Case Report - (2025) Volume 11, Issue 1
Introduction: AIDS-related Kaposi sarcoma decreased dramatically over the last two decades with the introduction of ART. It has improved the prognosis and outcome of PLHIV, however, delayed initiation lead to higher risk of AIDS defining illness such as Kaposi sarcoma. In the Philippines, the true prevalence of AIDS-related Kaposi sarcoma has not been established. This case is being reported for its rarity in the Philippines and to discuss diagnostic approach and treatment options available for disseminated AIDS-related Kaposi sarcoma in our locality.
Objectives: To discuss a rare case of disseminated AIDS-related Kaposi sarcoma in the advent of ART.
Case summary: A 31-year-old male diagnosed with HIV last 2016 who was not on ART presented at the ER with AIDS-defining signs and symptoms. He was admitted and opportunistic infections were treated accordingly, however there was persistent febrile episodes in which fever of malignancy was considered. The patient had multiple skin nodules and patches characterized as purple and localized over the trunk, bilateral upper and lower extremities. He also presented with multiple cervical and inguinal lymphadenopathies. He underwent skin lesion and excision cervical lymph node biopsy with histopathologic diagnosis consistent with Kaposi sarcoma. Further metastatic work-up were also done such as CT scan of the chest, whole abdomen and EGD-colonosopy with tissue biopsy. The patient was started on antiretroviral 2 weeks prior to discharge and was advised close follow-up at the OPD for chemotherapy planning. On follow-up admission, the lesions further disseminated on the inguinal area. The ideal chemotherapy for the patient is liposomal doxorubicin however it is costly and not available in the institution. Alternative chemotherapy, which is less myelotoxic is weekly paclitaxel. The patient was monitored for treatment response and possible side effects.
Conclusion: It is critical to establish whether Kaposi sarcoma is localized or systemic in order to determine the appropriate treatment. Additional documentation and response to treatment of PLHIV with Kaposi sarcoma is necessary to further optimize treatment and able anticipation of complications.
HIV-AIDS • Kaposi sarcoma • ART
Kaposi Sarcoma (KS) is a multicentric neoplastic proliferation of the vascular endothelial cells and usually associated with human herpes virus-8 in an immunocompromised patient. Acquired Immunodeficiency Syndrome (AIDS) related KS has mucosal and systemic involvement with rapid progression confined mostly to skin but may also disseminate, in rare cases, to extracutaneous sites such as gastrointestinal tract and lungs [1,2].
Early diagnosis and initiation of treatment greatly affects the outcome of these patients. With the advent of Anti Retroviral Therapy (ART), incidence of AIDS-related KS in developed countries had dramatically decreased [3].
However, in the Philippines, incidence of AIDS-related KS is not yet established and remains underreported. There were 6 reported cases of KS in a tertiary hospital in the Manila, Philippines with alarming increase in newly diagnosed cases of Human Immunodeficiency Virus (HIV) of 203% between 2010 and 2018 in the country. This exponential rise made it a major health priority and to address this problem, ARTs are given for free by the Philippine government and has put several HIV testing hubs across the country [4].
This case is being reported for its rarity in the Philippines and to highlight the importance of early initiation of ART.
A 31 year-old male presented at the emergency room with dyspnea on April 24, 2022. Patient presented with febrile episodes (T-max 40°C), multiple cervical-inguinal lymphadenopathies, hematemesis, hemoptysis, persistent back pain, poor oral intake, and progressive significant weight loss. The patient had been previously diagnosed with HIV last 2016. However patient was lost to follow-up hence, anti-retroviral therapy was not initiated.
Physical examination findings revealed pale palpebral conjunctiva, multiple cervical and inguinal lymphadenopathies. The skin has multiple nodules characterized as purple, tender, localized at the back, upper and lower extremities (Figures 1 and 2). There was also noted purple nodule on the hard palate and oral thrush was seen on the tongue. The patient is tachycardic with regular rhythm, distinct heart sounds and no murmur appreciated. There was symmetrical chest wall expansion with bibasal crackles noted. The abdomen is flat with normoactive bowel sounds, and non-tender.
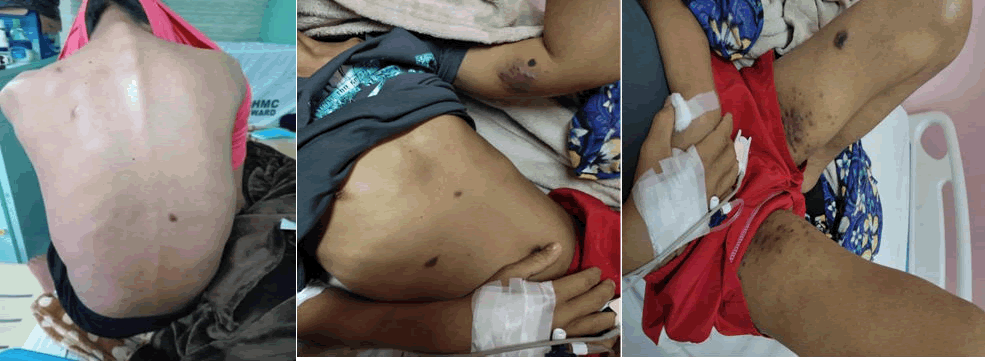
Figure 1. Violaceous nodular KS lesions on the back, upper and lower extremities.
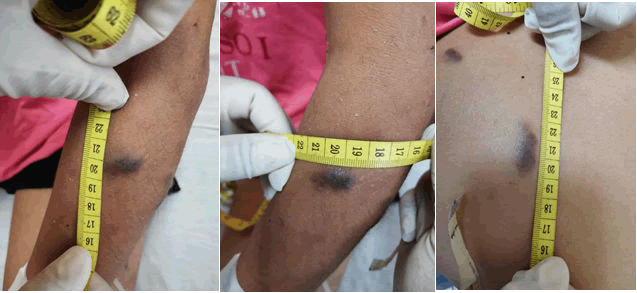
Figure 2. Skin lesions of Kaposi sarcoma taken from the patient.
Patient was initially managed as a case of Pulmonary Tuberculosis (PTB) and Pneumonia in the immunocompromised host. Work-up for other opportunistic infections were done. Regimen 1 for PTB and Pneumocystis Pneumonia (PCP) prophylaxis were started.
Over the course in the ward, the patient had persistent febrile episodes despite treatment of opportunistic infections with unremarkable repeat blood and sputum culture. Antiretroviral therapy was also started after 2 weeks of PTB Regimen 1. The CD4 count of the patient was 9 cells/mm3 predisposing him to different opportunistic infections and AIDS-defining illness.
The patient underwent skin lesion biopsy, in which the histopathlogic diagnosis was consistent of Kaposi Sarcoma (Figure 3). He also underwent cervical lymph node Level IV biopsy with same microscopic findings with that of the skin biopsy (Figure 4). The patient was referred to oncology service with initial plan to localize and establish extent of the Kaposi sarcoma then proceed with treatment planning.
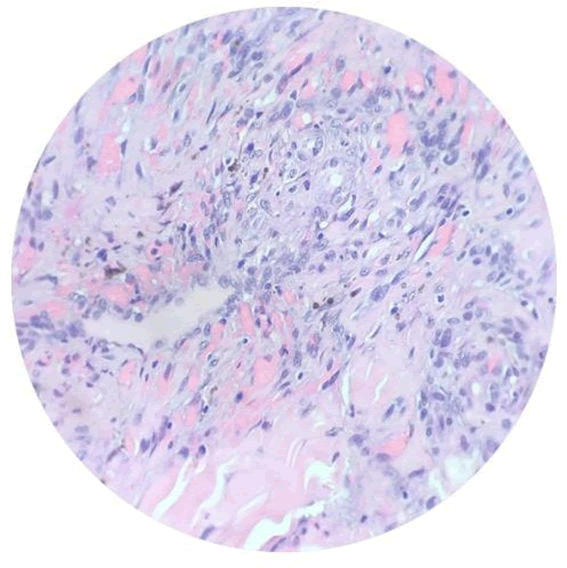
Figure 3. Microscopic features of skin lesion taken from the back of the patient: Proliferation of spindle cells in nodular aggregates, some dissecting with collagen bundles. There are areas with vascular proliferation with small-vessel protrusion into a vascular space.
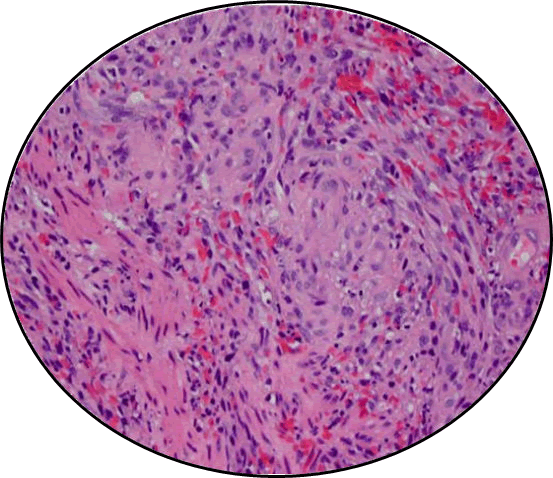
Figure 4. Microscopic features of cervical lymph node (Level IV left) taken from the patient: Proliferation of intersecting fascicles of uniform spindle cells dissected by collagen bundles and hemosiderin laden macrophages.
Additional metastatic work-ups were also done including CT scans (chest, whole abdominen and cranial) and colonoscopy-endoscopy with biopsy (Figures 5 and 6). Gastric ulcer sample during endoscopy was taken for biopsy which was consistent with chronic gastric ulcers (Figure 7).
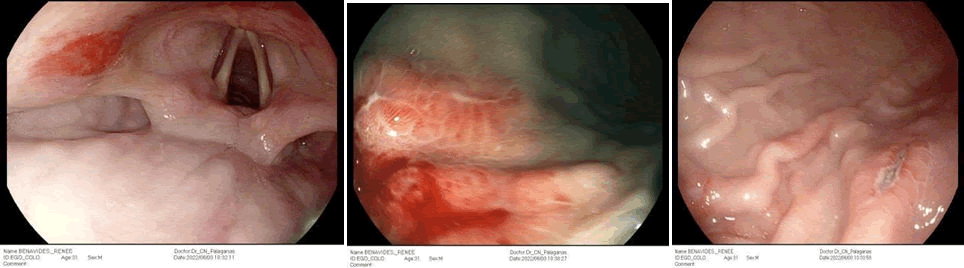
Figure 5. Endoscopic findings. An erythematous, raised, nodular ~1 cm, patchy area is noted in the left epiglottic fold. The esophageal mucosa is normal. Intact Z-line. Tight LES.
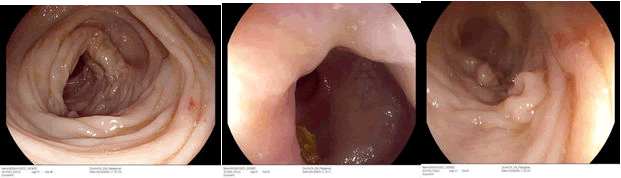
Figure 6. Colonoscopic findings. Normal fundus. Cardia tightly hugged the scope on retroflexed view, normal mucosa. Multiple ulcerations are noted in the greater curvature of the body of the stomach. The ulcers measure 5-12 mm in diameter, some round, some elongated, white based, with raised, nodular and erythematous borders; and without stigmata of recent bleeding. Multiple biopsies were taken from the base and borders of the ulcers for histopath examination. The antrum was mildly erythematous, there was no ulcer, mass or polyp. The pylorus was patent. D1 and D2 mucosa were unremarkable. The ampulla was identified, and observed to have adequate bile flow.
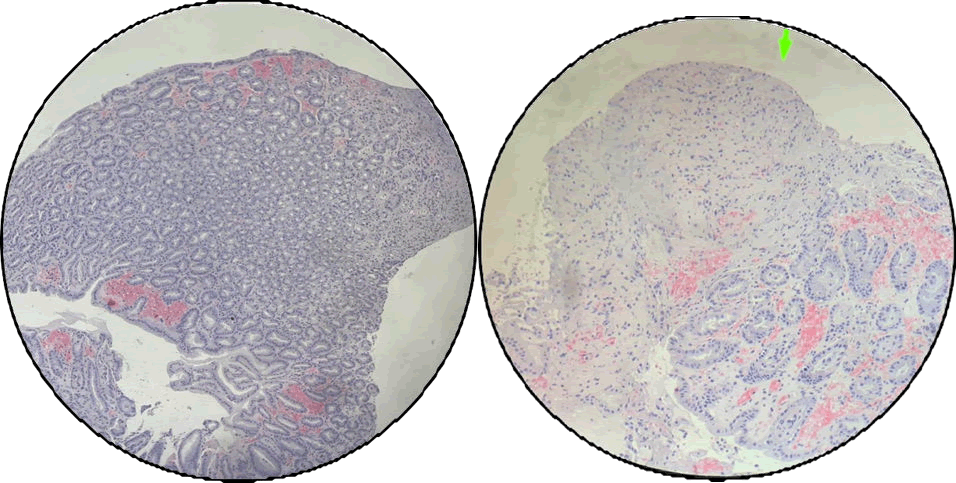
Figure 7. Gastric ulcer taken during endoscopy: Histopathologic diagnosis was consistent with chronic gastric ulcers.
Chest CT scan revealed pulmonary findings of patchy reticulonodular and ground glass opacities with areas of consolidation, interlobular septal thickening and nodularities which are suggestive of pulmonary involvement from the known Kaposi sarcoma. On the other hand, the whole abdominal CT scan revealed retroperitoneal, iliac and inguinal lymphadenopathy that could be a neoplastic process such as lymphoma. The neck CT scan revealed bilateral cervical and supraclavicular lymphadenopathies. The head CT scan has no definitive evidence of enhancing mass or leptomeningeal enhancement (Figure 8).
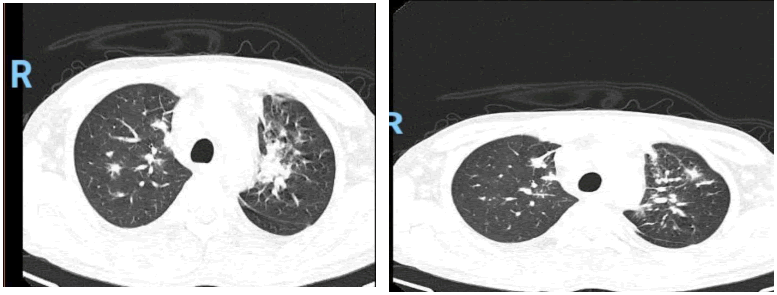
Figure 8. Pulmonary findings of patchy reticulonodular and ground glass opacities with areas of consolidation, interlobular septal thickening and nodularities are suggestive of pulmonary involvement from the known Kaposi sarcoma. However, other infectious/ inflammatory etiology may present with similar imaging findings. Please correlate with clinical and laboratory parameters. Small pulmonary air cyst, posterior segment of the right upper lobe. Subsegmental atelectasis, medial segment of the middle lobe and inferior lingula. Minimal bilateral pleural effusion with passive atelectasis, postero-basal segments of both lower lobes mild hepatomegaly.
The patient was discharged, clinically improved then to be re admitted for systemic treatment once with cardiopulmonary and IDS clearance. He was instructed to have close follow-up at the OPD before starting chemotherapy.
AIDS-related KS has a rapid progression and early diagnosis and initiation of treatment is crucial in the outcome of patients [5]. The diagnosis is usually suggested by the characteristic appearance of skin lesions, which can present as macules, papules, nodules or plaques, ranging in color from faint pink to purple to brown. These characteristic lesions may also be present on the oral and genital mucosa, with or without accompanying internal organ involvement. Associated dissemination to lymphatics may occur, with or without painful lymphoedema and/or lymphadenopathy. Visceral disease is present in a significant proportion of cases at presentation, but occurs at much higher rates in sub-Saharan Africa [6].
In our patient, skin lesion sample was taken at the back with final histopathologic diagnosis of spindle cell proliferation compatible with Kaposi sarcoma. Microscopic description show proliferation of spindle cells in nodular aggregates, some dissecting with collagen bundles (Figure 3).
Excision biopsy of the cervical lymph nodes, level IV left was done which revealed histopathologic diagnosis of atypical spindle cell proliferation suggestive of Kaposi sarcoma (Figure 4). The same specimen was sent for immunohistochemistry stain with result of positive CD31, strong, diffuse cytoplasmic membrane expression in the neoplastic cells.
Kaposi sarcoma is universally associated with HHV-8 infection (also known as Kaposi Sarcoma-associated Herpesvirus, KSHV). Serologic confirmation of HHV-8 infection is present in 95-98% of patients with Kaposi sarcoma howesver it was not done due to unavailability of HHV-8 stain in the Philippines [7]. Immunohistochemistry with CD31 and CD34 are also useful in certain circumstances whether tumor has a vascular origin. Additional biopsy of nodal or visceral sites is also suggested if coexisting malignancies are suspected like lymphoma and MCD. In our patient, we only had CD31 IHS.
Prior to introduction of ART, there is a high incidence of GI tract involvement and may occur even in the absence of cutaneous disease. It may manifest as wseight loss, abdominal pain, GI bleed, nausea or vomiting, obstruction, diarrhea, and malabsorption. They are typically diagnosed through endoscopy as it appears as isolated or confluent hemorrhagic nodules [8]. In our patient, the endoscopy-colonoscopy biopsy was negative for KS however, in contrast to the confirmation by biopsy, KS may not be depicted since lesions tend to be sub mucosal.
Among visceral involvement, lung involvement in KS is the most life-threatening occurring 20% of patients [9]. It manifests as dyspnea, cough, hemoptysis, fever, chest pain, and sometimes may be asymptomatic. The presumptive diagnosis can be done thru bronchoscopy which may have an appearance of cherry red, marginally elevated lesions. Lastly, lymph node involvement is no clinical significance and is not associated with worse outcome. Bronchoscopy should have been also done as part of the metastatic work-up.
The patient can be considered to have systemic involvement with the presentations and work-up done. Careful treatment planning and follow-up is indicated for improve clinical outcome and survival. Introduction of effective combination antiretroviral therapy has a major influence on the epidemiology and natural history of AIDS-KS [10].
Ideally, the chemotherapy should be liposomal doxorubicin, however it is very expensive, hence alternative chemotherapy were considered which include vincristine+bleomycin+/-doxorubicin; paclitaxel; etoposide; and gemcitabine which will be started as outpatient once with cardiopulmonary and IDS clearance.
In conclusion, it is critical to establish whether Kaposi sarcoma is localized or systemic in order to determine the appropriate treatment. Further studies on the incidence of AIDS-related KS in the Philippines is recommended to determine the disease burden in the country and to determine the associated factors in the delayed initiation of treatment despite free ART given by the government. If the extent of AIDS-related KS is established in our country, the availability of treatment options should also be allocated or made accessible. Additional documentation and response to treatment of PLHIV with Kaposi sarcoma is necessary to further optimize treatment and able anticipation of complications.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Dumalnos KCM, et al. "Disseminated AIDS-Related Kaposi Sarcoma in the Advent of Antiretroviral Therapy in a Tertiary Hospital in the Philippines: A Case Report". Oncol Cancer Case Rep, 2025, 11(1), 1-4.
Received: 29-Sep-2023, Manuscript No. OCCRS-23-115358; Editor assigned: 03-Oct-2023, Pre QC No. OCCRS-23-115358 (PQ); Reviewed: 17-Oct-2023, QC No. OCCRS-23-115358; Revised: 03-Jan-2025, Manuscript No. OCCRS-23-115358 (R); Published: 10-Jan-2025, DOI: 10.35248/2471-8556.25.11(1).001
Copyright: © 2025 Dumalnos KCM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.