Case Report - (2021) Volume 0, Issue 0
A 4.5-month-old girl presented to us with fever for a total of 10 days, loose stools for 2 days .she took short courses of multiple oral antibiotics during this period but was not relieved. A thorough physical examination was unremarkable her initial investigations were suggestive of urinary tract infection for which broad spectrum antibiotics were started. However, fever still persisted even after 72 hrs of antibiotics. Blood counts showed persistently high TLC and increasing platelet count, along with high CRP. Consequently a diagnosis of Kawasaki Disease (KD) was suspected, which was supported by echocardiographic findings. After she received intravenous immunoglobulins, her fever subsided and lab parameters showed significant improvement. This case highlights an unusual presentation of KD in an uncommonly young age group without much clinical pointers except for persistent fever.
Kawasaki disease • Multiple oral antibiotics • Diagnosis
Kawasaki Disease (KD) is an acute inflammatory vasculitis of small- and medium-sized arteries that can cause coronary artery weakening and aneurysm development in approximately 25% of untreated cases, with increased risks of cardiovascular complications and mortality [1]. Burns, et al. [2-4]. Noted that children of KD in India were older with almost half of them being over the age of five years possibly because it is being missed in infants and young children in whom the condition is being confused with viral exanthemata. Although one or multiple infectious triggers are most likely, the precise etiology is still unknown. Kawasaki disease is primarily a clinical diagnosis but Atypical or incomplete forms of KD are common (15%–20% of all patients) especially in children younger than 6 months [5]. Who also have the highest likelihood of development of coronary artery aneurysm, long term consequences and resistance to therapy [6,7]. In such patients laboratory and echocardiographic data can assist in diagnosis. For this reason it is recommended that any infant <6 months with fever ≥ 7 days without explanation should undergo echocardiography to assess the coronary arteries. Here we report the case of a 4.5-month-old child with an atypical form of KD, without much clinical clues, who developed aneurysm of the coronary arteries.
A full term delivered, previously healthy, 4.5-month-old girl presented at our Emergency Department with fever for a total duration of 10 days, loose stools for 2 days. Fever used to occur 3-4 times a day with a peak of 102-1030F (axillary). Child was apparently well and playful during afebrile period. Her oral intake was normal. She took incomplete course of treatment with drugs like oral amoxicillin+ clavulanic acid, cefixime, cefuroxime during this period. On physical examination, she presented in good general condition, body temperature was 101.4°F, no signs of dehydration (capillary refill time <2 s), mild perianal rash was noted. Rest of the general and systemic examination was normal.
Investigations
Before admission (outside): Showed a very high value of C - reactive protein C-RP: 113.7 mg/L; hemoglobin (Hb) 9.4 g/dL, White Blood Cell (WBC) count 23,670/ mm3 with 56.5% neutrophils, and Platelet (PLT) count 588,000/mm3.Blood culture report was awaited. Malarial antigen report was negative.
On day 1 of admission: Blood tests which had a gap of 2 days showed a similar picture with persistent high value of C-RP 47.5 mg/L, hemoglobin (Hb) 9.3 g/dL, White Blood Cell (WBC) count 24,800/mm3 with 60% neutrophils, and platelet (PLT) count 784,000/mm3. The urine analysis showed plenty of pus cells (35-40/ HPF), transaminases were marginally raised and renal functions were normal. Our patient being a female child of less than 6 months of age with suggestive urine tests we kept high possibility of a urinary tract infection and started with inj. Ceftriaxone and inj amikacin.
On day 3 of admission: Although the fever persisted with minimal variability, the C-RP showed a falling trend 38.3 mg/L, with hemoglobin (Hb) 9.2 g/dL, White Blood Cell (WBC) count 28,400/mm3 with 60% neutrophils, and Plate Let (PLT) count 7,43,000/mm3. The urine analysis showed decrease in pus cells (16-18/ HPF).
On day 4 of admission: Antibiotics were upgraded in view of partial response (decreased CRP and decrease in pus cell in urine)
On day 5 of admission: The fever decreased in intensity but remained well above the base line. The C-RP again increased to 55.0 mg/L, complete blood count showed a similar picture, the only significant change being significant increase in platelet count to 8,03,000/mm3. Transaminases values were also increased SGOT-106.5 U/L, SGPT-151.9 U/L. Initial blood culture and urine culture showed no growth. Repeated detailed clinical examinations were not helpful and child showed no clinical signs suggestive of Kawasaki disease. Hence, in view of persistent fever and lab parameters (Raised C-RP, WBC >15000, elevated ALT levels, platelet counts >4.5 lakhs, urine >10 WBC/hpf), an echocardiogram was performed (Figures 1-3).
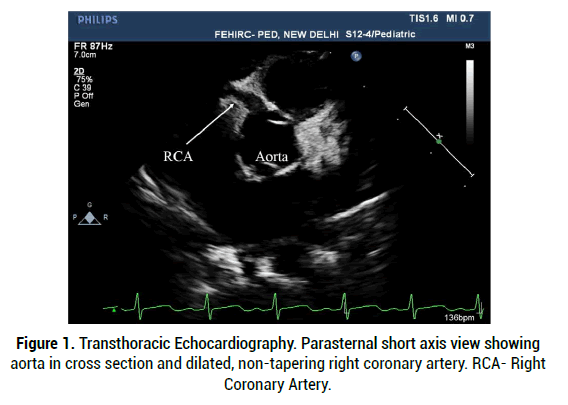
Figure 1: Transthoracic Echocardiography. Parasternal short axis view showing aorta in cross section and dilated, non-tapering right coronary artery. RCA- Right Coronary Artery.
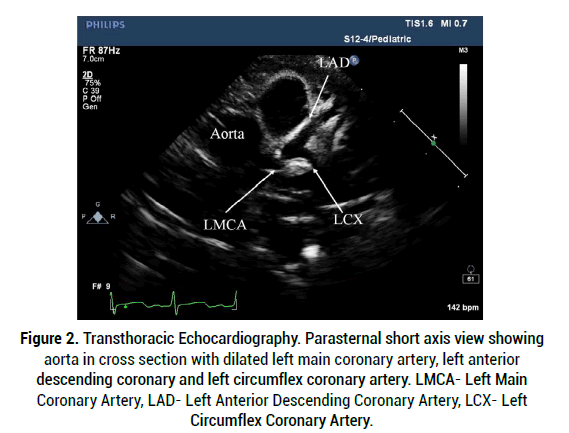
Figure 2: Transthoracic Echocardiography. Parasternal short axis view showing aorta in cross section with dilated left main coronary artery, left anterior descending coronary and left circumflex coronary artery. LMCA- Left Main Coronary Artery, LAD- Left Anterior Descending Coronary Artery, LCX- Left Circumflex Coronary Artery.
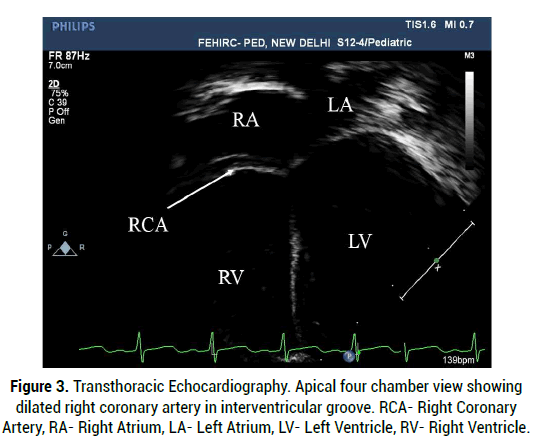
Figure 3: Transthoracic Echocardiography. Apical four chamber view showing dilated right coronary artery in interventricular groove. RCA- Right Coronary Artery, RA- Right Atrium, LA- Left Atrium, LV- Left Ventricle, RV- Right Ventricle.
Interpretation summary
Trace tricuspid regurgitation, trace pulmonic regurgitation, and trace pericardial effusion, dilated coronary arteries as mentioned in above Figures.
Left main coronary artery=4.1 mm (Z score +6.9)
Left anterior descending coronary – 2.4 mm (Z score +4.2)
Left circumflex coronary artery-1.8 mm (Z score +2.5)
Right coronary artery-3.4 mm (Z score +7.7).
With the above findings the diagnosis of KD with medium sized coronary artery aneurysm was made according to the American Heart Association (AHA) criteria [6]. She received intravenous immunoglobulin (IVIG infusion of 2 g/kg) and highdose oral acetylsalicylic acid (100 mg/kg/day).
Outcome and follow-up
After administration of IVIG and aspirin, the fever dramatically defervesced in the following 24 hours. The TLC dropped down to 15000/mm3 and C-RP was reduced to 18mg/L after 48 hours of afebrile period the dose of aspirin was changed to 5mg/kg and the child was discharged.
KD is an acquired heart disease most common in infants aged 6 months to 2 years. It is challenging to make a diagnosis of incomplete KD, particularly in infants younger than 6 months with fewer clinical manifestations [8-10]. Ram Krishna, et al. [11]. studfied the predfictors of coronary artery aneurysm. They suggested that anemia; low albumin, elevated ESR, elevated CRP, and pyuria are the risk factors of coronary artery abnormalities. The most common complications of KD include coronary artery dilatation caused by coronary artery vasculitis and aneurysm [12]. Other complications include decreased coronary arterial compliance, my pericarditis, arrhythmias, ischemic heart disease, pericardial effusion, valvular regurgitation, myocardial infarction, and sudden cardiac death. Prompt diagnosis and administration of IVIG within 10 days, or ideally before day 7 of the disease, is mandated in order to reduce such cardiac complications [13]. Since diagnosing KD in infants younger than 6 months is difficult, any febrile infant who has fever for 7 days or more without other explanations, even without any clinical clues of KD, should receive a blood analysis of systemic vascular response. If the ESR or CRP is elevated, echocardiography should be performed [14]. Unfortunately in our case the patient presented on 10th day of fever without any supportive clinical findings of KD and the preliminary tests pointed towards UTI. The fall of C-RP initially, decrease in pus cells in urine and relative decrease in fever spikes after the start of IV antibiotics led to further delay in clinching the diagnosis. Persistent increase in platelet count was one marker that helped us strongly suspect of Kawasaki disease. Apart from medium sized aneurysm in coronary arteries, there were no other complications.
Kawasaki Disease (KD) should be considered in infants less than 6 months even though the incidence is low in this age group. In Such children ,a significant proportion would not fulfil the diagnostic criteria as many would have ‘incomplete’ and ‘atypical’ forms of disease and unfortunately this age group is most vulnerable to development of coronary artery aneurysm. Hence it is recommended that any infant of age <6 months with fever for ≥ 7 days without explanation should undergo echocardiography to assess the coronary arteries.
This case report, including the cost to publish in open access, is self-financed by the first author.
The authors declare no conflict of interest.
Citation: Siddiqui K. A Typical Kawasaki Disease in an Early Infant a Diagnostic Challenge: Case Report. Med Rep Case Stud, 2021, 06(S4), 014-015
Received: 22-Sep-2021 Published: 13-Oct-2021, DOI: 10.35248/2572-5130.21.s4.014-015
Copyright: © 2021 Siddiqui K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO