Case Report - (2022) Volume 8, Issue 5
Medullary Thyroid Carcinoma (MTC) is a rare tumor of Para follicular cells of the thyroid gland. It can occur sporadically or maybe inherited as a component of MEN syndromes. When diagnosed during pregnancy, the timing of surgery is essential since maternal thyroxin is vital for fetal nervous system development. A 34 years old pregnant woman was diagnosed with MTC at her 17th week of pregnancy. Her Calcitonin level was elevated, while her CEA level was average. She underwent total thyroidectomy with a total lymph node dissection during the second trimester of pregnancy. After surgery, her calcitonin level dropped to the normal range. Levothyroxine treatment had initiated right after the surgery to prevent fetal complications. Calcium and active vitamin D3 supplementation were added. The patient gave birth to a term healthy infant. With this case report, we aim to share our experience in managing MTC in a pregnant woman till the birth of the infant.
Surgery • Endocrine malignancy • Parafollicular cells
Thyroid carcinoma is the most common endocrine malignancy in reproductive age women. About 10% of thyroid carcinomas are diagnosed during pregnancy [1]. Thyroid nodule evaluation in pregnant women is similar to nonpregnant adult examination. Ultrasound can be helpful for the physician to suspect carcinoma, and a fine needle biopsy can reveal the histological characteristics of the nodule. Thyroid carcinomas can be classified into two histological subtypes, which are differentiated thyroid carcinoma and the medullary variant. When the population base studies are considered, differentiated thyroid carcinoma usually has a better prognosis while the medullary variant has more aggressive features [2].
Medullary Thyroid Carcinoma (MTC) is a rare tumor of Para follicular cells of the thyroid gland. It can occur sporadically or maybe inherited as a component of MEN syndromes. MTC can be cured with total resection of the thyroid gland and the metastatic foci. When diagnosed during pregnancy, the timing of surgery is essential since maternal thyroxin is vital for fetal nervous system development [3,4]. On the other hand, high thyroxin levels must be avoided to prevent cancer spread.
With this case report, we aim to share our experience in managing MTC in a pregnant woman till the birth of the infant.
A 34 years old pregnant woman with a history of thyroid nodule was admitted to our clinic. She was in her 17th week of pregnancy. Thyroid-stimulating hormone and thyroxin levels were at a normal range, consistent with pregnancy. Ultrasound examination of the thyroid gland revealed a hypo echoic nodule (size: 12 x 12 x 14 millimeters) with foci of micro calcification in the right thyroid lobe and multiple cervical lymphadenopathies (the size of the largest lymph node 15 x 15 x 16 millimeters) (Figure 1). A fine needle biopsy was performed to identify the suspected nodule and lymph node. Fine-needle aspiration calcitonin washout was performed from the malignant lymph node (calcitonin level of 1650 ng/l). Pathological examination of the biopsy showed medullary thyroid carcinoma. The laboratory examination revealed an increased calcitonin level of 792 ng/L and a normal carcinoembryonic antigen level of 4,2 microgr/L. Once she had been diagnosed with MTC, further evaluation was planned to decide whether the disease had occurred sporadically or hereditary. Urinary metanephrin and normetanephrin levels, serum calcium, parathormone levels appeared to be normal. And genetic testing for detecting RET mutations proved the MTC was sporadically. The medical team consisting of endocrinologists, general surgeons, and obstetricians decided that surgery should be performed during the second trimester of pregnancy.
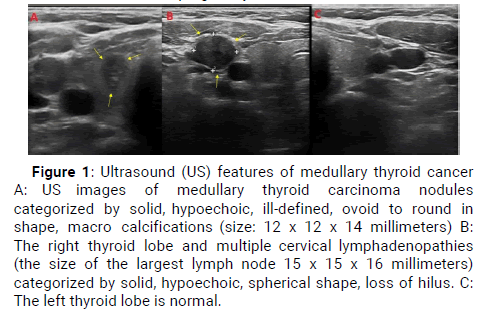
Figure 1: Ultrasound (US) features of medullary thyroid cancer A: US images of medullary thyroid carcinoma nodules categorized by solid, hypoechoic, ill-defined, ovoid to round in shape, macro calcifications (size: 12 x 12 x 14 millimeters) B: The right thyroid lobe and multiple cervical lymphadenopathies (the size of the largest lymph node 15 x 15 x 16 millimeters) categorized by solid, hypoechoic, spherical shape, loss of hilus. C: The left thyroid lobe is normal.
Total thyroidectomy and total cervical lymph node dissection were performed in her 19th week of pregnancy. Pathological examination showed a medullary carcinoma with a diameter of 8 x 4 x 5 millimeters in the right lobe of the thyroid gland. The mass was infiltrating the surrounding tissues had a lymph vascular and perinatal invasion. MTC metastasis was detected in 5 of the removed lymph nodes. On 50 high magnification fields, the tumor showed a characteristic appearance with the presence of round to polygonal tumor cells (Figure 2). Calcitonin immune histochemical stain revealed diffuse and strong positivity on 100 high magnification fields. The calcitonin level dropped to the level of 12 ng/L after surgery. There was not a suspicious appearance of malignancy in the postoperative ultrasound images. Levothyroxine treatment had initiated right after the surgery to prevent fetal complications. Calcium and active vitamin D3 supplementation were added. The patient gave birth to a term healthy infant.
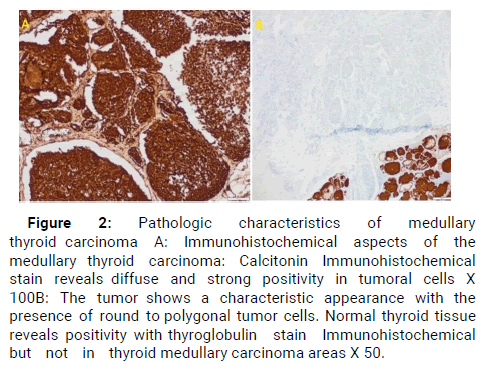
Figure 2: Pathologic characteristics of medullary thyroid carcinoma A: Immunohistochemical aspects of the medullary thyroid carcinoma: Calcitonin Immunohistochemical stain reveals diffuse and strong positivity in tumoral cells X 100B: The tumor shows a characteristic appearance with the presence of round to polygonal tumor cells. Normal thyroid tissue reveals positivity with thyroglobulin stain Immunohistochemical but not in thyroid medullary carcinoma areas X 50.
There are several cases of MTC as a component of MEN syndromes in the literature so far. To our knowledge, we report the first case of MTC that sporadically occurred in a pregnant woman. Once MTC is diagnosed during pregnancy, further examination for pheochromocytoma must be performed. RET oncogene analysis might be helpful. However, we would like to emphasize that MTC can also be seen in pregnant women without being a component of MEN syndromes.
Management of thyroid malignancy during pregnancy is essential for both maternal and fetal health. Since MTC has more extensive and aggressive features than DTC, the timing of the treatment can be challenging for both the patient and her medical team. Due to the rarity of MTC and pregnancy coexistence and lack of adequate data, there is not a consensus about the timing of the surgery [5]. For patients have diagnosed during the third trimester, surgical treatment can be safely postponed to the postpartum period, but for patients have diagnosed in the previous period, surgery is often considered without delay. For these patients, the safest period to perform surgery in the second trimester [6].
Lymph node metastasis is detected in %70 of patients on the course of MTC [5]. The surgery options for MTC include limited lymph node dissection or total lymph node dissection of the neck, both with total thyroidectomy. CEA and calcitonin levels are useful to identify residual tumor mass. Elevation of these markers is important for recurrence during the follow-up period. Our patient, who had multiple metastatic lymph nodes, underwent a total thyroidectomy and total neck lymph node resection. After surgery, calcitonin and CEA levels are dropped (Table 1).
| Preoperative | Postoperative | |
|---|---|---|
| Tsh (mıu/l) (0,27-4,20) | 2,33 | 0,26 |
| Free t4 (ng/dl) (0,93-1,71) | 0,95 | 1,05 |
| Free t3 (ng/dl) (2,01-4,42) | 3,39 | 2,69 |
| Cea (mcg/l) (0-6,50) | 4,3 | 1,05 |
| Calcitonin (ng/l) (0,20-5,0) | 792 | 12,4 |
| Calcium (mg/dl) (8,60-10) | 8,65 | 8,87 |
| Urinary metanephrine (ug/24 h) (0-341) | 18,27 | |
| Urinary normetanephrine (ug/24 h) (0-444) | 56,49 |
Table 1: Comparison of preoperative and postoperative blood tests.
Hyperparathyroidism is a typical result of total thyroidectomy. It’s essential to keep serum calcium and vitamin d levels at an optimal range in order to maintain fetal bone development and protect maternal bone reserves. Adequate vitamin D3 and calcium supplementation must be initiated after surgery.
The authors declare they have no potential conflict of interest regarding the investigation, authorship, and /or publication of this article
This study received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Citation: Mustafa Aydemir. "Medullary Thyroid Carcinoma during Pregnancy that Occurred Sporadically: A Very Rare Case". Oncol Cancer Case Rep, 2022, 8 (2), 1-2.
Received: 01-Sep-2022, Manuscript No. OCCRS-22-63016; Editor assigned: 05-Sep-2022, Pre QC No. OCCRS-22-63016(PQ); Reviewed: 13-Sep-2022, QC No. OCCRS-22-63016 (Q); Revised: 25-Sep-2022, Manuscript No. OCCRS-22-63016(R); Published: 30-Sep-2022, DOI: DOI: 10.4172/2471-8556.8.2.011
Copyright: © 2022 Aydemir M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.