Case Report - (2023) Volume 9, Issue 2
Lymph node positivity is one of the most important prognostic indicators and a wide lymphadenectomy should be routinely performed. In one study done in 101 patients with duodenal adenocarcinoma, the three and five years survival rates of patients with negative nodes were 73% and 68%, respectively, compared with 35% and 22% in patients with nodal metastases.
Although data are limited guiding adjuvant therapy options, oxaliplatin based chemotherapy is typically offered to high risk patients, such as those with positive lymph nodes. In some series, adjuvant radiation is associated with improved local control but no difference in overall survival.
The rarity of the incidence of duodenal carcinomas make it is a challenging entity to manage. Extreme rarity of the adenocarcinoma at ligament of trietz also made the true incidence of adenocarcinoma is unknown. Nevertheless, duodenal adenocarcinomas constitute about 0.3% to 0.4% of all GIT cancers.
Lymph node • Oxaliplatin • High risk • Carcinomas • Adenocarcinoma
Primary small bowel neoplasms at the ligament of treitz are extremely rare and require advanced surgical technique for extirpation. Management of such a rare tumour is a unique challenge for the surgeons due to several reasons [1]. Those include the diagnostic difficulty with insidious onset and delayed presentation leading to increased growth of the neoplasm by the time of diagnosis, the partial retroperitoneal location of the tumour with nearness to critical anatomical structures like pancreas and superior mesenteric pedicle, difficulty in surgical planning with small bowel resection and reestablishment of gastrointestinal continuity. Present an unusual case of a primary small bowel adenocarcinoma at the ligament of treitz, requiring segmental resection from third part of the duodenum to proximal jejunum [2].
61 years old farmer presented with a history of melena for 6 months and anemic symptoms. He was diagnosed with rectal adenocarcinoma 5 years ago and underwent A PR in 2016. He was referred to us by oncologists for follow-up colonoscopy and Upper Gastrointestinal Endoscopy (UGIE) for the investigation of melena [3].
We found a large malignant looking polypoidal mass in the third part of the duodenum during the UGIE and multiple biopsies were taken. Colonoscopy was normal and no polyps were found in entire colon [4].
Histology 2022, from the biopsy was moderately differentiated adenocarcinoma. Contrast enhanced CT scan showed a heterogeneously enhancing soft tissue density mass lesion measuring 4.4 cm × 7.2 cm in size in the third part of the duodenum favoring a malignant lesion with evidence of perilesional fat infiltration. However, there was no CT evidence of pancreatic or other bowel loop infiltration. The transverse colon and mesocolon appears normal. The lesion is displacing the superior mesenteric vessels anteriorly without any vascular infiltration. Posteriorly the aorta appears normal. There are multiple enlarged lymph nodes in the perilesional and superior mesenteric group. No liver or lung secondaries [5].
Patient was evaluated for co-morbidities and optimized as required. His weight was 35 kg with a BMI of 14.8 kg/m2. Nutrition referral was made considering his very low BMI and supplementations were started. On admission Hemoglobin was 7.8 q/dl and 3 units of RCC transfused preoperatively [6, 7].
Surgical procedure was carried out under general anesthesia with invasive monitoring and epidural analgesia. Upper abdominal midline incision was made. Hepatic flexure was mobilized and full duodenal kocherization made. Tumor was identified at the ligament of treitz involving third part of the duodenum up to proximal jejunum. The neoplasm was circumferential and an almost obstructing mass macroscopically. It was a large tumor (60 mm × 65 mm × 20mm) infiltrating Third and fourth parts of the duodenum and proximal jejunum. It is very closely related to the aorta posteriorly and separated from it with only very flimsy layer of loose areolar issue. The superior mesenteric artery was pushed anteriorly by the tumour mass. The surrounding peritumoral desmoplastic reactions/adhesions were carefully dissected, allowing the tumour to be gently released. Superior mesenteric vascular pedicle carefully separated from the tumour and lifted off from the posteriorly placed aorta. At this point it was evident that it is possible to achieve an adequate proximal resection margin without committing for Whipples’ surgery. Duodenum divided at the junction of 2nd and third part of the duodenum with a 3 cm macroscopic proximal margin and assured that enough length is available from sphincter of oddi for anastomosis. Proximal jejunum divided with a linear stapling device with an adequate distal resection margin and the stapler margin is oversewed. The small bowel tumour was resected (from third part of the duodenum up to proximal jejunum) en bloc with the corresponding jejunal mesentery for wide margins and nodal clearance. A hand sewn end to side anastomosis made in two layers with 3.0 PDS sutures [8]. The distal cut end of the duodenum anastomosed to the anti-mesenteric border of as the free limb of proximal jejunum (Duodenojejunostomy). Distal enterotomy made in the jejunum and drain is inserted through it and brought in to the second part of the duodenum and taken out through the anterior abdominal wall in duodenal exteriorisation. A separate feeding jejunostomy created distal to the duodenal exteriorisation. The operative time was 6 hours and intraoperative blood loss is 350 ml (Figure 1).
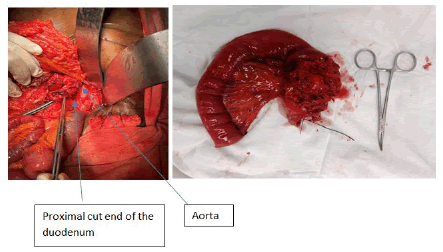
Figure 1: Post-operative period was uneventful.
The histopathology report stated that sectioning through the duodenum and jejunum shows a moderately differentiated adenocarcinoma with focal mucinous differentiation. The tumour infiltrating full thickness of the bowel wall, but the circumferential margin is clear. (0.5 mm) Vascular emboli were not seen and there were ten lymph nodes where all are free of metastatic deposits. Both resection margins are clear and well away [9].
Immunostains findings stated as CK 7 positive with strong cytoplasmic staining in tumour cells. CK 20 was negative. Finally conclude as moderately differentiated adenocarcinoma of small intestine.
Small bowel is comprised 80% of the gastrointestinal tract but small bowel carcinomas are comparatively rare (<1% of all gastrointestinal malignancies).
Small bowel cancers are more common in men than women and mean age at presentation is 67 years.
The risk factors for small bowel cancers include alcohol consumption, ingestion of smoked foods, salt cured foods, red meats and refined sugars. Majority of small bowel adenocarcinomas are arising from adenomas in the intestinal mucosa. Therefore adenoma-carcinoma sequence which is well described in the large bowel appears to be recapitulated to some extent in the small bowel. However, the exact sequence of genetic changes in the small bowel mucosa has not been well elucidated. Small bowel primary tumours are more frequent in Hereditary Nonpolyposis Colorectal Cancer (HNPCC) and Familial Adenomatous Polyposis (FAP) family members. Majority of the small bowel adenocarcinomas arises in the duodenum, then decrease in incidence from jejunum to ileum [10].
The distribution of small bowel tumors varies between studies but was similar to the findings in this study with 25% of the tumors in the duodenum, 37% in the jejunum, and 38% in the ileum. Several explanations have been proposed to account for this discrepancy. Reasons include the liquid nature of the intestinal contents, which may be less irritating to the mucosa, the rapid transit time in the small bowel that reduces the exposure to carcinogens, a decreased bacterial population to produce carcinogens, the increased lymphoid tissue, an alkaline pH and the presence of the enzyme benzyprene hydroxylase, which helps to detoxify potential carcinogens. The explanation for the infrequent finding of small bowel primary tumors is most likely multifactorial and encompasses all the above theories.
The duodenal adenocarcinoma is usually presents in the 6th and 7th decades. The possible histology from small bowel masses is adenocarcinoma, carcinoid and lymphomas. The commonest site at which adenocarcinomas arises in the small bowel is duodenum. A study done by Tocchi, et al. with 129 patients who was diagnosed to have primary small bowel cancers have found that 33% were adeno carcinomas, 29% were carcinoids and 19% were lymphomas [11].
About 50% of all adenocarcinomas occur in the duodenum, nearly 20% in jejunum and a little over 10% in ileum and 14% occur in unspecified sites according to the national cancer data base in United States.
The majority (2/3) of duodenal adenocarcinomas arises at the periampullary region. The duodenal adenocarcinomas are associated with adenomatous polyposis coli, gardners and turcots syndrome, crohns disease, coeliac disease, lynch syndrome and immunosuppression, etc.
The patients usually present with vague symptoms like intermittent pain due to partial intestinal obstruction, manifestations of upper gastrointestinal bleeding like melena or anaemic symptoms. Some may also present with anorexia and weight loss. However, the extreme rarity and vagueness of symptoms makes it difficult to diagnose these tumours at early stage.
The diagnosis of malignancies beyond the normal reach of upper gastrointestinal endoscope is a challenge. Surgeons and gastroenterologists use several methods to visualise and obtain biopsies from these tumours. There are no specific methods to diagnose these tumours in an early stage. Most of the cases require special investigations for diagnosis. Barium contrast has a diagnostic accuracy of 83%. Enteroclysis was considered as the gold standard for the investigation of small bowel pathologies. However, it is largely replaced by capsular endoscopy and Double Balloon Enteroscopy (DBE). The advantage of double barrel endoscopy is its’ ability to obtain biopsies. It was described by Yamamoto et al l in 2001. Other available methods are Enteroscopy by the "push" method using the paediatric colonoscope or "sonde" enteroscopy.
In general tumours at first and second parts of the duodenum are treated by Whipples' procedure. From third part of the duodenum to proximal illeal tumours can be treated by segmental resection with lymph node clearance. Distal ileal tumours needed to be treated with right hemicolectomy. Tumours at the ligament of treitz is treated by duodenojejunal segmentectomy and duodenojejunal anastomosis.
Adjuvant chemotherapy is widely practising in small bowel cancers even though some studies showed that adjuvant treatment after complete resection has not shown reduction in recurrence.
The small bowel cancers have relatively a bad prognosis with an overall 5 years survival of 17%-25% and median survival of 19.7 months. Bad prognostic features are large tumor size, transmural invasion and moderate to poor tumour grade, nodal metastases, positive margins and tumour staging.
Prognosis is worse in duodenal malignancies. It is mandatory to follow up, these patients closely as there is a high possibility of developing another abdominal carcinoma. Majority of these recurrences are from synchronous polyps that are missed during the initial assessment especially in the duodenum or jejunum. Therefore, it is advisable to assess the upper gastrointestinal tract including the initial part of the jejunum, preoperatively or intra-operatively by way of endoscopy to prevent early recurrence.
Citation: Thilakarathna B, et al. "Adenocarcinoma at the Ligament of Treitz-A Rare Presentation ". Oncol Cancer Case Rep, 2023, 9(2), 1-3
Received: 30-Sep-2022, Manuscript No. OCCRS-22-75203; Editor assigned: 03-Oct-2022, Pre QC No. OCCRS-22-75203 (PQ); Reviewed: 18-Oct-2022, QC No. OCCRS-22-75203; Revised: 13-Feb-2023, Manuscript No. OCCRS-22-75203 (R); Published: 20-Feb-2023, DOI: 10.37532/2471-8556.23.9.2.1-3
Copyright: © 2023 Thilakarathna B, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.