Case Report - (2025) Volume 10, Issue 1
Dermatofibroma is a cutaneous condition that is typically localized in the dermis of the skin. It is a commonly occurring condition and is also known as benign fibrous histiocytomas of the skin, superficial/ cutaneous benign fibrous histiocytomas and common fibrous histiocytomas.
It occurs more often in middle-aged people and is slightly more common in women. The majority of lesions appear as small, elevated, hyperkeratotic, cutaneous nodules with a reddish-brown surface on the limbs.
Dermatofibromas • Clinicopathological • Exophytic tumour • Granular cell
Diagnosing dermatofibromas can be challenging due to their diverse range of clinicopathological variations. Here, we present a case of keloidal dermatofibroma. It is important not to disregard the keloidal form of dermatofibroma as a typical keloid. Trauma being a potential cause of dermatofibroma may be supported by the results of keloidal transformation in dermatofibromas [1-3].
Dermatofibroma is a common benign cutaneous nodule composed of fibroblasts and histiocytes, typically presenting as a firm, hyperpigmented papule on the lower extremities. While its classic appearance is well-documented, unusual morphological variants can present diagnostic challenges. One such rare variant is the keloidal presentation of dermatofibroma, where the lesion mimics a keloid both clinically and histologically. This atypical manifestation can lead to misdiagnosis and inappropriate treatment if not properly recognized. Understanding the clinical, dermoscopic, and histopathological features of keloidal dermatofibroma is crucial for accurate differentiation from true keloids and other fibrous skin tumors, ensuring appropriate management and prognosis.
A 26-year-old male patient presented to the OPD of Department of Dermatology. Patient complaint of multiple, asymptomatic exophytic lesions located at the lateral aspect of left upper arm and back since last 2 years. The lesions are progressive in nature and insidious in onset. There were no associated symptoms and no regional lymphadenopathy was present. There was no history of trauma to the affected area. Patient has no history of diabetes, hypertension or any other known condition and is not on any medication. Furthermore, the family history of the patient is nonsignificant [1-3].
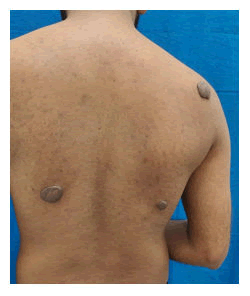
Figure 1. Multiple neurofibromas on the back in a patient with neurofibromatosis.
On further examination, three, well defined exophytic tumour like lesions of size varying from 3 cm to 6 cm in diameter with shiny, hyperpigmented, smooth surface was present over the back. They are rubbery on palpation, without apparent adhesion to deeper layers. A solitary, well defined, skin coloured growth of similar morphology, of size 2 cm in diameter presented over the left upper arm. Upon palpation, it was firm and non-tender. Dimpling sign could be elicited over these lesions.
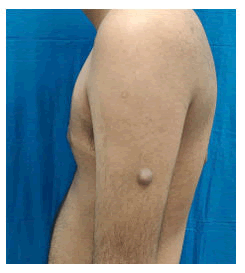
Figure 2. Solitary neurofibroma over arm in patient with neurofibromatosis type 1.
Dermoscopic findings revealed central reddish brown patch with peripheral dark brown network. Few lesions exhibited linear or arborizing telangiectasia. After examining the patient, a differential diagnosis of keloid, dermatofibroma, dermatofibrosarcoma protuberance was considered and the biopsy was taken from the sites of lesions to confirm the diagnosis.
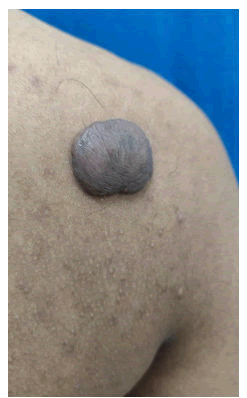
Figure 3. Close-up of pedunculated neurofibroma on shoulder in neurofibromatosis.
The histological findings revealed poorly defined proliferation of fibro-histiocytic cells within the dermis with overlying sparing of grenz zone. At the periphery of lesion, entrapment of collagen fibre was noted. The overlying epidermis is acanthotic and showed increased basal layer pigmentation. This thus confirmed the diagnosis of dermatofibroma.

Figure 4. Multiple cutaneous neurofibromas on back suggestive of neurofibromatosis type 1.
Dermatofibroma accounts for approximately 3% of skin biopsy samples which are received by dermato-pathology laboratories [2].
Dermatofibromas typically present clinically as hard, reddishbrown nodules, whereas keloidal dermatofibromas typically manifest as hard, erythematous papules [4].
The formation of dermatofibromas is explained by two theories: (A) Neoplastic proliferation and (B) Reactive process vs. clonal. There is proof to support each of these hypotheses. Patients with dermatofibromas frequently have a history of potentially initiating local trauma at the location, such as a thorn or wood splinter bite or superficial puncture wound [1].
The histopathological types of dermatofibroma include fibrous histiocytoma (most common type), aneurysmal, epithelioid, cellular, atrophic, clear cell variants and other atypical variants (including palisading, keloidal, granular cell, myxoid, lichenoid, balloon cell and signet-ring cell variants) [2].
Upon histopathological analysis, typical forms of dermatofibromas are commonly observed to manifest as welldefined, nodule tumours with a random arrangement of small spindle cells. Regular proliferation of the epidermis overlaying the tumour and darkening of the basal cell layer are characteristic features of dermatofibromas. Whereas, in the superficial part of the tumour in keloidal dermatofibromas, bounded, keloid-like patches made of thick, highly eosinophilic collagen fibres which are placed erratically can be seen. Additionally, round keloidal collagenous fibres can be seen. Furthermore, keloidal dermatofibromas lack elastic fibres which is a similar morphology as of keloidal scars [5,6].
To the best of our knowledge, only a small number of cases of keloidal dermatofibroma have been documented since its initial description in 1998. The existence of keloidal dermatofibroma has been proposed to support the injury theory of dermatofibroma genesis, since keloids are caused by skin injuries. The hypothesis that trauma may be a potential cause of dermatofibroma may be supported by the finding of keloidal transformation to dermatofibromas. Researchers have discovered this novel variation to be imporant because Asians are at greater risk to develop keloids.
The authors have declared that no conflict of interests.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Received: 10-Aug-2024, Manuscript No. MRCS-24-145085; Editor assigned: 13-Aug-2024, Pre QC No. MRCS-24-145085 (PQ); Reviewed: 27-Aug-2024, QC No. MRCS-24-145085; Revised: 01-Jan-2025, Manuscript No. MRCS-24-145085 (R); Published: 19-Jan-2025, DOI: 10.4172/2572-5130.25.10(01).1000277
Copyright: © 2025 Dogra P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.