Case Report - (2021) Volume 0, Issue 0
Pseudopelade of Brocq (PPB) is a rare, chronic, and gradually progressive cicatricle alopecia that primarily affects middle-aged women. The vertex and parietal scalp are frequently involved. It can be primary or secondary to scarring alopecia’s such as lichen planopilaris and discoid lupus erythematosus. It is diagnosed clinically and trichoscopically by exclusion. There is no one-size-fitsall treatment for PPB. We present a case of rapidly progressing primary idiopathic Brocq pseudopelade of Brocq in a young female child, which was confirmed by trichoscopy and histopathology. Alopecia areata is non scarring alopecia while Pseudopelade of Brocq is scarring alopecia. Both these clinical entities can mimic each other. Here we present a case of Alopecia areata mimicking clinically as Pseudopelade of Brocq.
Alopecia areata • Puedopelade of Brocq • Trichoscopy • Histopathology
Alopecia areata is an autoimmune disorder characterized by transient, nonscarring hair loss and preservation of the hair follicle [1]. The characteristic lesions of alopecia areata are round to oval; smooth non scarring patch involving scalp or any other hair bearing area. Diagnosis of alopecia areata is usually clinical [2]. Sometimes histopathological examination is essential to decide the plan of therapy required [2]. Here we introduce a case of 14 year old female patient who presented with lesion clinically consistent with Pseudopelade of Brocq and histopathology of the same lesion consistent with Alopecia areata. It can be a single entity (primary) or the outcome of a number of scalp disorders, all of which result in scarring (secondary). It manifests as small patches of alopecia with mildto- moderate atrophy and no evidence of folliculitis or significant inflammation. We present a case of a young female child with rapidly progressing cicatricle alopecia with no known underlying cause, which was histopathologic ally confirmed to be PPB.
A 14 year old female patient presented with hair loss of 6 months duration. On physical examination she had polygonal, discrete to confluent, asymmetrical areas of hair loss. Tufted hair, discrete areas of scarring and footprint in snow appearance was present. There was no evidence of scaling and inflammation. On clinical basis probable diagnosis of Psedopelade of Brocq was made. Punch biopsy revealed morphological features consistent with Alopecia areata. Patient was treated with benison forte twice a week oral mini pulse for a month which resulted in dramatic improvement with reappearance of hair. Clinical presentation, histopathological finding and response to benison oral mini pulse led to the diagnosis of Alopecia areata. She first developed a lesion a year ago, but the disease has been rapidly progressing in the last six months. Her mother described how new lesions were constantly forming and how the size of older lesions was increasing. There had been no previous history of papules, pustules, or plaques. There had been no previous history of cutaneous or systemic illness. There were no other family members with a history of alopecia. On cutaneous examination, an irregular but well-defined confluent patch of hair loss over the vertex, resembling a footprint in snow, was found.
Palade is the French term for alopecia areata, which is derived from a word “pelage” meaning the fur, hair, wool, etc., of mammal [3].“Pseudo-plead” was first described by Neumann in 1869. Pseudopelade was named by a French dermatologist Louis-Anne-Jean Brocq in 1888 for its similarity to hair loss of alopecia areata [3,4]. Pseudopelade of Brocq is a chronic, insidious, primary lymphocytic cicatricle (scarring) alopecia. It is clinically characterized by multiple, small, discrete, asymmetrical, smooth, soft, flesh-toned or white alopecic patches with minimal or no inflammation. Three patterns of pseudopelade including scattered, large plaques, and a combination of both morphologies have been described. The parietal and vertex of the scalp are primarily involved (Figures 1 and 2) [4]. It usually occurs in middle aged white woman [2]. The classic description of “footprints in the snow” refers to lesioned depression caused by moderate dermal atrophy and by a reticulated pattern with small irregular patches (Figure 3). The initial smaller lesions evolve into larger alopecic patches with polycyclic borders. Hairs in patches may be scattered isolated or grouped and curly due to follicular distortion [4,5].
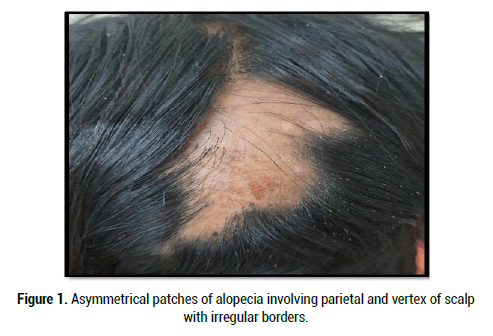
Figure 1:Asymmetrical patches of alopecia involving parietal and vertex of scalp with irregular borders.

Figure 2: Footprint in snow appearance and tufted hairs.

Figure 3: Improvement after 3 months of treatment.
Mainly two types of PPB are recognized.
• Burnt-out or end-stage scarring alopecia’s-Pathophysiology corresponds to underlying disease process. e.g., Lichen Planopilaris (LPP), Discoid Lupus Erythematosus (DLE)
• Primary idiopathic pseudopelade where pathophysiology is unknown [3].
Histopathologic ally decreased sebaceous glands, wide spread scarring of intermolecular dermis with minimal lymphocytic infiltrate is noted. Epidermis is usually normal with rarely fibrotic stream extending to sub cutis. Alopecia areata is a common type of hair loss or alopecia in humans; it is an autoimmune disease with typically relapsing or remitting, course. Alopecia areata is the second-most frequent non-scarring alopecia, after male and female pattern alopecia [1]. clinical patterns range from patchy alopecia, reticulate alopecia, ophiasis, ophiasis inverses (sisaphio), and alopecia total is or alopecia universal [6]. Although diagnosis is clinical, skin biopsy is sometimes needed to distinguish alopecia areata from other types of alopecia [4]. Alopecia areata is a dynamic disease that is reflected in its histopathologic features [1].The histopathological features are described in 4 classical phases of the lesions: acute hair loss, persistent alopecia, partial telegenic to antigen conversion and recovery [7]. The earliest and most important feature in the acute phase is the per bulbar lymphocytic infiltrate, rarely extend into the epithelium and hair matrix. In later stages, the inflammation may be diminished or absent. In such cases histopathological diagnosis is relied on the presence of eosinophils near hair bulbs and fibrous tracts [8]. In our case, clinical presentation was consistent with Pseudopelade of Brocq showing patchy alopecia with scarring and presence of footprint on snow appearance. But histopathological diagnosis was suggesting alopecia areata. Also, clinical improvement with reappearance of hair with prednisolone oral mini pulse therapy further supported the histopathological diagnosis.
Pseuopelade of brocq and alopecia areata are mimickers of each other. Though diagnosis is clinical in both the cases, clinical picture may be confusing. Histopathological examination helps in deciding line of management in such cases. PPB can, although infrequently, affect children. Proper evaluation with trichoscopy and biopsy at the effective time can help reduce unnecessary topical steroid treatment, and the patient can be advice about the progression of disease.
Citation: Manwar P, et al. Pseudopelade of Brocq: A Caricature of Alopecia Areatas. Med Rep Case Stud, 2021, 06(S5), 023-024
Received: 15-Nov-2021 Published: 06-Dec-2021
Copyright: © 2021 Manwar P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO