Case Report - (2025) Volume 11, Issue 2
Choriocarcinoma is a type of gestational trophoblastic tumor; approximately 20% of patients will require treatment for malignant sequelae after evacuation of a hydatidiform mole. Therefore, rigorous monitoring with quantitative levels of human Chorionic Gonadotropin (hCG) is essential. This type of tumor occurs in about 1 in every 20,000 to 40,000 pregnancies, with a risk of 2-3% after a complete mole. Clinical case: A clinical case of a patient with metastatic choriocarcinoma to the brain, lung and kidney is described, the latter being of low prevalence. The patient did not receive medical follow-up after a complete hydatidiform mole and was diagnosed due to neurological symptoms. So far, she has experienced favorable progress under monitoring of hCG levels. Conclusion, the optimal management of this disease depends on the type of specialized center, the review of the pathology and a treatment based on evidence and clinical guidelines. Given the rarity of trophoblastic tumors, as well as the associated diagnostic challenges, follow-up of hydatidiform molars is crucial to prevent metastasis, as in the case of this patient.
Gestational trophoblastic tumor • Choriocarcinoma • Brain metastasis • Human chorionic gonadotropin hormone
Choriocarcinoma is a type of gestational trophoblastic tumor. Approximately 20% of patients will be treated for malignant sequelae after evacuation of a hydatidiform mole, so follow-up with quantitative hCG levels is strictly necessary. This type of tumor occurs in about 1 in every 20,000 to 40,000 pregnancies. The risk of developing choriocarcinoma after a complete mole is 2-3% (0.1-0.5% in incomplete mole), being the most common gestational trophoblastic tumor, with a wide range in the age of presentation of the patients, with an average of 30 years [1]. It can arise from any type of gestational event: 50% after a full-term pregnancy, 25% after a molar pregnancy, and 25% after other types of pregnancy [2].
Uterine bleeding is the most frequent symptom, but extrauterine events can be the first presentation in a patient with extrauterine dissemination, as in the case of the patient reported, with metastasis to the lung, central nervous system and kidney, the latter reported with less frequency. The optimal management of the disease depends on the type of specialized center, the review of the pathology and the treatment based on evidence and management guidelines. Which contributes to the prognosis. Trophoblastic tumors are rare and pose significant diagnostic challenges due to wide differential diagnoses and diagnostic uncertainty of their precursor lesions [3].
A 38-year-old female patient was admitted to the emergency room with an altered state of consciousness, seizure from focal motor to bilateral tonic-clonic onset lasting 3 minutes with recovery of consciousness and a new similar episode during the assessment. Postictal period was 15 minutes. Treatment was started with levetiracetam (500 mg every 12 hours) with an adequate response. During the evaluation, the patient presented vaginal bleeding, with a report of positive qualitative beta subunit chorionic gonadotropin. Family members report that she has had metrorrhagia for a month. The last pregnancy was 10 months ago, with evidence of a molar pregnancy, carried out for curettage, with pathology that evidenced gestational trophoblastic disease type complete hydatidiform mole. The patient loses follow-up and does not perform controls. In the 2 weeks prior to admission, she presented intense headache, changes in behavior, due to aggressive and irritable behavior, and seizures.
During the current evaluation, in the ultrasonography, an enlarged uterus was found, the presence of multiple endometrial cystic foci configuring a mass with a snowstorm pattern, measuring 108 × 66 × 70 mm, volume of 264 cc, findings suggestive of molar pregnancy (Figure 1). On physical examination she was febrile, drowsy, requiring invasive mechanical ventilation and vasopressor support. Respiratory sounds with bilateral rhonchi, abundant mobilization of secretions. Chorionic gonadotropin report 219181 mIU/ml in blood (Table 1). She was taken for obstetric curettage which showed an enlarged uterus (11 cm), a curettage product with scant ovular remains, and difficult bleeding control.
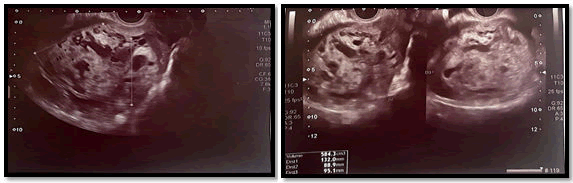
Figure 1. Ultrasonography with multiple endometrial cystic foci configuring a mass with a snowstorm pattern, measuring 108 × 66 × 70 mm, volume of 264 cc, findings suggestive of molar pregnancy.
| Gravindex | Positive | Unit |
| Calcium | 8.06 | mg/dl |
| Chlorine | 105 | mEq/L |
| Potassium | 3.12 | mEq/L |
| Sodium | 137 | mEq/L |
| Bun | 6.8 | mg/dl |
| Creatinine | 0.6 | mg/dl |
| H.B. | 11.7 | |
| HTO | 31.1 | |
| Neutrophils | 5420 | uL |
| Lymphocytes | 4.1 | % |
| Neutrophils | 80.4 | % |
| BHCG | 219181 | mUl/ml |
| Total bilirubin | 0.59 | mg/dl |
| Direct bilirubin | 0.42 | mg/dl |
| Indirect bilirubin | 0.17 | mg/dl |
| TGO-AST | 27 | U/L |
| TGP-ALT | Fifteen | U/L |
| PTT | 30.4 | sec |
| PTT | 10.8 | sec |
| INR | 1.07 | |
| Lactate | 0.68 | mmol/L |
Table 1. Paraclinical.
Magnetic resonance imaging of the brain was performed (Figure 2)with evidence of an intra-axial lesion in the deep white matter of the left frontal lobe measuring 5 mm, oval, with peripheral contrast enhancement, which is associated with extensive vasogenic edema (thickness up to 12 mm). and in ferromagnetic sequences, bleeding within the lesion is evident. Without ruling out neuroinfection, paraclinical tests are performed, with a complete blood count showing anemia and mild hypokalemia, as well as metabolic acidosis partially compensated with mild oxygenation disorder. Lumbar puncture without signs of an infectious process, however, with a report of elevated hCG in CSF (Table 2). Chest tomography (Figure 3) with evidence of bilateral pleural effusion predominantly on the right. Numerous nodules with soft tissue density are identified in the right hemithorax. The largest of them projected in the posterior segment of the basal lobe with a long axis diameter of 68 mm. In the left hemithorax, nodules with the same characteristics were identified, the largest of which was projected in the anterior segment of the apical lobe with a long axis diameter of 12 mm.
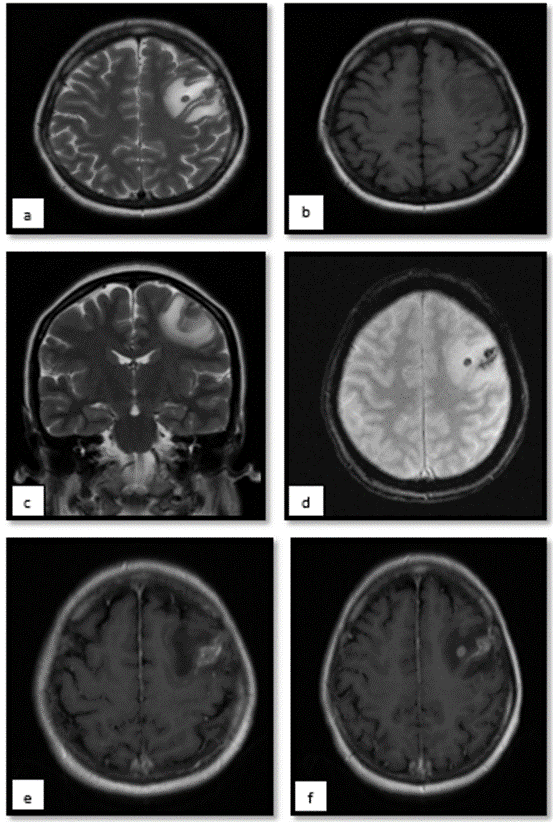
Figure 2. Magnetic resonance imaging of the brain showing intra axial lesion in the deep white matter of the left frontal lobe that measures 5 mm, oval, isointense on T1 (B), hypointense on T2 (AC), which is associated with extensive vasogenic edema (thickness up to 12 mm). and in ferromagnetic sequences, bleeding within the lesion is evident, characteristic of these. With peripheral contrast enhancement (F).
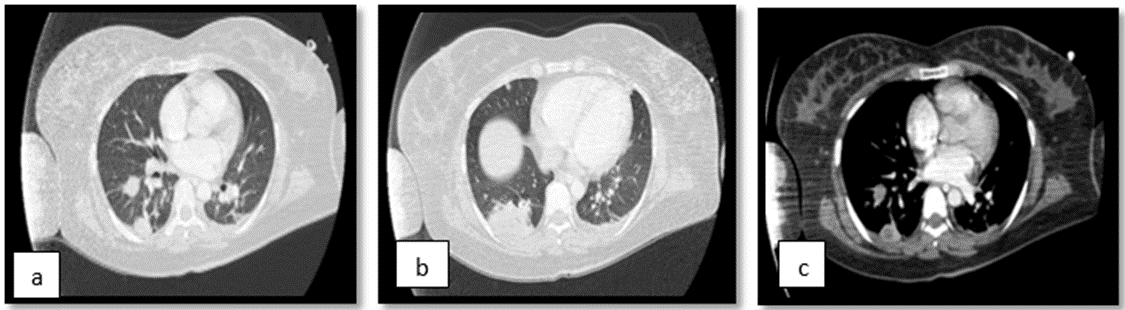
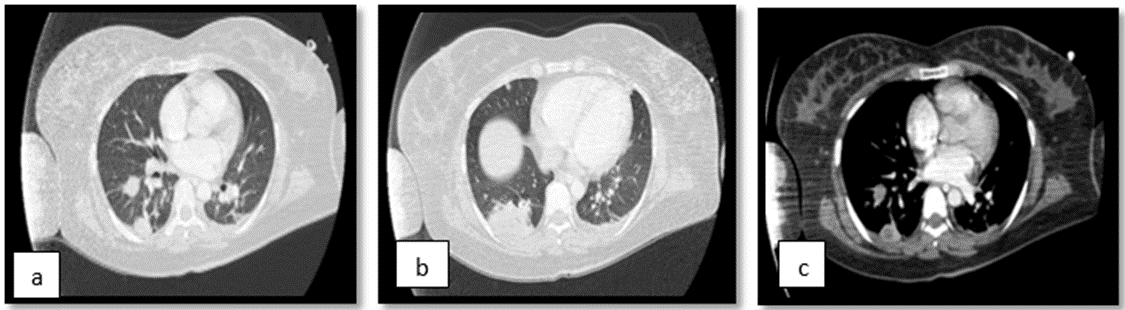
Figure 3. Chest tomography: Numerous nodules with soft tissue density are identified in the right hemithorax. The largest of them projected in the posterior segment of the basal lobe with a long axis diameter of 68 mm. In the left hemithorax, nodules with the same characteristics were identified, the largest of which was projected in the anterior segment of the apical lobe with a long axis diameter of 12 mm.
| Gravindex | Positive | Unit |
| Glucose | 67 | |
| Total proteins | 14 | |
| VDRL serology | NR | mg/dl |
| White | 0 | |
| Red | 2 | |
| Neutrophils | 0 | |
| Lymphocytes | 0 | % |
| Fresh erythrocytes | 100 | % |
| Created erythrocytes | Either | |
| Crop | Negative | |
| Chinese ink | Negative | |
| hCG | 747 | |
| Gram | Negative | mUl/ml |
Table 2. CSF.
Given these findings, an extension of the search for lesions was carried out, finding in neck tomography, numerous lymph nodes in the different spaces of the neck, the largest of which was projected in left station III with a diameter of 12 mm in the short axis. And in the bone system with the presence of a small lytic image projected on the vertebral body of C5. In tomography of the abdomen and pelvis (Figure 4), in the middle third of the left kidney the ill-defined hypodense image of 34 × 33 mm with soft tissue density, central uterus with thick endometrium of 31 mm of heterogeneous content. With the rest of the tumor markers reported (Table 3).
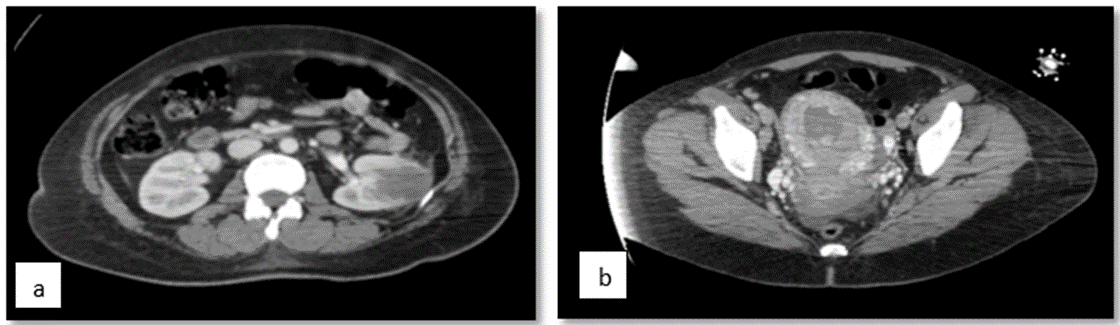
Figure 4. Abdominopelvic tomography which shows in the middle third of the left kidney the ill-defined hypodense image of 34 × 33 mm with soft tissue density, central uterus with thick endometrium of 31 mm of heterogeneous content.
Gravindex |
Positive |
Unit |
Antigen 19-9 |
10.22 |
U/mL |
LDH |
434 |
U/L |
AC 125 |
21.3 |
U/ml |
Carcinoembryonic GA |
3.54 |
ng/ml |
Serum alpha-fetoprotein |
2.66 |
ng/ml |
Alpha-fetoprotein in CSF |
<0.5 |
Ul/mL |
BHCG in CSF |
747.9 |
mUl/ml |
Table 3. Tumor markers.
Progressive weaning of vasopressor support and ventilation was initiated due to clinical and hemodynamic stability. If metastatic lesions are suspected, a biopsy of the lung lesion is performed. The pathology reports, labeled lower left segmental lobectomy: Violet brown lobectomy product measuring 3.5 × 1 × 1 cm, a violet-colored nodular lesion measuring 0.6 × 0.6 × 0.6 cm is observed, in apparent contact with the pleura. To which evidence of involvement by choriocarcinoma, immunohistochemistry studies show reactivity in the problem population with HCG, CKAE1/AE3, P63, PLAP, MUC4, INHIBINA AND SALL4. P53: 50%. KI67: 70%. The pathology of the obstetric curettage material shows atypical cells that suggest gestational tumor, with reactivity in the problem population with GATA-3, PLAP, CKAE1/AE3 OR HCG. there is patchy reactivity with SALL4, INHIBIN AND MUC4. No reactivity with P63. P53: NEGATIVE. KI67: 30%. With report of choriocarcinoma. The patient's ventilatory and hemodynamic stability is successfully achieved. With symptomatic improvement.
Finally, given the diagnosis of FIGO IV gestational trophoblastic neoplasia of the choriocarcinoma type, treatment with chemotherapy was decided to manage the high-risk trophoblastic neoplasia that the patient presented (cyclophosphamide, etoposide, methotrexate, vincristine, dactinomycin in combination with folic acid, dexamethasone, pegfilgrastim for complete the diagram). During the course, in the second cycle of chemotherapy, secondary intracranial hemorrhage was documented, in a lesion already described in the brain MRI, clinically with evidence of right hemiplegia and focal motor crises in the right upper limb, so the dose was increased. of levetiracetam with seizure resolution. As well as the requirement for supplemental oxygen at low flow to maintain perfusion oxygenation goals. Upon follow-up with hCG, the values described in Figure 5 of the patient with adequate evolution are documented.
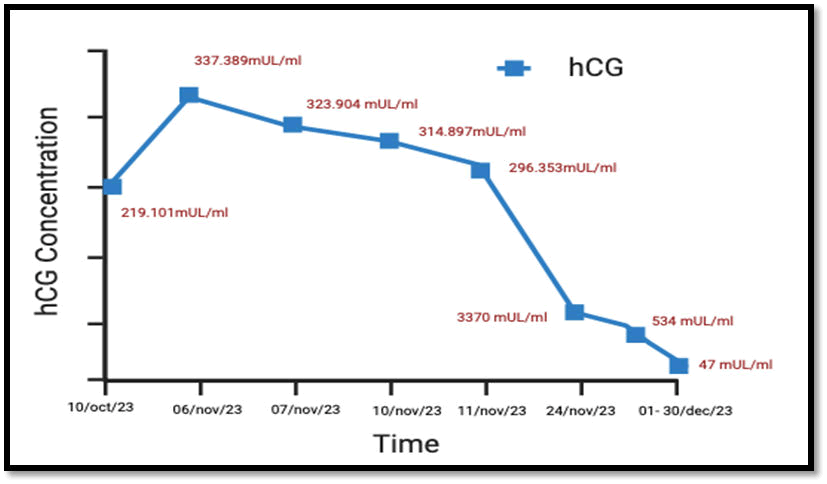
Figure 5. hCG levels over time.
Gestational trophoblastic diseases are proliferative disorders of the placental trophoblast. These can be non-neoplastic proliferation such as partial and complete hydatidiform moles, being premalignant conditions or true neoplastic such as gestational trophoblastic tumors. The latter include four different pathologies which are: Gestational choriocarcinoma, placental site trophoblastic tumor, epithelioid trophoblastic tumor and recently added placental site nodule. Known as gestational trophoblastic neoplasia. And each of them arise from several subtypes of placental trophoblast with a different pathobiology.
It has been described that the tumor can arise from any type of gestational event, 50% after the end of pregnancy, 25% after a molar pregnancy as in the case of our patient and 25% after other types of pregnancy [4]. Approximately 20% of patients will be treated for malignant sequelae after evacuation of a hydatidiform mole, the latter being observed in approximately 1 in 600 therapeutic abortions and 1 in 1000-1200 pregnancies [5].
Carcinoma occurs in approximately 1 in every 20,000 to 40,000 pregnancies, the risk of developing choriocarcinoma following a complete mole is 2-3% and there is a low but existing risk of developing choriocarcinoma following an incomplete mole (0.1-0.5%). The diagnosis of postmolar choriocarcinoma will be made an average of 13 months after mole evacuation according to existing data in the literature. While placental trophoblastic site tumor and epithelioid trophoblastic tumor have varied production of the hormone Human Chorionic Gonadotropin (HCG), choriocarcinoma is invariably present in all patients. Which makes it an excellent biomarker of disease progression. In which a stable or increasing HCG level allows early detection of progression of complete or partial hydatidiform mole to gestational trophoblastic neoplasia. This will allow for positive detection, treatment and follow-up if managed appropriately [6].
Serial quantitative determinations of serum hCG should be performed after molar evacuation, obtaining a first sample 48 hours after evacuation, every 1 to 2 weeks while elevated, and then at intervals of 1 to 2 months for 6 to 12 months. additional. During which monitored hCG contraception is recommended to reduce recurrent pregnancy during postmolar surveillance. Unlike our patient, who does not perform controls and loses follow-up, which is related to the neoplastic proliferation of gestational trophoblastic tumors like this case in question.
Gestational choriocarcinomas generally present as uterine masses, hemorrhagic and with necrosis. In histopathology, proliferating tumor cells of the chorionic villous trophoblast type of cytotrophoblasts bordered by layers of multinuclear syncytiotrophoblastic cells can be observed. Immunohistochemistry showed strong and diffuse positivity for hCG and HSD3B1. Intermediate trophoblasts express Mel-CAM, HLA-G and MUC-4 as in the case of our patient. And generally with a high Ki-67 proliferation index of over 90% [7].
Choriocarcinoma usually spreads widely hematogenously and associated with distant metastasis. It has been reported to commonly metastasize to the lungs and vagina and, less commonly, to the liver, brain, kidneys, and gastrointestinal tract. The symptoms of metastatic lesions are usually secondary to acute hemorrhages in the organ to which it spreads [8].
There are few documented cases of brain metastases due to choriocarcinoma, however, 10-20% of cases have been described. They are highly vascularized tumors and have a propensity to bleed as well as their metastases. The blood products present may be evident on MRI as loss of signal and “blooming” or flowering on T2* and intrinsically hyperintense signal on T1 [9]. They metastasize hematogenously with the possibility of presentation with aneurysmal lesions and other subdural or intraparenchymal hematomas [10].
The differential diagnoses of choriocarcinoma must be separated from its nongestational counterpart of somatic or germ cell origin, which occur in children and young adults. Which are choriocarcinomas in nulligravids. This type of tumor has a mixed component of germ cells in the ovary, extra gonadal sites which can be differentiated in histological findings. As well as differentiating them from other gestational trophoblastic tumors [11].
The diagnosis is based on the International Federation of Gynecology and Obstetrics (FIGO) 2000 criteria given by four or more stable human chorionic gonadotropin concentrations for three weeks, increasing human chorionic gonadotropin concentrations for three consecutive weekly measurements for at least one period of 2 weeks or more elevated but decreasing concentrations of human chorionic gonadotropin for six or more months after molar evacuationeitherIf there is a histological diagnosis of choriocarcinoma.
Biopsy is a method of confirmation of gestational trophoblastic neoplasia but it could cause complications depending on the location of the biopsy, causing massive uncontrollable bleeding such as in the lungs, in abdominal-pelvic organs, or brain biopsies as in our patient. Staging is essential. The American guidelines recommend initial stratification with Magnetic Resonance Imaging (MRI) of the brain and abdomen-pelvis and Computed Tomography (CT) of the chest, the FIGO recommends performing a pelvic-transvaginal Doppler ultrasound and a chest X-ray. In those patients with metastases larger than 1 cm or doubts about normality in the chest X-ray, it should be complemented with chest CT and brain MRI [12].
The use of Positron Emission Tomography (PET) is not yet well established; there are no differences with respect to conventional images, although it could be useful in metastases with unusual locations or the differentiation of metastatic nodules from necrotic or hemorrhagic tissue, even after the use of chemotherapy.
To define the treatment of gestational trophoblastic neoplasia, it must be determined with the FIGO (International Federation of Gynecology and Obstetrics) score; in the case of our patient, it was defined as stage IV and high risk. So it is treated with combined chemotherapy. Having high cure rates and acceptable toxicity profiles with Etoposide, Methotrexate, Dactinomycin, Cyclofosamide, Vincristine (EMA-CO) and the second regimen with Etoposide, Methotrexate, Dactinomycin, Etoposide, Cisplatin (EMA-EP), and for management of myelosuppression can be managed with granulocyte colony-stimulating factor. Taking into account the weekly monitoring of hCG until normalization of serum hCG as in the case of our patient [13].
Recognition of gestational trophoblastic tumors remains problematic, due in large part to the relative rarity and overlap with common gynecologic tumors. However, early and accurate diagnosis is crucial to define the treatment of patients due to the good response to chemotherapy, especially gestational choriocarcinoma; as well as monitoring both complete and partial moles with serum hCG, which is the main marker used in surveillance. Choriocarcinoma usually spreads hematogenously. Our patient had metastases to the brain, lung and kidney. Which is considered ultra-high risk according to FIGO. They can be complicated as a result of acute hemorrhages or complications such as the intracranial hemorrhage of the patient presented in this case, therefore it is important to adequately control molar pregnancies to minimize acute complications and identify malignant sequelae promptly.
Through this we can assert that none of those present have any conflicts of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Yovana-MartÃnez A, et al. "Description of a Rare Case of a Gestational Trophoblastic Tumor of the Choriocarcinoma Type Metastatic to the Brain, Lung and Kidney". Oncol Cancer Case Rep, 2025, 11(1), 1-6.
Received: 11-Jan-2024, Manuscript No. OCCRS-24-124989; Editor assigned: 13-Jan-2024, Pre QC No. OCCRS-24-124989 (PQ); Reviewed: 27-Jan-2024, QC No. OCCRS-24-124989; Revised: 19-Mar-2025, Manuscript No. OCCRS-24-124989 (R); Published: 26-Mar-2025, DOI: 10.35248/2471-8556.25.11(1).001-006
Copyright: © 2025 Yovana-Martinez A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.