Case Report - (2025) Volume 11, Issue 2
It is the first time to report a coincidence of nasopharyngeal carcinoma and pituitary adenoma in a 36-year-old female with a history of chronic nocturnal headaches in the temporal region. The nasopharyngeal mass was missed during the initial visits as the patient was evaluated due to the secreting pituitary adenoma. Her initial symptoms were six months of amenorrhea, massive bilateral galactorrhea and typical clinical signs of acromegaly. It was just during the rhinoplasty that the nasopharyngeal mass was detected for the first time, using the endoscope. Histopathology reported non-keratinizing nasopharyngeal carcinoma (differentiated) and also pituitary adenoma. During the radiotherapy for the nasopharyngeal carcinoma, the patient showed visual symptoms including ptosis and outward deviation of the eye. Since the patient did not consent to the excision of the pituitary adenoma, the field of radiotherapy was increased to include the pituitary adenoma as well. As a result, after three months, all the patient's symptoms, including headache and vision problems, were completely resolved. There was no evidence of recurrence or disease progression on follow-up after 14 months.
Non-Keratinizing Nasopharyngeal Carcinoma (NKAC) • Epstein-Barr Virus (EBV) • Prolactin • Histopathology • Pituitary hormones
The World Health Organization (WHO) has classified the nasopharyngeal carcinomas into three types: Keratinizing squamous cell carcinoma, non-keratinizing carcinoma and basaloid squamous cell carcinoma [1]. Non-Keratinizing Nasopharyngeal Carcinoma (NKAC) is the most common variant of nasopharyngeal carcinoma and can be further subclassified as either differentiated or undifferentiated, although this has no effect on treatment or outcome [2]. It is characterized by the absence of keratin production, which differentiates it from other forms. There are several risk factors associated with NKAC, including Epstein-Barr Virus (EBV) infection, Asian descent, positive family history, exposure to tobacco and alcohol and certain environmental factors, such as wood dust, formaldehyde and nickel and certain genetic variations [3]. The treatment of non-keratinizing nasopharyngeal adenocarcinoma typically involves a combination of surgery, radiation therapy and chemotherapy. The specific treatment plan will depend on the stage and extent of the cancer, as well as the overall health of the patient [4].
Pituitary adenomas are usually noncancerous (benign) and slow growing, but they can cause several health problems, including a condition called acromegaly. The risk of developing pituitary adenoma increases with age, with most cases occurring in adults between the ages of 30 and 50. Pituitary adenomas are slightly more common in women than in men. Certain hormonal imbalances, such as excessive growth hormone (acromegaly) or prolactin (prolactinoma), can increase the risk of pituitary adenoma. Some studies suggest that smoking and heavy alcohol consumption may increase the risk of developing pituitary adenoma, although more research is needed to fully understand the association. Treatment for pituitary adenoma and acromegaly aims to reduce the production of excess growth hormone and alleviate symptoms. The primary treatment option is usually surgery to remove the tumor from the pituitary gland. However, in some cases, the tumor may be too large or located in a difficult-to-reach area, making complete removal impossible. In such instances, other treatment modalities, including medications and radiation therapy, may be used to control the hormone levels.
In this case report we presented a case of NAKC concomitant with a pituitary adenoma, while NAKC was detected during rhinoplasty as a rehabilitation after her acromegaly treatment. To our knowledge, this is the first time to report coincidental NAKC and pituitary adenoma in a patient.
We present the case of a 36-year-old female with a history of chronic nocturnal headaches in the temporal region since 2020. Except for many years of tobacco use, the patient did not mention any history of environmental exposure or positive family history. When she was visited in 2022, she was referred to an endocrinologist because of six months of amenorrhea, massive bilateral galactorrhea and typical clinical signs of acromegaly including enlarged hands and feet, enlarged nose, thickened lips, enlarged tongue and headaches. Magnetic Resonance Imaging (MRI) of the pituitary gland with and without GD injection revealed evidence of sellar enhancing mass lesion measures 30 × 28 × 15 mm extending to suprasellar cistern leading to depression of sellar floor due to pituitary macroadenoma. Faint homogenous enhancement in mentioned lesion after contrast injection was seen. Extension of the lesion to suprasellar cistern was noted causing compression of optic chiasma. Involvement of right cavernous sinus was seen, but left cavernous sinus appeared normal in shape and signal intensity. Further investigations showed a high serum level of Prolactin (PRL) (105 ng/ml) and IGF-1, as a primary mediator of Growth Hormone (GH) (830.7 ng/ml), as well as basal GH concentrations of 22.4. Levels of all other pituitary hormones were within reference ranges.
With the diagnosis of functional pituitary secreting PRL and GH, she was treated with a combination of octreotide LAR, cabergoline and dopamine analogue. After one year of medication and the patient's lack of consent for surgery to excise the tumor, despite the relative improvement of some symptoms such as galactorrhea, the level of IGF-1 was still high (267 ng/ml). Despite the patient's refusal to undergo surgery for pituitary adenoma excision, she was referred for rhinoplasty in 2023, and during the operation, the surgeon noticed a large mass in the nasopharynx. Using endoscopy, excision of the nasopharyngeal mass was done, while the mass that was seen in the base of the skull during endoscopy was also sampled. Histopathology reported non-keratinizing nasopharyngeal carcinoma (differentiated) and also pituitary adenoma. Microscopic exam revealed interconnecting cords and large trabeculae of tumor cells with no evidence of keratinization. Tumor cells showed rather well-defined cell borders, increased nuclear/cytoplasmic ratio, oval or round vesicular nuclei and prominent nucleoli, interspersed by a fibrotic stroma with dense lymphoplasmacytic infiltrate (Figure 1). Since the nasopharyngeal mass was missed in the first radiologic report, we assessed the MRI again. An axial post-contrast, fat-saturated T1 images showed a large enhancing nasopharyngeal mass extended superiorly from the roof of the nasopharynx into the bilateral cavernous sinus (more in left), traversing skull base. There was extension along the dura of the floor of the left middle cranial fossa, involving of left temporal lobe. Findings were infavor of nasopharyngeal carcinoma with intracranial invasion (Figure 2).
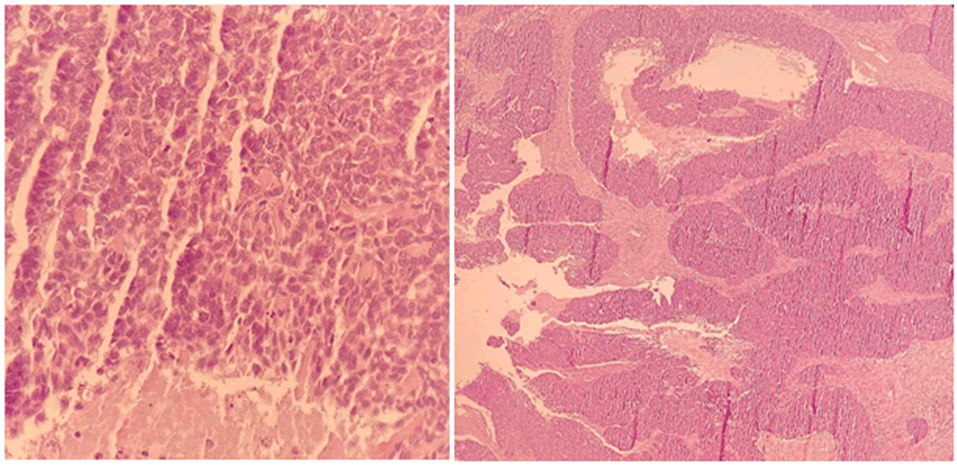
Figure 1. Nasopharyngeal carcinoma, non-keratinizing, differentiated subtype.
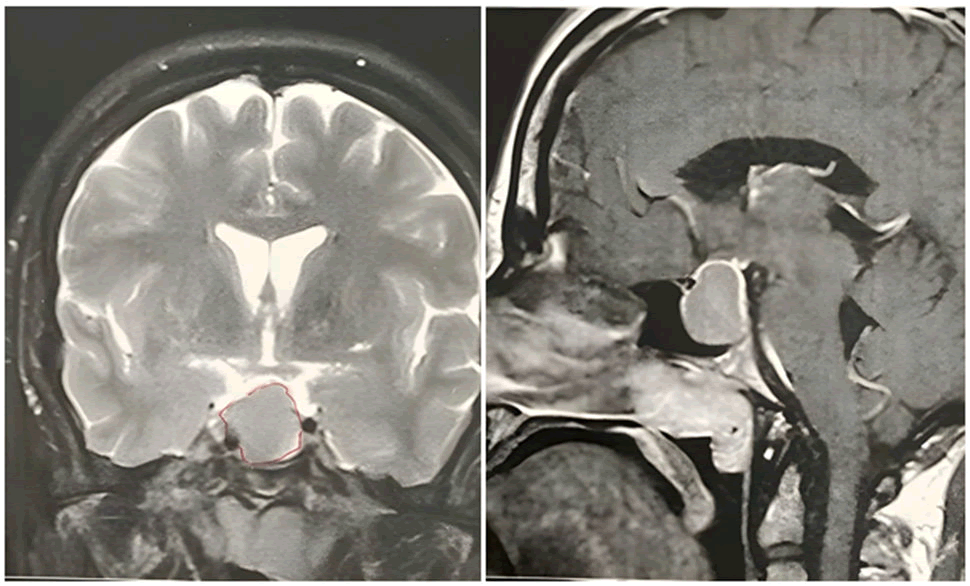
Figure 2. A large enhancing sellar mass with suprasellar extension and optic chiasm compression is noted infavor of pituitary macroadenoma and a nasopharyngeal carcinoma with intracranial invasion.
With the new diagnosis of NKAC, the patient underwent a full tumor work-up including the cervical, chest and mediastinal CT scan and the PET scan. Positive findings were a 5 mm subpleural nodule in the medial segment of the right lower lobe and a hypodense nodule in the right thyroid lobe which was reported as benign follicular (Bethesda II) when fine needle aspiration was performed. At the time of diagnosis, the patient showed a positive plasma serology for the Epstein-Barr Virus (EBV).
In conclusion, we faced an NKAC tumor of the nasopharynx (T2N0M0) which was missed in the initial assessments and was excised later during rhinoplasty and a coincidental functional pituitary adenoma which was treated non-surgically. To complete the treatment of NAKC, the patient underwent a standard combination of concurrent chemo and radiotherapy (50 mg/m2 cisplatin weekly and 70Gy/35 fractions). During the chemoradiation therapy, following the increase in the size of the pituitary adenoma, the patient showed signs of pressure on the 3rd and 6th cranial nerves (ptosis and outward deviation of the left eye). Since the patient did not consent to the excision of the pituitary adenoma, the field of radiotherapy was increased to include the pituitary adenoma as well. As a result, after three months, all the patient's symptoms, including headache and vision problems, were completely resolved. There was no evidence of recurrence or disease progression on follow-up after 14 months, which included post-treatment MRI and PET-CT scans.
Diagnosis of nasopharyngeal carcinoma is usually difficult at the initial stages since the patient occasionally does not present any nasal symptoms [5]. In this report, despite the obvious nasopharyngeal mass in the first MRI of the patient, when she was referred because of acromegaly and galactorrhea, it was missed by both the radiologist and endocrinologist. To our knowledge, it is the first time that the coincidence of NAKC and pituitary adenoma is reported. Nasopharyngeal masses usually do not demonstrate clinical symptoms until the advanced stages when the mass is big enough to obstruct the eustachian tube (leading to serous otitis media) or cranial nerves (leading to headache or visual loss) [6,7]. However, it the current case, the patient did not have any ear pain. All symptoms manifested in the patient of this study were due to pituitary adenoma, as they persisted after resection of the nasopharyngeal tumor, but disappeared when the radiotherapy field was widened enough to include the pituitary tumor. However, headache and visual disturbance have been reported to be the only symptoms of nasopharyngeal carcinoma. This highlights the importance of considering the nasopharyngeal cavity in patients undergoing MRI due to any medical suspicion. Studies have demonstrated that MRI has a high sensitivity and specificity in diagnosis of nasopharyngeal carcinomas [8].
A large body of evidence supports the role of the EBV as the most common risk factor for nasopharyngeal carcinomas [9]. In the current case, the patient was not only positive for EBV, but also was born in an endemic region for the NKAC [10]. However, this is the first time that the coincidence of these two types of tumors is reported, there is a possibility that some reasons for the occurrence of these two types of tumors are the same. Among the risk factors mentioned for each of these two types of tumors, exposure to tobacco is the only common factor, which was also seen in this patient. Using the human gene database (GeneCards®), an RNA gene called MEG3 (Maternally Expressed 3) was found to be a common gene between these two masses with a high relevance score of 92.08 (Figure 1) [11]. It can be a direction for future researchers to be more specific on the common genomic origin of these two tumors. Recently, studies have highlighted the genomic aspects of nasopharyngeal carcinoma, suggesting the emergence of new therapeutic targets and biomarkers for this malignancy [12]. MEG3 can be suggested as one of these therapeutic targets.
Until it is determined that the presence of these two types of tumors in the same person is just a coincidence or has a common cause, practitioners should pay more attention to accompanying cases such as nasopharyngeal carcinomas when examining the disease with pituitary adenoma.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Received: 04-May-2024, Manuscript No. OCCRS-24-131406; Editor assigned: 06-Apr-2024, Pre QC No. OCCRS-24-131406 (PQ); Reviewed: 20-Apr-2024, QC No. OCCRS-24-131406; Revised: 21-Apr-2025, Manuscript No. OCCRS-24-131406 (R); Published: 28-Apr-2025, DOI: 10.35248/2471-8556.25.11(1).001-009
Copyright: © 2025 Bahador M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.