Case Report - (2021) Volume 7, Issue 8
Multiple extramedullary plasmacytoma concurrent with multiple bony plasmacytoma is very rare presentation and thorough investigations are required to exclude multiple myeloma in these patients. Close follow up is required in these patients as they may present with new lesions with dismal prognosis. We present a case of multiple plasmacytoma with aggressive cutaneous involvement, which is a very rare presentation. Treatment with alkylating chemotherapy reduces tumor bulk. However, the risk of progression to multiple myeloma being not yet documented should always be kept in mind.
Extra medullary • Plasmacytoma • Multiple myeloma • Dismal prognosis
Multiple solitary plasmacytoma (MSP) is defined as a monoclonal plasma cell infiltrate in one or more lytic bone lesions (often spreading to the surrounding soft tissues) associated with no evidence of plasma cell proliferation on random bone marrow biopsy and without systemic abnormalities typical of MM (e.g. hypercalcaemia, anaemia, renal failure, serum and/or urinary monoclonal proteins or monoclonal light chains).
Extramedullary solitary plasmacytoma (EMP) presenting as a soft tissue mass in more than one site is therefore a very rare event. 90% of EMP cases develop in the head and neck area especially in the upper respiratory tract, including nasal cavity and sinuses, nasopharynx and larynx. Infrequent sites of involvement include the gastrointestinal tract, liver, spleen, pancreas, lungs, thyroid, breast, testis or skin.
Cutaneous Plasmacytomas are monoclonal neoplasms of plasma cells, usually associated with multiple myeloma, resulting either from direct spread from underlying connective tissue focus or from the haematogenous metastatic spread [1]. Very few cases of primary cutaneous plasmacytoma have been reported in the literature thus far. Lesions typically present as slow-growing, reddish brown macules or plaques on the face, trunk, or extremities. They may be single or multiple, though solitary lesions are thought to portend a better prognosis [2].
We present here a case report of a 55-year old male having multiple solitary plasmacytoma with aggressive cutaneous manifestation.
We present here a case report of follow up case of solitary plasmacytomas of the left orbit concurrent with scalp and left chest wall plasmacytoma in a 55-year old male whose thorough initial diagnostic workup was negative for multiple myeloma and showed complete resolution of disease with non-conventional treatment that is oral chemotherapy in the form of tab melphalan and thalidomide. Patient lost to follow up for 9 months and presented in emergency department with complaints of pain, swelling and one nodule over the left forearm. X-ray left upper arm showed fracture of ulna (Figure 1). MRI of left forearm arm revealed left ulnar proximal diaphysis large destructive lesion with extensive soft tissue malignant mass with multiple neoplastic bony lesions (Figure 2). He was managed with excision of lump followed by fibular bone graft with ulnar plating in orthopedics department. Excisional biopsy was consistent with plasmacytoma.

Figure 1: X-ray left upper arm showed fracture of ulna.
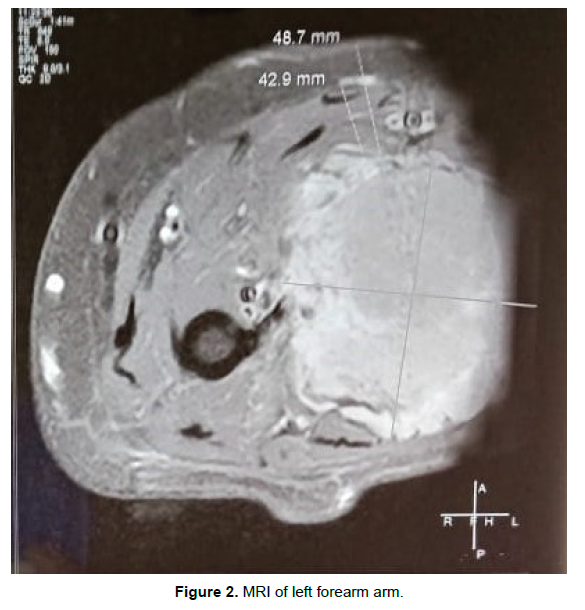
Figure 2: MRI of left forearm arm.
Patient again underwent thorough diagnostic workup to rule out multiple myeloma. Bone marrow aspiration was done and found to be with in normal limit. Quantitative serum electrophoresis was also normal. Urine B J protein was absent. MRI spine showed compression of D1 vertebra (Figure 3). X-Ray chest (PA view) showed fracture of right clavicle (Figure 4). Though patient was asymptomatic but in view of multiple bony lesions, Bone scan was done, which was in favour of multiple focal involvement of nearly all bones (Figure 5).
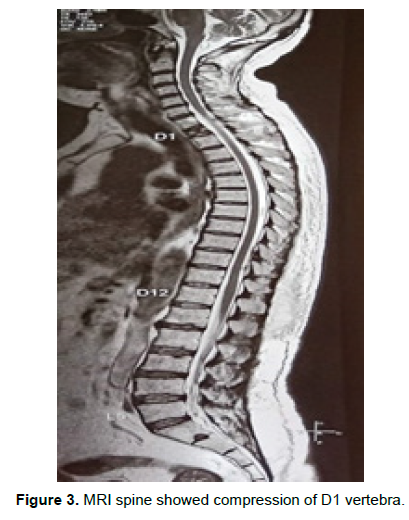
Figure 3: MRI spine showed compression of D1 vertebra.
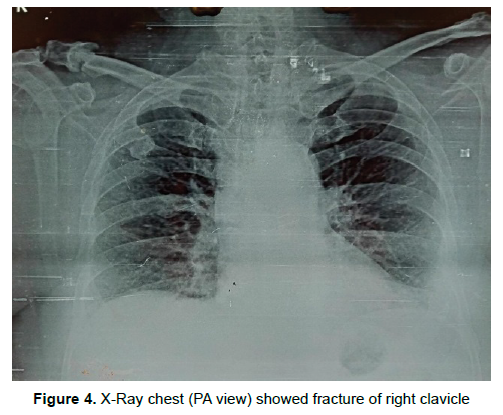
Figure 4: X-Ray chest (PA view) showed fracture of right clavicle.
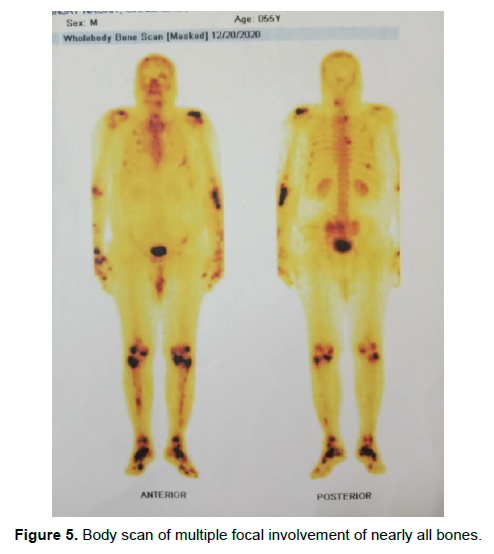
Figure 5: Body scan of multiple focal involvement of nearly all bones.
Patient was restarted on tab thalidomide 100 mg 1 OD and inj zolidronic acid 4 mg I/V monthly but disease was progressive and after 2 wks., patient presented with multiple cutaneous nodules over the left forearm with complaints of itching and burning pain over the skin nodules (Figure 6). FNAC of these nodules was in favour of plasmacytoma (Figure 7). IHC was advised but patient denied due to financial constraint. Patient’s hemoglobin levels. Calcium level and renal function test and liver function tests were all with in normal limit. Patient has been put on VAD regimen (inj vincristine, inj Adriamycin and inj dexona) and local radiotherapy of 30Gy/10# was delivered to C7 and D1 vertebra.

Figure 6: Multiple cutaneous nodules over the left forearm.
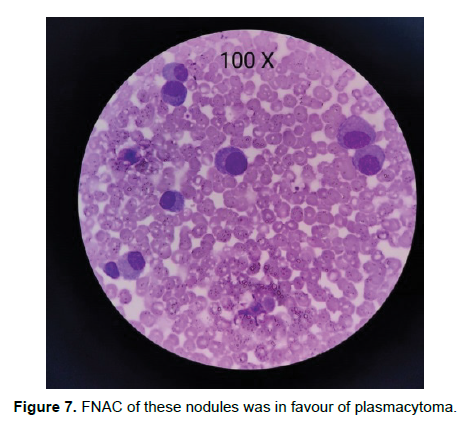
Figure 7: FNAC of these nodules was in favour of plasmacytoma.
The International Myeloma Working Group in 2003 classified plasmacytomas as solitary plasmacytoma of bone (SBP) when a single bone lesion was present, solitary extra medullary plasmacytoma(SEP) when a solitary soft-tissue lesion was present and multiple solitary plasmacytoma (MSP) when multiple sites of disease were present in soft tissue, or both [3]. SBP, SEP and MSP are rare clinical entities, characterized by a monoclonal plasma cell infiltrate in bone or soft tissue, cytologically and immune phenotypically identical to multiple myeloma (MM). EMP occurs predominantly in males at the ratio of 3:1. The majority of patients affected are between 50 and 70 years of age. The incidence of these entities is 0.35/100 000/ year, representing 5-10% of all plasma cell neoplasms [4].
The criteria to diagnose MSP includes monoclonal plasma cell proliferation involving one or more lytic lesions of bone often spreading to the adjacent soft tissue, without evidence of bone marrow involvement on a random iliac crest bone marrow biopsy, and absence of evidence of end organ damage (hypercalcemia, renal failure, anemia, monoclonal proteins in the urine/serum or monoclonal light chains) [5]. Primary extra medullary plasmacytoma is an extremely rare condition with an incidence of 2-4% of extramedullary cases. To establish this diagnosis, it requires absence of MM and plasmacytomas in other organs [6].
Skin manifestations in MM can be classified into three categories:
1) Primary extramedullary plasmacytoma
2) Cutaneous plasma cell neoplasm in the setting of previously diagnosed MM
3) Cutaneous plasma cell neoplasm from direct extension of osteolytic lesions in MM [7].
Cutaneous plasmacytoplasma can occur from hematogenous spread or infiltration of plasma cells from adjacent structures such as bones. It usually occurs in patients with aggressive or highly progressive form of MM and can be divided into primary and secondary. Primary cutaneous extra medullary plasmacytoma is when plasma cells infiltrate skin without the involvement of bone marrow. Secondary cutaneous extra medullary plasmacytoma can occur from metastasis from MM or from primary extra medullary plasmacytoma of other tissues [8,9].
Histopathologically, cutaneous plasmacytomas are divided into two types namely, nodular and diffuse [10]. It is a very rare condition with incidence of 1.9% [11]. Skin plasmacytomas manifest as reddish, violaceous, non-tender dermal or subcutaneous nodules, and sometimes may also appear as diffuse erythematous rash [12]. Most common sites for cutaneous manifestations are chest (44%), lower extremities (24%), back and buttock (22%), face and neck (20%), and upper extremities (18%) [13].
In our patient, establishing the proper diagnosis was a challenge as patients was not having any systemic sign of multiple myeloma. Patient was having bony plasmacytoma over multiple sites concurrent with multiple extramedullary plasmacytoma. All the investigations for establishing diagnosis of multiple myeloma was negative. Though bone scan showed multiple bony lesions but these were osteoblastic type. Our patient developed multiple cutaneous nodules over the forearm within very short span. These subcutaneous nodules were overlying the bony lesion of left ulna. Though alkylating agents shows good results but in this case disease was not responding to these agents and thus carries a very bad prognosis.
Multiple solitary plasmacytoma of different sites with no systemic involvement at present may be the first of its kind to be reported to the best of our knowledge. However, the risk of progression to multiple myeloma being not yet documented, should always be kept in mind, mandating a close follow-up of these patients.
Citation: Gupta S, et al. Multiple Solitary Plasmacytoma with Cutaneous Manifestation: An Unusual Presentation - A Case Report. Oncol Cancer Case Rep. 2021, 07 (8), 001-003.
Received: 04-Aug-2021 Published: 27-Aug-2021
Copyright: © 2021 Gupta S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.