Research Article - (2023) Volume 9, Issue 1
Introduction: A hospital or other healthcare facility's Intensive Care Unit (ICU) is a unique division that offers intensive care medicine.
Highly skilled medical professionals and nurses, who specialise in caring for critically ill patients, work in these facilities. ICUs differ from ordinary hospital wards by having a larger staff-to-patient ratio and having access to cutting-edge medical tools and resources that are not frequently found elsewhere. The selection and admission of patients should be based on classical indices, especially for patients who benefit of intensive care, have lower risk of mortality and better prognosis. On the other hand, the long stay of patients in ICU isn’t cost-effective and is a barrier for admission of new patient. Hence, identification of postoperative complications is necessary for effective planning for optimal use of ICU beds and facilities. Proper planning and consideration of factors in reducing the mortality rate, and correct planning of treatment, the scientific and systematic admission of patients in intensive care units and separation of surgical and internal intensive care units can reduce the mortality rate in this unit as the most important measure for efficiency of the treatment unit.
Aim: To evaluate factors affecting on patient admission from operating room to intensive care unit in Pravara Rural Hospital, Loni.
Materials and Methods: Ethical approval for this study was obtained from the Institutional Ethical Committee. All patients between 20 yeras-60 years of age, of either gender, who are shifted from operation theatre to the intensive care unit in postoperative period, were taken in for the study. The data was obtained through observation.
Results: The study with a sample size of 120 showed maximum subjects was males (59.16%). The Subjects classified under ASA grading whom were shifted to ICU were maximum of ASA grade 4 being (36.66%) and least being grade 1 (7.5%). The subjects undergoing or facial maxillary surgery was the most common to be shifted to ICU being 31.66%. The subjects with hypertension was the most common comorbid status encountered accounting to 20%, the elective monitoring stood most common reason for shifting to ICU being 77.5%.
Conclusion: The airway related problems are most commonly expected hence it is most common to see the patient with head and neck surgeries are shifted out of operation theatre for ICU care.
Post operative period • Intensive care unit • Operation theatre • Ill patients
In modern era, ICU was introduced in the 1960’s. ICU is the unit in the hospital, allocated to critical ill patients. The patients undergo continuous cardiorespiratory monitoring and also undergo lifesaving techniques such as airway management, transfusion of blood and various intravenous fluids and drugs. Multiple perioperative factors contribute to morbidity or mortality in a perioperative period. Hence patient selection should be based on classical indices so to benefit for intensive care and in turn better the prognosis. The limited number of beds in ICU, financial burden in prolonged ICU stay and improper shifting handover are the limiting factors. The effective planning of ICU bed utilization, anticipation of postoperative complications and proper communication between the teams, so that appropriate solutions are provided to prevent complications is of utmost importance [1].
The length of the ICU stay is associated with patient’s preoperative status. The post-operative complications lead to prolonged ICU stay. Risk evaluation is mainstay to decide and to assess about the preoperative risks; hence, some special indices are used. Therefore, the precise definition of complication and low threshold seems to be necessary for designing the classification system [2]. Different measures are used to evaluate the risk of operations such as ASA classification. ASA classification is a status classification system of physical category to examine the patient physical status before choosing the type of anesthesia and operation. Different factors such as age, sex, underlying diseases, clinical symptoms, and laboratory findings are involved in these classifications [3].
The study is an observational descriptive longitudinal study conducted in intensive care unit, Pravara Rural Hospital, Loni, Maharashtra for a period of 6months i.e. from March 2021 to August 2021. The subjects were who was shifted to ICU for post operative care from operation theatre [4].
Inclusion criteria
• Patients aged between 20 yeras-60 years of either gender
• Patients who are transferred from operating room to intensive care unit.
Exclusion criteria
• Patients who have undergone surgery from other hospital and getting admitted to our hospital.
• Patients who are already in the ICU and taken up for surgery.
The study with a 120 sample size conducted in Intensive care unit. The variables included were gender, ASA grade, and time of decision, reason for shifting, co morbid status and type of surgery. Among the subjects, 71 (59.16%) were males and 49 (40.83%) were females. The age distribution in the study was within 20 years-60 years with most common age group being 60 years 20 (16.6%). The observation made in relation with subjects being shifted to ICU with ASA grading constituted ASA grade IV being the maximum accounting of 44 (36.66%), followed by grade III 36 (30%), Grade II 31 (25.83%) and least being Grade I 9 (7.5%).
The observations in the study showed most surgical procedure under which the subject was shifted to ICU was OMFS constituting 38 (31.66%). The other surgeries were General surgery 34 (28.33%), Neurosurgery 23 (19.16%), Obstetrics and Gynecology 14 (11.66%), ENT 5 (4.16%), Plastic and reconstructive surgery 3 (2.50%), Orthopedic surgeries 2 (1.66%) and Urological procedures 1 (0.83%) [5,6].
The comorbidity status observed were of Hypertension 24 (20%), Diabetes mellitus 14 (11.66%), Rheumatic heart disease 1 (0.83%) and COPD 1 (0.83%). Few subjects had multiple comorbidities affecting their care which accounted for 5 (4.16%) out of the total sample. The time of decision to shift patients from OT to ICU, prior to surgery was 96 (80%) and intraoperative was 24 (20%). The reasons for shifting to ICU were for elective monitoring 93 (77.5%), complications due to comorbid illness 15 (12.5%), surgical complications 11 (9.16%), and an aesthetic complications 1 (0.83%).
The decision of the team in shifting to ICU from OT, Anaesthetist 87 (72.5%), both 30 (25%) and surgeon 3 (2.5%) the patients were shifted to ICU maintained on various oxygen devices most common being endotracheal tube 76 (63.33%) followed by Face mask 32 (26.66%) and least being with tracheostomy 12 (10%) (Figures 1-8).
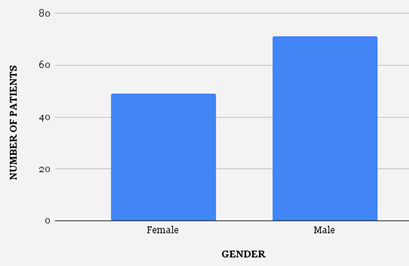
Figure 1: Gender distribution.
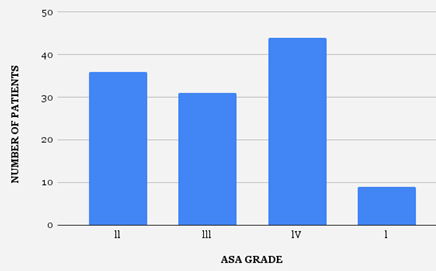
Figure 2: ASA grading distribution.
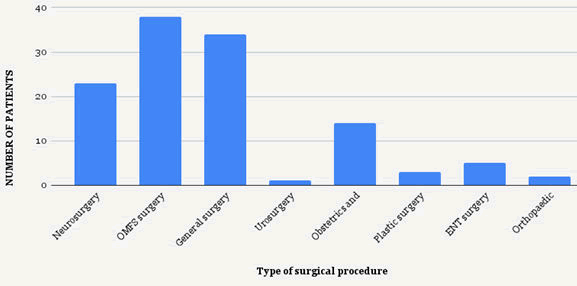
Figure 3: Various surgical procedures distribution.
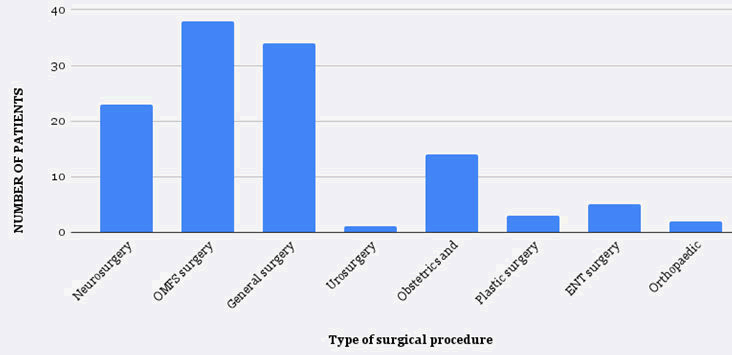
Figure 4: Co-morbid status distribution.
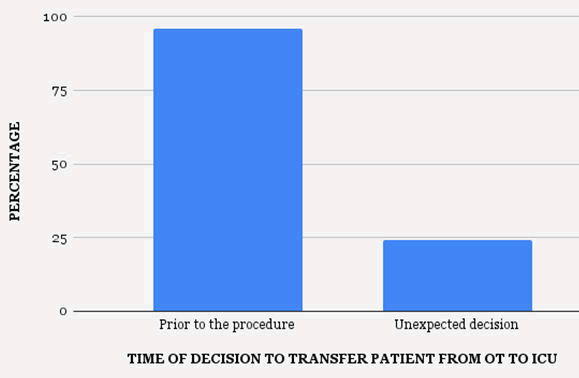
Figure 5: Time of decision distribution.
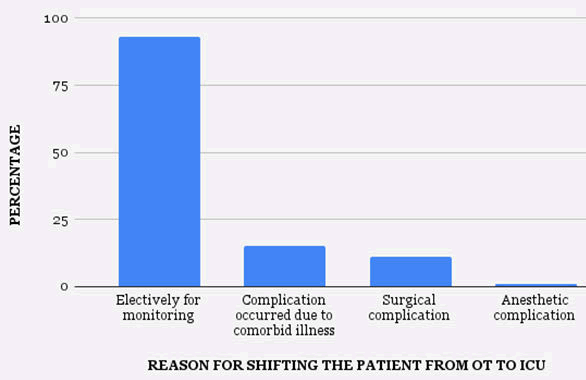
Figure 6: Reason for shifting to ICU distribution.
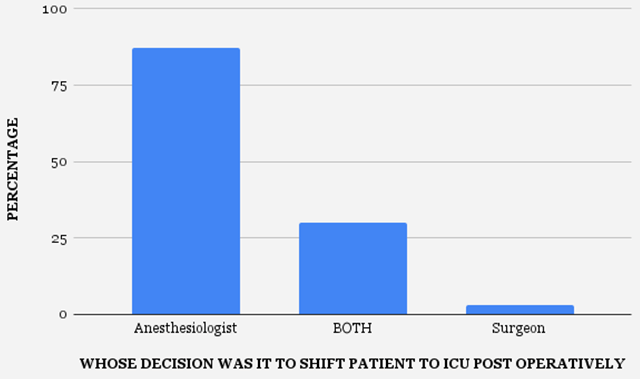
Figure 7: Team decision distribution.
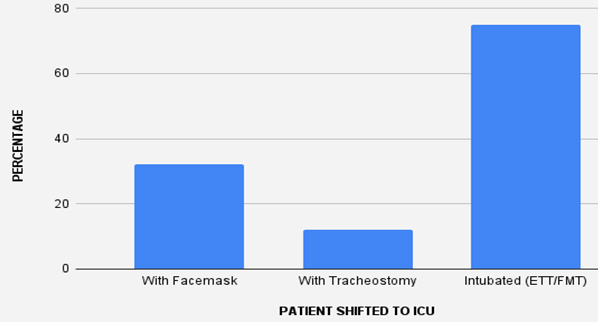
Figure 8: Airway usage in transit distribution.
The Intensive care unit is an important care unit reflecting the critical care involved in the hospital. The critical patients are monitored on various aspects continuously so to enhance the recovery and better the prognosis [7]. The availability of bed, financial burden are the major and most common setbacks encountered in ICU care [8]. In a similar study Young et al. showed the financial burden in ICU hindering ICU admission as a setback in treatment. The ASA grading prior to surgery plays an important role in anticipating the post-operative complications and also in planning the need of effective post-operative care. The study resulted with ASA grade IV subjects being most commonly shifted to ICU constituted to 44 (36.66%) subjects and least being Grade I with 9 (7.5%) subjects [9]. The decision of the team to shift to ICU prior to procedure was 96 (80%) and intraoperative decision was 24 (20%). Young et al. in their study showed a direct proportionality with high risk patient’s mortality and delay in transfer of patients.
In a study done on high-risk surgical population in UK showed poor triage of high risk individually lead to increase mortality. The age distribution in the study was maximum with subjects aged 60 years accounting to 20 (16.6%). Reported that mortality rate in ICU and the proportion to the standard mortality rate in patients who had been referred from other health centres to ICU is significantly higher. In our study the most common surgical procedures for which patient was shifted to ICU was orofaciomaxillary surgery procedures accounting for 38 (31.66%) subjects with least being urological procedures 1 (0.83%) [10]. Most common cause for patient transferring to ICU was trauma, especially, brain trauma. In an extensive study in more than 28 hospitals with 37 intensive care units, the patients had higher mortality compared to the patients with medical problems. Morales et al. conducted a study on 181 trauma patients in the intensive care unit, it was shown that over 84% of causes were road traffic, and in total, 30 patients died [11]. The results of on the patients in ICU mentioned that the most common cause of death was related to the nervous system and neurosurgical service had referred the most patients to the intensive care unit [12].
The decision in shifting the patient to ICU post operatively was maximum for elective monitoring 77.5% and least being anaesthetic complication 0.83%. The co-morbid status of the subjects in the study included hypertension 24 (20%) being most common, followed by Diabetes mellitus 14 (11.66%). The multiple co-morbid statuses of the subjects were of 5 (4.16%).
The airway related problems are most commonly expected hence it is most common to see the patient with head and neck surgeries are shifted out of operation theatre for ICU care. In similar studies showed relevancy in high risk patients admitted to ICU had increased mortality rates.
Citation: Shetti AN, et al . "The Evaluation of Factors Affecting on Patient Admission from Operating Room to Intensive Care Unit in Pravara Rural Hospital, Loni". Oncol Cancer Case Rep, 2023,9(1), 1-3.
Received: 04-Nov-2022, Manuscript No. OCCRS-23-85391; Editor assigned: 09-Nov-2022, Pre QC No. OCCRS-23-85391(PQ); Reviewed: 23-Nov-2022, QC No. OCCRS-23-85391; Revised: 02-Jan-2023, Manuscript No. OCCRS-23-85391(R); Published: 30-Jan-2023, DOI: 10.37532/23.9.1.001
Copyright: © 2023 Shetti AN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.