Case Report - (2023) Volume 9, Issue 2
Background: Primary peritoneal carcinoma is epithelial tumor. Histologically, the most common type is primary peritoneal serous carcinoma, which almost occurs in women. Another rare subtype is Primary Peritoneal Mucinous Adenocarcinoma (PPMA). To date, only few cases of PPMA occurring in male patient have been published in English literature. Here we described another rare case of primary peritoneal mucinous adenocarcinoma in a male patient.
Case presentation: We report an 82 years old male patient with the chief complaint of abdominal pain for more than a month without associated symptoms of nausea, vomiting, ascites, and weight loss. Peritoneal cytology and immunohistochemistry reported peritoneal carcinoma of intestinal origin. The patient underwent laparotomy and a primary peritoneal tumor with metastasis to the right colon and mesentery was found. Postoperative histopathology showed the primary peritoneal mucinous adenocarcinoma.
Conclusion: Primary peritoneal mucinous adenocarcinoma is an extremely rare malignancy and has a very poor prognosis. Its delayed diagnosis and management can warrant to complications such as bowel obstruction.
Primary peritoneal mucinous adenocarcinoma • Peritoneal cytology • Laparotomy • Immunohistochemistry • Bowel obstruction
Primary peritoneal carcinoma is a rare intra-abdominal carcinomatosis, involving the peritoneum and omentum. It can affect both men and women. There are different subtypes of primary peritoneal carcinoma. The most common type is Primary Serous Papillary Carcinoma (PSPPC). Other less common types are clear-cell carcinoma, endometrioid adenocarcinoma, and mucinous adenocarcinoma. PSPPC is a well-known entity in women and is histologically similar to ovarian papillary carcinoma.
It is classified as low and high-grade primary peritoneal serous carcinoma. Primary peritoneal carcinoma is diagnosed and treated the same way as ovarian carcinoma.
The first case of PSPPC in women was described by Swerdlow in 1959 [1]. To our knowledge, there have been only a few cases reported as primary peritoneal serous carcinoma in men. Primary peritoneal mucinous adenocarcinoma is a very rare tumor with only two cases available in the literature. The first case was published by Wang et al in 2018 in a female patient [2], while the second case was reported in 2021 by Fumiko et al in a male patient. [3]. In this report, we present the third case of the primary peritoneal mucinous adenocarcinoma in 82 years old man.
An 82 years old, Chinese man with a past medical history significant for Chronic Obstructive Pulmonary Disease (COPD) for more than 40 years, hypertension grade 3 for one year, and coronary heart disease for about 10 months. He also had a surgical history of benign prostatic nodules for 10 years. There was no history of blood transfusion, tuberculosis, and hepatitis, but there was a history of exposure to asbestosis as labor for about 25 years. The patient first time presented to the gastrointestinal oncology department with a chief complaint of intermittent abdominal pain for more than 1 month. The pain was sudden in onset with recurrent attacks. He had no fever, nausea, vomiting, ascites and weight loss. The physical examination revealed no abdominal distension or tenderness. The following tumor markers were performed. CA125: 99.57 U/ml (normal 0-30.2), CA19-9: 9.80 U/ml (normal 0-37), CEA: 355.81 ng/ml (normal 0-5), AFP: 4.13 IU/ml (normal 0-6.7), CA72-4: 9.41 U/ml (normal 0-6.9), CYFRA21-1: 3.72 ng/ml (normal 0-3.3). The abdominal and pelvic CT scan showed rectal wall thickening and multiple peritoneal nodules. Gastroscopy showed superficial gastritis, gastric polyps, and a duodenal ulcer. Colonoscopy findings were chronic colitis and colonic polyp. On the 3rd day of admission, a CT-guided percutaneous peritoneal biopsy was performed, microscopic mesothelial cells in fibrous adipose tissue were extracted, and immunohistochemistry was advised. The Immunohistochemical stains were positive for AE1/AE3(+), Calretinin (-), CK5/6(+), WT1(-), positive for cytokeratin CK20(+), CDX2(+), SATB2(-), CK7(+), but negative for Thyroid Transcription Factor TTF-1(-), PSA (-), TG (-), VILIN (+), gastric foveolar cell mucin MUC5AC (+) and intestinal goblet cell type mucin MUC2(+) were positive, Ki-67(50%).The immunohistochemistry results point out the adenocarcinoma of intestinal origin. He was discharged with a suspicious diagnosis of peritoneal carcinoma. After one week the patient was admitted to our department for further evaluation and management of the same chief complaints. The vital signs were BP: 158/101 mmHg, RR: 16/ min, PR: 72/min, temperature: 39â??, and SpO2: 98%. On physical examination, the abdomen was soft and non-tender without any palpable mass. Bowel sounds were audible and normal. The blood investigations showed TLC: 5.10 (normal 3.50-9.50), Hb: 15 g/dl (13.0-17.5), PT: 13.30 s (normal 11-14.5), APTT: 32.70 s (normal 26-43), INR: 0.99 (normal 0.8-1.5), ALP: 74.30 U/L (normal 45-125), ALT: 19.20 U/L (normal <50), AST: 31.20 U/L (normal 15.00-46.00), Alb: 37.30 g/L (normal 35-50), GGT: 17.50 U/L (normal 12.0-58.0), glucose: 4.96 mmol/L (normal 4.1-5.9), Urea: 5.40 (normal 3.2-7.5), serum creatinine: 80.20 µmol/L (normal 58-110), serum calcium: 2.17 mmol/L (normal 2.1-2.6), and blood group A positive; the HbsAg, anti-HCV Ab, and HIV tests were negative. A CT thorax was also performed, which revealed mediastinal and multiple bilateral hilar lymph nodes. After the complete investigations and pathology report, the diagnosis of peritoneal carcinoma was suspected. The patient underwent laparotomy. Intraoperative findings were: extensive peritoneal nodules, and numerous metastasis to the omentum, mesenteric root, and right colon (Figure 1). There was also some structure noted in the right colon. Firstly, peritoneal dissection and right hemicolectomy was performed. The mesenteric lymph nodes were removed as much as possible. Then, the ileocecum and peritoneum of the right ascending colon were incised along the right paracolic sulcus.
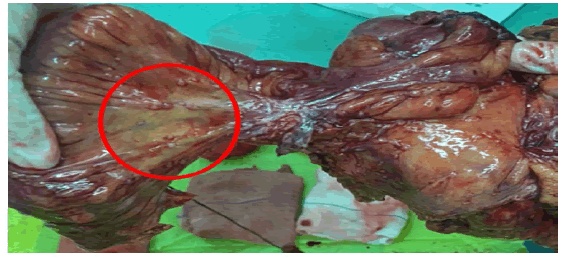
Figure 1: Surgical specimen: revealed a peritoneal tumor with multiple lymph nodes (red circle) found on omentum.
The right part of the gastrocolic ligament and the right portion of the transverse mesocolon was resected. The ileum and transverse colon were end-to-side anastomosed with a circular stapler and sutured with a seromuscular layer. Abdominal lavage with warm normal saline was done and two drainage tubes were placed near anastomosis and in the abdominal cavity. We performed Cytoreductive Surgery (CRS) and right hemicolectomy to minimize the risk of future bowel obstruction. Although some residual cancer nodules remained, but mostly nodules were removed along omentum, then specimen was sent for histopathology. The postoperative histopathology showed that there were multiple nodules on the surface of the right colon, appendix, and small intestinal mesentery, with a diameter of 0.1 cm-0.2 cm. Multiple omental nodules were found with a diameter of 4 cm-13 cm. Moderately differentiated adenocarcinoma was seen in the omentum, mesocolon, small intestine, and serosa of the appendix. Some of them were mucinous adenocarcinoma (Figures 2 A and 2B). Most of the cancer tissue was located in the omentum, and no primary lesion was found in the colon and appendix. Combined with the pathological diagnosis and immunohistochemical results, and after the imaging examination ruled out metastatic cancer, the patient was diagnosed with primary peritoneal mucinous adenocarcinoma. After the operation, the patient received routine antibiotics and postoperative treatment. On the 6th postoperative day, the patient passed the flatus, and bowel sounds were positive on auscultation. So, a soft diet was started. After 18 days, the patient’s symptoms improved significantly, the drains were removed and was subsequently discharged. At a 1-month follow-up after hospital discharge, the patient recovered well without any gastrointestinal discomfort.
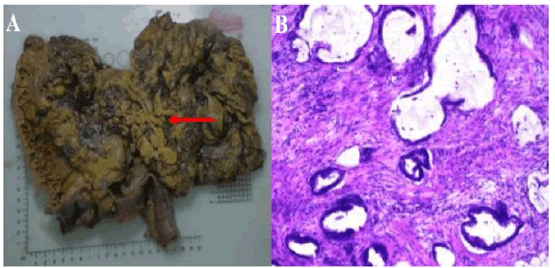
Figure 2: (A) The gross photograph reveals cut section of peritoneal tumor mass (red arrow) along with right colon and omentum. (B) Microphotograph showing neoplasm consisting of multiple mucinous epithelium.
Peritoneum is a serosal membrane that covers the abdominal cavity, forms mesenteries, and also covers the abdominal and pelvic viscera. Peritoneal carcinoma can originate from peritoneal tissue that is primary peritoneal carcinoma or secondary peritoneal carcinoma if metastasis to the peritoneum of the adjacent organs. Primary Peritoneal Carcinoma (PPC) is an extremely rare neoplasm, histologically the origin of this resembles epithelial ovarian carcinoma [4].The first published case of primary peritoneal adenocarcinoma was by Swerdlow in 1959 [1]. Primary peritoneal mucinous adenocarcinoma can also be known as: Pseudomyxoma Peritonei (PMP) or Disseminated Peritoneal Adenomucinosis (DPAM) of unknown origin [5-7]. In fact, primary peritoneal carcinoma predominantly occurs in menopausal and post-menopausal women. In addition, women with a higher risk of ovarian cancer also have an increased risk of peritoneal carcinoma [8]. In general, neoplasms of the unknown primary site usually consider being metastatic, whose primary tumor cannot be identified despite thorough examination. [9, 10].The primary peritoneal neoplasms are classified as malignant mesothelial tumors, epithelial tumors, smooth muscle tumors, and tumors of uncertain origin [11-13]. The most common type of primary peritoneal carcinoma is primary serous papillary peritoneal carcinoma [14, 15]. Other subtypes such as mucinous adenocarcinoma and clear-cell carcinoma and endometrioid adenocarcinoma are very rare [16, 17].The mucinous adenocarcinoma usually occurs in the vermiform appendix, pancreas, stomach, colon, ovary, lung, and breast [18]. Primary serous peritoneal carcinoma in females has histopathological similarities with ovarian carcinoma, which is divided into high and low grade serous carcinoma. Most of the cases of PSPPC in men also follow the same classification [13, 14]. The diagnosis of primary peritoneal mucinous adenocarcinoma preoperatively is often very challenging, due to clinicopathological similarities with serous ovarian carcinoma. The diagnosis of PSPPC usually depends on the criteria of the Gynecologic Oncology Group published in 1993[19]. Peritoneal mesothelioma might be clinically different from PSPPC, and can be divided into three pathological subtypes: malignant mesothelioma, cystic mesothelioma, and Desmoplasmic Small Round Cell Tumor (DSRCT) [20]. Malignant peritoneal mesothelioma is a rare neoplasm but a very aggressive tumor in nature. The possible etiology of peritoneal malignant mesothelioma is related to carcinogens such as asbestos exposure, while some other etiologies are also been reported such as abdominal therapeutic radiation and peritonitis [21, 22]. Moreover, it is more common in men. In this case, the patient has a history of asbestosis exposure and worked in a factory for about 25 years. Cystic mesothelioma; a type of peritoneal mesothelioma found a rare tumor in the surfaces of the pelvis. Typically, these neoplasms consist of multiple grapes-like clusters of mesothelium-lined cysts [23]. Some data reported intraperitoneal chemotherapy was very effective in this subtype, but no clinical study determined the long-term prognosis. Desmoplasmic small round cell tumor DSRCT is a highly aggressive cellular tumor that mostly occurs in young adults. It invades the peritoneal surfaces with the hematogenous route to the liver, and lungs. In addition, the immunohistochemical profile in this tumor is characterized by CD56, vimentin, and myogenic (desmin maskers) [23]. In the literature, there are a total of 9 cases of primary serous and mucinous carcinoma of the peritoneum [1-3,14,24-26] which include only one case of primary peritoneal mucinous adenocarcinoma occurred in women as shown in Table 1. In primary peritoneal carcinoma the hereditary predisposition may play an important role; such as patients with BRCA1/2 mutations have an increased risk of malignancy. While some environmental factors, such as carcinogens, most commonly asbestos also play a role. Moreover, simian virus 40 has been also reported as a main etiological factor, however, the evidence is not strong. [27] The peritoneal malignancies are usually asymptomatic in the initial stage, but with progressive involvement of the peritoneum the most common clinical symptoms are abdominal distension with ascites, abdominal pain, gastrointestinal symptoms (loss of appetite, nausea, and change in bowel habits). On physical examination, the most common presentation is increased abdominal girth, abdominal tenderness, and abdominal mass [28, 29]. Although, in our current case the only main clinical presentation was severe intermittent abdominal pain for the last one month. In the previous reviews, some patients with peritoneal carcinoma secondary to colorectal malignancy also presented with bowel obstruction [30]. Peritoneal carcinoma complications include small bowel obstruction, blockage of the ureter by tumor, and shortness of breath due to malignant pleural effusion. The use of tumor markers may help, the serum level of CA125 in most patients of peritoneal carcinoma is elevated prior to treatment. Similarly, in this case, the CEA, and CA 125 were elevated. The Immunohistochemical (IHC) stains play an important role in differentiating peritoneal carcinoma from mesothelial lesion. On occasion, the carcinoma of the peritoneum usually shows the same histological characteristics as malignant mesothelioma. In our case, the origin of peritoneal carcinoma was confirmed by IHC. The tumor marker for cytokeratin 7 and cytokeratin 20 were positive. The CK7/CK20 expressions are very useful for differentiating the colorectal origin from none intestinal origin [31, 32]. The focal positive for CDX2. Mucinous tumors of appendiceal and ovarian origin usually express on CDX2 and CK20 [33-35]. Interestingly, these markers are identical to the markers of this primary peritoneal mucinous adenocarcinoma. The mucin core protein MUC2, MUC5AC, and Villin were also positive. Initially, these findings were suggestive of the carcinoma of intestinal origin. the Therefore, preoperative clinical symptoms and intraoperative findings also have an important role in out diagnosis of PPMA.Standard imaging studies, including ultrasound and the Abdominal-pelvic CT is the investigation of choice to assess the peritoneal malignancy but cannot be used to accurately rule the diagnosis. To rule out mesothelioma extensive calcification and omental caking is useful finding on CT scan. It often demonstrates ascites and nodules. The reported sensitivity of CT ranges from 25 to 96% for the detection of peritoneal carcinoma [36, 37]. The imaging findings between infiltrating tumors or focal tumors appeared as stellate or pleated characteristics. Some studies showed that Magnetic Resonance Imaging (MRI) is superior to CT scan. However, Fluorodeoxyglucose (FDG)-Positron Emission Tomography (PET) can also be used to diagnose peritoneal carcinomatosis [38]. So Preoperative imaging and immunohistochemical stains play important role in determining peritoneal carcinoma. In this case, the preoperative diagnosis was based on immunohistochemical stains and peritoneal associated with cytology. poor Peritoneal prognosis carcinomas are generally in patients with colon adenocarcinoma. The overall prognosis of peritoneal carcinoma is very poor with a prognosis rate of 6 months [39].For the management of peritoneal carcinoma the surgery alone is not adequate. The intraperitoneal chemotherapy can be administered intraoperatively and early and late postoperatively.
Table 1. All reported cases of primary serous and mucinous peritoneal carcinoma
| Name and year of publication | Age (yrs) and Gender | Clinical presentation | Type of peritoneal carcinoma |
|---|---|---|---|
| I.A. Shah et al 1998 | 74/man | Abdominal distension | Papillary serous carcinoma of the peritoneum |
| E. Shmueli et al 2001 | 53/man | Abdominal pain, abdominal distension | Primary papillary serous carcinoma of the peritoneum |
| Canbay et al 2013 | 63/man | Not reported | Primary peritoneal serous carcinoma |
| Jin Xu et al 2017 | 58/man | Abdominal pain | Primary peritoneal low-grade serous carcinoma |
| Yuan J et al 2017 | 62/woman | Abdominal distension, nausea and vomiting | High-grade primary peritoneal papillary serous Adenocarconoma |
| V.V.Makarenko et al 2020 | 59/man | Asymptomatic but on CT Ascites | Low-grade primary peritoneal serous carcinoma |
| A.Guellil et al 2022 | 77/man | Abdominal pain | Primary peritoneal high-grade serous carcinoma |
| Wang et al 2018 | 49/woman | Abdominal and back pain, Anorexia | Primary peritoneal mucinous adenocarcinoma |
| Fumiko et al 2021 | 69 /man | Abdominal distension | Primary peritoneal mucinous adenocarcinoma |
| Current study | 82/man | Abdominal pain | Primary peritoneal mucinous adenocarcinoma |
The effect of intra-peritoneal chemotherapy has been depending on the following conditions such as the general condition of the patient, absence of metastasis, lysis of intra-abdominal adhesions, minimal residual disease after cytoreductive surgery, large volume carrier solution, and adequate drug choice [40, 41]. The intraperitoneal chemotherapy method is divided into closed and open intraoperative techniques commonly termed “the coliseum technique” described by Sugarbaker [42, 43]. Cytoreductive surgery is mainly for the removal of the macroscopic peritoneal tumor [44]. In this current case, the primary peritoneal tumor along with the omentum and right colon was resected, for prevention of bowel obstruction in the future. In the previous report by Wang at el, the patient postoperatively was diagnosed with peritoneal adenocarcinoma that presented with the complication of bowel obstruction which might have been due to metastasis to colon [2]. When treating the intraperitoneal lesion, the Cytoreductive Surgery-: Hyperthermic Intraperitoneal Chemotherapy (CRS-HIPEC) are more effective compare to systemic therapy and showed a high survival rate [45].Cytoreductive surgery plus heated intraperitoneal chemotherapy is a useful therapeutic option for patients with peritoneal carcinomatosis from colon carcinoma and pseaudomyxoma peritonei. A complete cytoreductive surgery is the cornerstone of curative treatment [46]. Peritoneal carcinomatosis description on peroperative can be evaluated by different types of staging systems such as the Gilly PC Staging System (GSS), Sugarbaker Peritoneal Center Index (PCI), the Dutch simplified PCI, and Japanese PC staging system. [47]. The Gilly staging system was first described in 1994 [48]. According to Gilly peritoneal carcinomatosis staging system, the median survival rate for stage 1 and stage 2 is 16 months, while for stage 3 and stage 4 is about 6 months [49]. The peritoneal cancer index is based on the size and spreading of the peritoneal metastasis in 13 defined regions, while the Dutch region count is based on the division of the abdomen in 7 regions [50]. Peritoneal Cancer Index (PCI) measures the size and extent of the peritoneal tumor. Sugarbaker reported patients with carcinomatosis from colon carcinoma to have a 50% survival rate if the PCI was less than 10, but PCI of 11-20 have 20% while PCI>20 has a 0% 5 year of survival rate [51, 52]. Japanese surgeons presented intraperitoneal chemo-hyperthermia in 1984 [53]. The most reliable determinants for the resectability of peritoneal carcinomatosis deposits are; the Peritoneal Cancer Index (PCI), Complete Cytoreductive Surgery (CRS-R0), and the estimation of postoperative quality of life[54, 55]. Moreover, compare with other staging systems Gilly and PCI are the most accurate methods for peritoneal carcinomatosis [56]. In this reported case, the preoperative colonoscopy and endoscopy confirmed that the stomach and large intestine were not the primary sites of peritoneal mucinous adenocarcinoma. Thus, based on immunohistochemistry, surgical findings, and histopathological examination, the patient was finally diagnosed with primary peritoneal mucinous adenocarcinoma.
Primary Peritoneal Mucinous Adenocarcinoma (PPMA) is an extremely rare malignancy. It poses both diagnostic and therapeutic challenges to surgeons, and warrants the complication of bowel obstruction which may be due to a primary or secondary infiltrating tumor. Delays in diagnosis and management can warrant high morbidity and mortality. By virtue of their rarity, each case of PPMA should be reported to add evidence in the literature and aid future-generation surgeons to manage this rare entity accordingly .
Ethical approval and consent to participate
The study protocols were approved by the Ethical Committee of the Second Affiliated Hospital of Dalian Medical University .
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that they have no competing interests.
Funding
All authors have no sources of funding.
Author contributions
SF and FL collected the data, conducted the literature search and wrote the paper. YL, LL, ZC, MW and HD took care of the patient. SN and YL performed the operation. FL, SN, and SF revised the manuscript. SF and FL contributed equally to the work and should be regarded as co- first authors. All authors read and approved the final manuscript.
We acknowledge the contribution of the Department of General Surgery of the Second Hospital of Dalian Medical University for making all resources available and providing the technical support needed for the completion of this article .
[Google Scholar] [Cross Ref]
[Google Scholar] [Cross Ref]
[Google Scholar] [Cross Ref]
[Google Scholar] [Cross Ref]
Citation: Luo, F, et al. Primary Peritoneal Mucinous Adenocarcinoma: A Rare Case and Literature Review, Oncol Cancer Case Rep. 2023, 9(2), 1-5
Received: 18-Mar-2023, Manuscript No. OCCRS-23-92221; Editor assigned: 20-Mar-2023, Pre QC No. OCCRS-23-92221 (PQ); Reviewed: 22-Mar-2023, QC No. OCCRS-23-92221 (Q); Revised: 25-Mar-2023, Manuscript No. OCCRS-23-92221 (R);; Published: 31-Mar-2023, DOI: 10.35248/23.9.2.1-5
Copyright: ©2023 Luo, F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : All authors have no sources of funding.