cells or blasts. A course of oral corticosteroid therapy was prescribed and 20Gy of radiation was administered to the whole brain including the left orbit. Vision was improved dramatically in the left Eye. Isolated optic nerve relapse of leukemic infiltration is of paramount importance to early diagnosis, as vision can be saved if treatment with orbital radiotherapy if initiated promptly.
The Relapse in ocular structures without systemic involvement is extremely rare in Acute lymphoblastic leukemia (ALL). Active bone marrow disease is usually associated with optic nerve infiltration (ONI) [1]. However, ONI is rarely reported as an initial site of relapse after complete systemic remission. This relapse, If diagnosed and treated promptly deterioration of vision may be prevented [2]. We describe an adult patient with ALL whose disease relapsed with unilateral left side optic nerve infiltration of leukemic cells who suffered sudden vision loss 6 months after complete remission. We discussed the implications of early diagnostic and the optimal treatment for vision prognosis.
A 23yr old man was diagnosed with T cell ALL and treated with conventional chemotherapy including vincristine 2 mg/m2 associated to prednisolone 70 mg/m2 and L-asparaginase 6,000 U/m2. Prophylactic intrathecal therapy was administered with methotrexate. The Cerebro Spinal Fluid (CSF) examination was carried out prior to each intrathecal-therapy drug instillation without any Central Nerve System (CNS) suspicious disease. Complete remission was achieved. The patient refused the intracranial prophylactic treatment. Six months later, he complained of dimness of vision for 25 days in his left eye. A cerebral Magnetic Resonance Imaging (MRI) was performed, showing an isolated thickening of the left nerve with increased perineural gadolinium enhancement (Figure 1). On fundoscopic, left sided optic disc edema and peripapillary nerve fiber layer edema was detected (Figure 2). There was peripapillary retinal hemorrhage but vitreous, macula and retinal vessels were normal. The optical coherence tomography (OCT) indicated swollen of left optic nerve (Figure 3). CSF was normal at morphologic and immunophenotypic studies. The CSF viral studies (CMV, EBV, HHV-6, HSV1, HSV2) were performed without abnormalities. A curative orbital radiotherapy (ORT) at the dose of 20 Gy was administered associated to intracranial irradiation. An improvement in Vision was reported after the first few sessions. A consolidation chemotherapy was continued. Fundoscopic examination showed resolving of the hemorrhage. After 12 months of follow up, he remained stable for many months but unfortunately developed systemic complications and intramedullary progression and he could not survive.
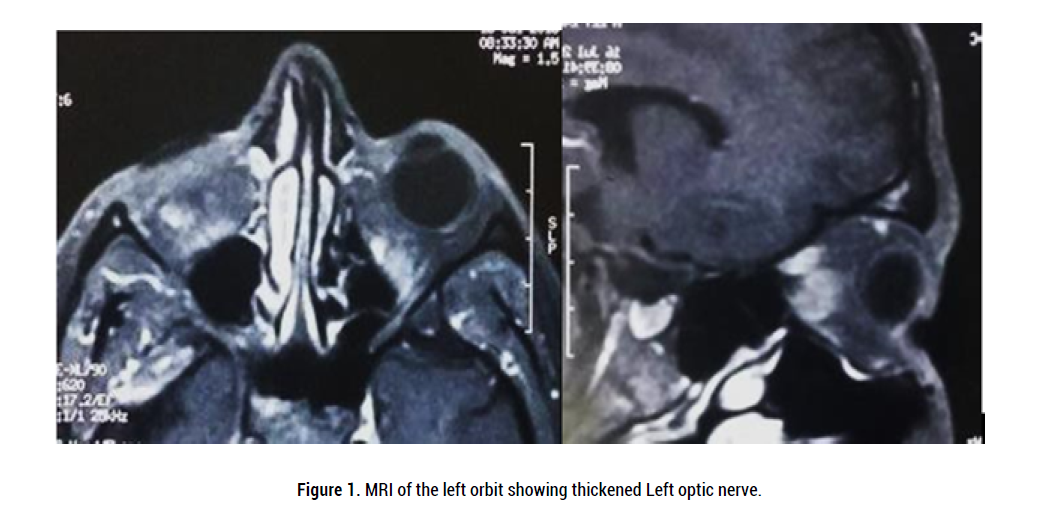
Figure 1: MRI of the left orbit showing thickened Left optic nerve.
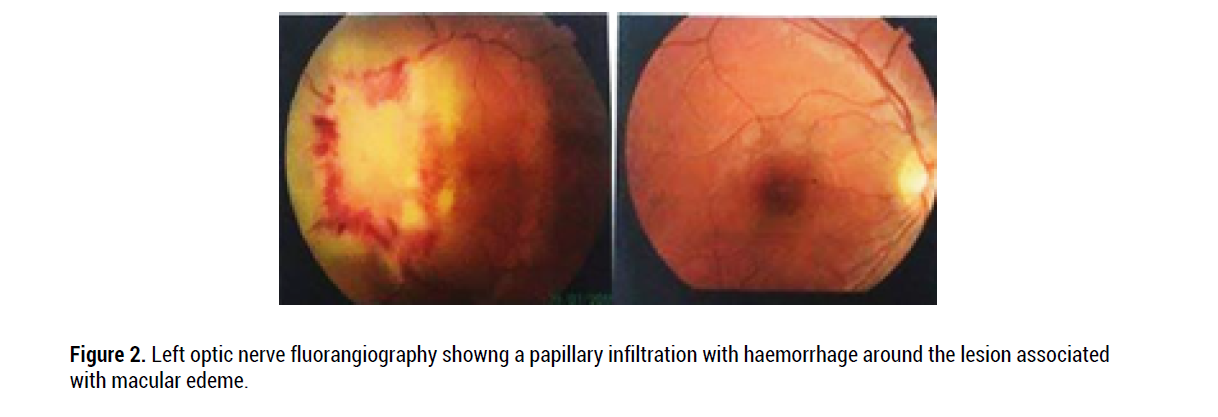
Figure 2: Left optic nerve fluorangiography showng a papillary infiltration with haemorrhage around the lesion associated with macular edeme.
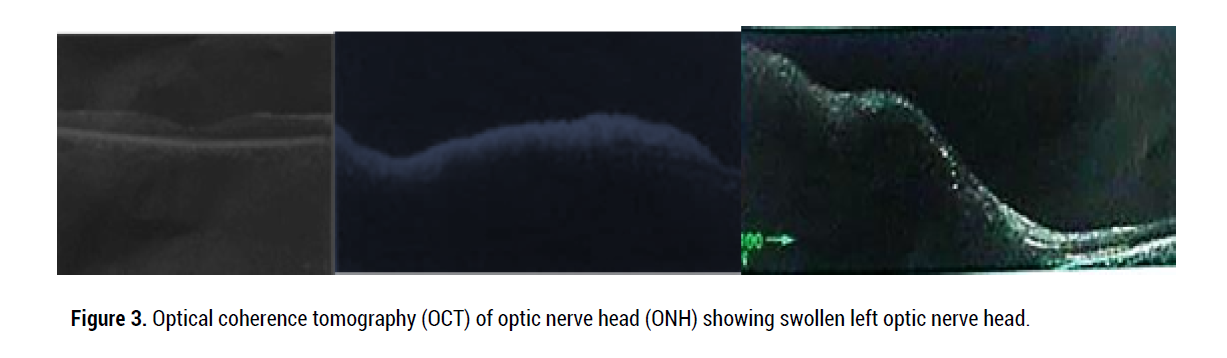
Figure 3: Optical coherence tomography (OCT) of optic nerve head (ONH) showing swollen left optic nerve head.
The estimating incidence of ocular infiltration in ALL varied between 5 to 13% [3]. The largest series of 657 children identified a 4.4% rate of infiltration of the optic nerve, retina, iris, or orbit [4]. Intracranial irradiation and intrathecal chemotherapy are required to prevent recurrence of ALL and to attain the complete remission. The orbital cavity and optic nerve are potential sanctuaries for leukemic relapse after conventional central nervous system prophylaxis because these structures are shielded during brain irradiation [3]. Clinicians should be aware of this possible manifestation even after achieving disease remission. The CNS relapse and ocular involvement in ALL usually indicate refractory disease and a poor prognosis [5]. ALL have an eye-meningeal risk of infringement more important than acute myeloid leukemia and always receive prophylactic treatment of CNS by repeated intrathecal injections of cytostatic. This treatment is associated in adults to radiation CNS including the optic nerve in its extra-orbital portion [6]. Early limited relapse without systemic involvement is a challenge issue for clinical management because the optic nerve is relatively unaffected by systemic chemotherapy and serves as a sanctuary of ALL [7,8]. To confirm the diagnosis of ONI, other causes of decreased visual acuity in ALL have to be excluded like infection, vasculitis, radiation optic neuropathy or side effects of chemotherapeutic agents [2]. The typical appearance was an infiltration of the entire papillary region by a tumor mass, accompanied by exudates and hemorrhages and forming a projection into the vitreous cavity. Sometimes bilateral, but often asymmetrical, it must be differentiated from papilledema on intracranial pressure [9]. Decreased visual acuity, perivascular infiltration and parapapillary retinal, an asymmetrical involvement and the absence of clinical signs of intracranial hypertension or meningitis argue for a blast infiltration of the optic nerve. The occurrence of papilledema mechanism is a consecutive venous obstruction to the invasion perivascular by leukemic cells [9]. The efficacy of intrathecal chemotherapy is limited because the drug is unlikely to reach the optic nerve located in an optical channel obstructed by tumor infiltration. The most effective treatment is irradiation of the orbit at a dose of 20- 24 Grays over 2 weeks [9]. Early administration of focal RT allows the cytotoxic drugs to reach the CSF to attack the neoplastic cells. Optic nerve is relatively less sensitive to RT whereas leukaemic cells are quite radiosensitive. It must be done as early as possible to observe a rapid regression and improvement of visual function. Treatment should be instituted before irreversible optic nerve damage occurs. The target volume should involve the posterior poles of the globes with or without whole brain treatment [10]. Despite intensive treatment the prognosis is poor and is related to other risk factors of bone marrow with CSF involvement and the length of initial hematological remission. Overall survival in case of eye location is less than 24 months [9].
Two larges retrospectives multicenter studies included a total of 59 patients with leukemic orbital infiltration, most of whom also had bone marrow or CNS involvement [11,12]. Results suggested that patients treated with RT were more likely to achieve remission. The authors recommended doses of greater than 20 Gy to the affected eye [11]. RT to the orbital structures is associated with the risk of long-term morbidity. However considering that radiation-induced cataracts can be surgically removed but an inadequate RT dose may increase the risk of progression [3]. Intravitreal methotrexate administration can be also another option therapy in this case relapse [13].
In this case, the intracranial and orbital irradiation was delivered simultaneously with a complete recovery of left eye sight. The optic nerve leukemic infiltration should be kept in mind in high-risk patients with T-cell ALL. the accurate ophthalmologist and MRI can suggest early diagnosis of ONI. Prompt irradiation should be given to prevent irreversible visual loss.
Received: 21-Jun-2020 Published: 05-Aug-2020
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.