Research Article - (2021) Volume 6, Issue 6
With increased air pollution level there is certainly health impact on human health, it is crucial to estimate the public health relevance of the problem. The public health impact of smoking, environmental tobacco smoke, and air pollution on the prevalence of chronic cough/phlegm were estimated. Health impact assessment studies clearly suggest that public health largely benefits from better air quality. The studies are selective underestimates as they are strongly driven by full quantification of the impact on morbidity and their consequences on quality of life among the diseased and the caregivers. Ludhiana city was identified as critically polluted city by Central Pollution Control Board. A cross-sectional study was conducted to estimate the effects of air pollution on mortality. A cross-sectional study was conducted in Ludhiana city of Punjab located in northern India. Air pollution and morbidity data was collected from 2003 to 2004. SPM was measured by Gravimetric method and NOx and SO2 by chemical method. SPM daily average level was attempted by combining 24-hour average of the stations working on a particular day. Levels of SPM were more than permissible limit in Industrial (814.2-559.2 mg/m3) and residential areas (590.2-290.8 mg/m3) as compared to Samrala (358.2-239.7 mg/m3). Levels of NOx (19.1 mg/m3) and SOx (26.2 mg/m3) were under permissible limit in both the towns. In Ludhiana, air pollution level is quite high and is still rising. The air pollution level was high was found to be significantly associated with respiratory and cardiovascular morbidity.
Public health • Air pollution • Morbidity • Quantification study
With the rising pace of industrialization, the quality of air is being compromised world over. As a matter of fact, the air had never been pure as foreign substances are invariably present in the air at all times and at all places. The term air pollution becomes applicable when an excessive concentration of foreign matter in the outdoor atmosphere begins to have harmful impact on the human beings or their surrounding environment. Natural air pollution sources include fires, wind erosion, volcanic activities etc. Anthropogenic air pollution is caused by various man made activities like industries, motor vehicles, and domestic and agriculture sources. Air pollution has become a major environmental problem affecting the developed and the developing countries alike. Air pollutants are usually classified as suspended particulate matter (dust, fumes, mists, and smokes), gaseous pollutants (gases and vapours) and odours. Current techniques measure the mass concentration of particles in air using size-specific sampling devices. The impact of air pollution on the respiratory health has been studied world over. High levels of exposure to air pollutants produce symptoms of both upper and lower respiratory tract irritation and increase the severity of respiratory diseases like asthma and chronic bronchitis. When air pollutants are inhaled they may affect other body systems as well. For example, benzene affects the bone marrow, metallic mercury has an adverse effect on the kidneys and the central nervous system and carbon disulphide affects the cardiovascular and the nervous system. Several studies have established the association of air pollution with cardio-respiratory mortality [1]. Short term exposure to outdoor air pollution has been linked to adverse health effects, including increased mortality, rates of hospital admissions and emergency department visits, and decreased lung function [2]. These acute effects are attributed to the exacerbation of pre-existing cardio-respiratory conditions [3]. Crosssectional studies have also reported association of respiratory symptoms with poor ambient air quality [4-6]. Cohort studies have shown deterioration in lung function with air pollution [7,8]. Recent multi city analyses conducted in U.S., Canada and Europe provide further evidence supporting the coherence and plausibility of this association [9-13]. Most of the studies on air pollution and health have been conducted in industrialized countries of the North. The climatic conditions, characteristics of the population, and the composition of air pollutants may have important bearing on the health effects of air pollution. Not only the physical form and properties of the air born particles influence their distribution in the environment, but concentration of the particles also depend upon the wind-speed and the stability of the atmosphere which is responsible for the upward diffusion of the pollutants. Thus, studies need to be conducted in developing countries also, where the characteristic of outdoor pollution, meteorological conditions and socio demographic patterns differ from North America and Western Europe [14]. In India, many cities are experiencing heavy air pollution [15]. An ecological study carried out recently among the residents of an industrial town of Punjab has shown association of outdoor air pollution with chronic respiratory morbidity [16]. Acute effects also need to be studied so that a comprehensive policy can be evolved for prevention of the health effects of air pollution. Therefore, a cross-sectional study was carried out among the residents of an industrial town vs non-industrial town of Punjab with high level of air pollution and chronic respiratory and cardiovascular morbidity in Northern India.
The study was carried out in Ludhiana city which is the largest City of Punjab state in northern India with population of 1.5 million and having area of 135 square kilometres. Major sources of pollution are: Vehicular emissions, industries, domestic and agricultural waste burning. This city is located at a distance of about 100 km from Chandigarh and about 360 km from New Delhi. Three areas were randomly selected from the industrial, commercial and residential areas of Ludhiana city and fourth area was selected from a non-industrial area as reference population, i.e. Samrala. A cluster sampling method was used to select the area. In the randomly selected four different areas, initially field investigators did a cross-sectional household survey. By using a semi-structured questionnaire, socio-demographic characteristics important life-style and household information of the individuals residing in the area was collected. Detailed interview of the household members has been done to find their morbidity status. Air quality was monitored for SPM, NOx and SO2 using high volume air sampler. Gravimetric method is used for SPM and chemical method for NOx and SO2. Eight-hourly averaging is done for RSPM and 4-hourly average is done for NOx and SO2. Bureau of Indian Standard (BIS) is used for monitoring these air pollutants [17-19]. Air quality was monitored intermittently at three sites (Figures 1 and 2). Air sampling sites have been selected so as to be representatives of different areas of the city, however, the city is not a very well planned and industrial, commercial and residential areas are not separated. Residences are in the close proximity of the industries. Air quality data was collected for the years, i.e., 2003 and 2004 for all the criteria air pollutants, i.e., RSPM, NOx and SO2. The data was checked for quality and consistency. Recording of air quality for > 75% of the time in a day was taken as a complete daily recording, i.e., all the three 8-hourly recoding for RSPM and at least five out of the six 4-hourly recording for NOx and SO2. City daily average was derived by averaging the daily average of each of the station available for that day from three monitors which worked till end of the study.
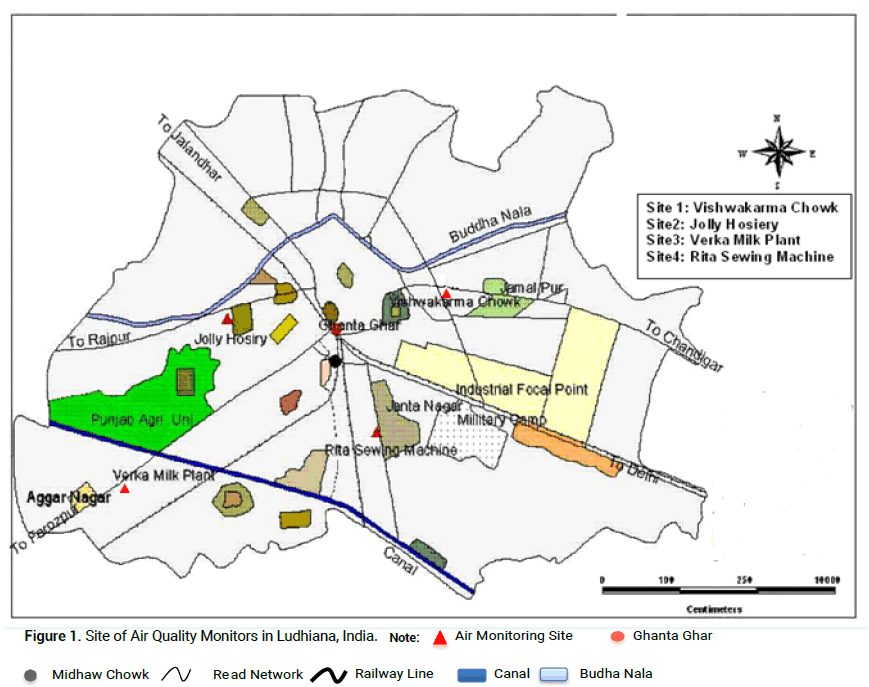
Figure 1: Site of Air Quality Monitors in Ludhiana, India. Note:

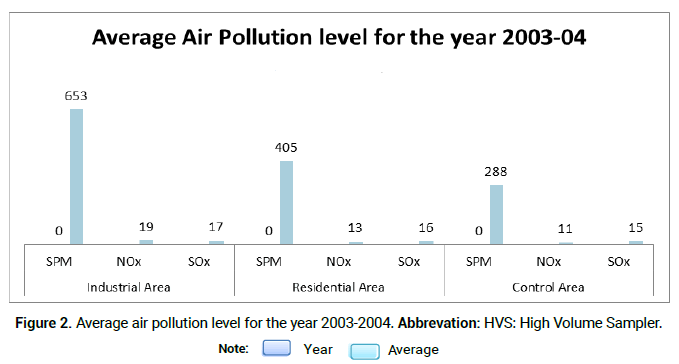
Figure 2: Average air pollution level for the year 2003-2004. Abbrevation: HVS: High Volume Sampler. Note:

Air pollution
Concentration of all the air pollutants was higher in Ludhiana as compared to Samrala. Levels of SPM were more than permissible limit in Industrial (814.2- 559.2 mg/m3) and residential areas (590.2-290.8 mg/m3) as compared to Samrala (358.2-239.7 mg/m3). Levels of NOx and SOx were under permissible limit in both the towns (Tables 1 and 2).
| Station→ | Industrial area | Residential area | Control area | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Month/ Year |
SPM | NOx | SOx | SPM | NOx | SOx | SPM | NOx | SOx |
| (In mg/m3) | (In mg/m3) | (In mg/m3) | |||||||
| Aug.2003 | 814.2 | 18.2 | 11.4 | - | - | - | - | - | - |
| Sept.2003 | - | - | - | 590.2 | 12.2 | 17.4 | 358.2 | 10.2 | 15.2 |
| Oct.2003 | 559.2 | 18.8 | 26.2 | - | - | - | - | - | - |
| Nov.2003 | - | - | - | 332.7 | 14.2 | 18.6 | 239.7 | 12.2 | 16.5 |
| Dec.2003 | 586.1 | 19.1 | 12.2 | - | - | - | - | - | - |
| Jan.2004 | - | - | - | 290.8 | 13.1 | 14.1 | 266.8 | 11.1 | 13.1 |
Table 1. Ambient air quality with respect to SPM, NOx, SOx.
|
SPM (mg/ m3) | Nox (mg/ m3) | Sox (mg/ m3) |
|---|---|---|---|
| Industrial and Mixed Use Area | 500 | 120 | 120 |
| Residential and Rural Area | 200 | 80 | 80 |
| Sensitive Area | 100 | 30 | 30 |
Table 2. The National Standards are
Health status
Socio-economic status was higher of peoples living in the control, commercial and residential area as compared to industrial area according. Low-income settlement was higher in industrial area. Pucca houses were higher as compared to semi-pucca house in all the four areas. Most of the people live in their own houses. Ventilation condition was good in industrial, commercial, residential and control areas. Location of kitchen was indoor in all the house in all the four areas i.e. industrial, commercial, and residential and control area. Kitchen was separated in most of the houses in all the four areas. LPG was used by 79.2% in industrial area, 81.6% in commercial, 78.8% in residential area and 70.4 % in control area. Whereas kerosene was used by 17.6% in industrial area, 19.6% in commercial, 12.0% in residential area and 11.6% in control area. Wood was used by 1.6% in industrial area, 2.4% in commercial, 8.0% in residential area and 28.0% in control area. Only 2.8% used other fuels in industrial area. Vehicular pollution due to heavy and moderate type of vehicles was in Ludhiana whereas Light vehicles were more in Samrala. Width of road is more in Ludhiana as compared to Samrala. More wide roads in residential area as compared commercial and industrial area. Vehicular piles of heavy-duty trucks and buses were higher in Ludhiana as compared to two wheelers that are more in Samrala. Parked vehicles were higher in control area as compared to Ludhiana. There was no much difference in windows facing towards road, but more windows were opened in Ludhiana as compared to Samrala. More industries were located at a distance of approx. <2.0 km in Ludhiana as compared to Samrala. Protectives gloves, hanky, hanky and gloves both, sun glasses, towels, vizier were used more commonly in Ludhiana as compared to Samrala. Subjects of Ludhiana commonly used hanky and gloves as protective equipment. Indoor workers i.e. Factory and office workers were higher in Ludhiana whereas outdoor workers wore higher in Samrala. Present and previous fumes, vaporous and dust exposure was more in Ludhiana. More workers missed their work due to Illness. According to perception, industrial air pollution is a major problem in industrial area (96.0%), in commercial (31.2%) and in residential area (27.6%) as compare to control area (0.0%). Vehicular air pollution is also a major problem according to perception, in industrial area (17.6%), in commercial (11.2%) and in residential area (27.6%) as compare to control area (0.0%). Smokers were more in commercial (15.1%) and residential (12.3%) as compared to industrial (10.1%) and control area (11.2%).
In adults of industrial, commercial and residential areas symptom of cough (11.1%, 8.6%, 4.9% respectively), sputum (9.6%, 7.3%, 3.9% respectively), breathlessness (10.6%, 4.2%, 3.4% respectively) and wheezing (3.5%, 1.3%, 0.3% respectively) were more as compared to control area i.e. cough (6.5%), sputum (5.4%), breathlessness (2.0%) and wheezing (0.2%). Symptoms of ever had pain in his chest were higher, in industrial area (8.2%) and in commercial (6.4%) as compare to in residential area (3.8%) and control area (4.6%). High BP problem were more in industrial area (14.6%), in commercial (17.9%) and in residential area (15.7%) as compare to control area (9.4%). Problem of ever having chest pain was in 8.2% industrial, 6.4% commercial and 3.8% residential areas as compared to 4.6% control areas. Problem of BP was in 14.6% industrial, 17.9% commercial and 15.7% residential areas as compared to 9.4% control areas. Gastric problem was also higher in Ludhiana as compared to Samrala. Vector borne diseases i.e. malaria, dengue, were higher in Ludhiana as compared to control area. Eye irritation (21.7%, 22.4%, 12.4% respectively), redness of eyes (16.3%, 11.0%, 6.7% respectively) watery discharge (18.1%, 14.2%, 8.8% respectively) was higher in industrial, commercial and residential areas as compared to control. Ratings of health status of children’s (<20 years) were excellent and good in control (26.5% and 67.5%) and residential areas (32.7% and 56.6%) as compared to industrial (21.8% and 75.1%) and commercial areas (14.6% and 80.9%). Premature birth in industrial (5.4%), commercial (0.8%) and residential areas (3.6%) were more as compared to control area (0.2%). Child missed there school due to illness more in industrial and commercial areas as compared to residential and control areas. Chest illness before the ages of 2 years were higher in industrial (13.8%), commercial (9.6%) and residential areas (7.0%) as compared to control areas (6.5%) but there were no difference in asthmatic children's in all these four areas. Illness in last three months, number of unable days to do work and doctor visit regarding this problem was more in Ludhiana as compared to Samrala (Tables 3-16).
| Variables | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Total family members | ||||
| 1-2 | 39 (15.6) | 23 (9.2) | 23 (9.2) | 25 (10.0) |
| 3-5 | 148 (59.2) | 189 (76.2) | 174 (69.6) | 180 (72.0) |
| >5 | 63 (25.2) | 38 (15.2) | 53 (21.2) | 45 (18.0) |
| No. of rooms | ||||
| 1-2 | 133 (54.0) | 169 (67.6) | 123 (49.2) | 143 (57.2) |
| 3-5 | 100 (40.0) | 75 (30.0) | 124 (49.6) | 107 (43.2) |
| >5 | 15 (6.0) | 6 (2.4) | 3 (1.2) | 0 (0.0) |
| Housing conditions | ||||
| Type of locality slums | 110 (44.0) | 181 (72.4) | 144 (57.6) | 119 (47.6) |
| Low income settlement | 128 (51.2) | 47 (18.8) | 102 (40.8) | 102 (40.8) |
| High income settlement | 12 (4.8) | 22 (52.4) | 4 (1.6) | 4 (1.6) |
| Type of house | ||||
| Pucca | 205 (82.0) | 204 (81.6) | 201 (80.4) | 225 (26.9) |
| Semi-pucca | 45 (27.3) | 46 (27.9) | 49 (29.7) | 25 (15.2) |
| Ownership | ||||
| Owner | 165 (66.0) | 196 (78.4) | 191 (76.4) | 227 (90.8) |
| Tenant | 85 (34.0) | 54 (21.6) | 59 (23.6) | 23 (9.2) |
Table 3. Household Conditions.
| Indoor air quality | Industrial Area | Commercial Area | Residential Area | Control Area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Kitchen | ||||
| Indoor | 230 (92.0) | 243 (97.2) | 227 (90.8) | 206 (82.4) |
| Outdoor | 20 (8.0) | 7 (2.8) | 23 (9.2) | 44 (17.6) |
| Kitchen ventilation | ||||
| Good | 107 (42.8) | 97 (38.8) | 118 (26.3) | 127 (50.8) |
| Moderate | 74 (29.6) | 96 (38.4) | 81 (32.4) | 67 (26.8) |
| Bad | 49 (19.6) | 50 (20.0) | 28 (11.2) | 12 (4.8) |
| Hours spend in the cooking in kitchen | ||||
| <1 | 12 (4.8) | 5 (2.0) | 14 (5.6) | 2 (0.8) |
| 1-3 | 226(90.4) | 243(97.2) | 231(92.4) | 212(84.8) |
| >3 | 12(4.8) | 2(0.8) | 5(2.0) | 36(14.4) |
| Kitchen Separated | ||||
| Yes | 172 (68.8) | 161 (64.4) | 171 (68.4) | 195 (78.0) |
| No | 78 (31.2) | 89 (35.6) | 79 (31.6) | 55 (22.0) |
| Type of fuel used | ||||
| LPG | 198 (79.2) | 204 (81.6) | 222 (78.8) | 176 (70.4) |
| Kerosene | 44 (17.6) | 49 (19.6) | 30 (12.0) | 29 (11.6) |
| Wood | 4 (1.6) | 6 (2.4) | 20 (8.0) | 70 (28.0) |
| Others | 7 (2.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Smokers in the house | ||||
| Yes | ||||
| No | 56 (22.4) | 84 (33.6) | 59 (23.6) | 69 (27.6) |
| 194 (77.6) | 166 (66.4) | 191 (76.4) | 181 (72.4) | |
Table 4. Indoor air quality.
| Present in Home | Industrial area | Commercial area | Residential area | control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Animals | ||||
| Yes | 4 (1.6) | 1 (0.4) | 21 (8.4) | 60 (24.0) |
| No | 246 (98.4) | 249 (99.6) | 229 (91.6) | 190 (76.0) |
| Pets | ||||
| Yes | 5 (2.0) | 29 (11.6) | 48 (19.2) | 29 (11.6) |
| No | 245 (98.0) | 221 (88.4) | 202 (80.8) | 221 (88.4) |
Table 5. Presence of pets and animals.
| Vehicular pollution | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Width of road (meter) | ||||
| <4 | 125 (50.0) | 50 (20.0) | 25 (10.0) | 150 (60.0) |
| 4-6 | 125 (50.0) | 200 (80.0) | 225 (90.0) | 100 (40.0) |
| Vehicular traffic | ||||
| Heavy | 27 (10.8) | 9 (3.6) | 24 (9.6) | 0 (0.0) |
| Moderate | 131 (52.4) | 117 (46.8) | 60 (24.0) | 8 (3.2) |
| Light | 92 (36.8) | 124 (49.6) | 166 (66.4) | 242 (96.8) |
| Vehicle piles | ||||
| Heavy duty trucks | 25 (10.0) | 9 (3.6) | 24 (9.6) | 0 (0.0) |
| Buses | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Passenger cars | 26 (10.4) | 16 (6.4) | 59 (23.6) | 6 (2.4) |
| Auto rickshaws | 0 (0.0) | 0 (0.0) | 8 (3.2) | 0 (0.0) |
| Two wheelers | 199 (79.6) | 225 (90.0) | 159 (63.6) | 244 (97.6) |
| Parked vehicles | ||||
| Yes | 80 (32.0) | 109 (43.6) | 69 (27.6) | 2 (0.8) |
| No | 170 (68.0) | 141 (56.4) | 181 (72.4) | 248 (99.2) |
Table 6. Vehicular pollution.
| Windows | Industrial area | Commercial area | residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Facing the outside | ||||
| Yes | 73 (29.2) | 67 (26.8) | 50 (20.0) | 70 (28.0) |
| No | 177 (70.8) | 183 (73.2) | 200 (80.0) | 180 (72.0) |
| Mostly | ||||
| Closed | 62 (24.8) | 62 (24.8) | 40 (16.0) | 70 (28.0) |
| Open | 11 (4.4) | 5 (2.0) | 10 (4.0) | 0 (0.0) |
Table 7. Presence of window.
| Industrial air pollution | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Industry closed to residence | ||||
| Yes | 250 (100.0) | 250 (100.0) | 250 (100.0) | 250 (100.0) |
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| App. distance of industry from residence (km) | ||||
| <0.5 | 97 (38.8) | 70 (28.0) | 0 (0.0) | 225 (90.0) |
| 0.5-2.0 | 152 (60.8) | 142 (56.8) | 73 (29.2) | 0 (0.0) |
| >2.0 | 1 (1.4) | 38 (15.2) | 177 (70.8) | 25 (10.0) |
| Protective used | ||||
| Yes | 16 (6.4) | 39 (15.6) | 47 (18.8) | 0 (0.0) |
| No | 234 (93.6) | 211 (84.4) | 203 (81.2) | 250 (100.0) |
| Amount spent (Rs.) | ||||
| <5000 | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| ³ 5000 | 15 (6.0) | 39 (15.6) | 47 (18.8) | 0 (0.0) |
| Mostly travel on congested roads | ||||
| Yes | 40 (16.0) | 89 (35.6) | 58 (23.2) | 50 (20.0) |
| No | 106 (42.4) | 65 (26.0) | 120 (48.0) | 61 (24.4) |
| Protective equipment used | ||||
| Yes | 22 (8.8) | 26 (10.4) | 32 (12.8) | 0 (0.0) |
| No | 124 (49.6) | 128 (51.2) | 146 (58.4) | 111 (44.4) |
| Type of protective used filter | ||||
| Gloves | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hanky | 0 (0.0) | 1 (0.4) | 0 (0.0) | 0 (0.0) |
| Hanky and gloves | 16 (6.4) | 25 (10.0) | 28 (11.2) | 0 (0.0) |
| Sun glasses | 1 (0.4) | 0 (0.0) | 1 (0.0) | 0 (0.0) |
| Towels | 3 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Vizier | 0 (0.0) | 0 (0.0) | 31 (1.2) | 0 (0.0) |
| 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.00) | |
| Cost of protective used (Rs.) | ||||
| <10 | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 10-50 | 18 (7.2) | 26 (10.4) | 32 (12.8) | 0 (0.0) |
| >50 | 3 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Diversion to avoid vehicular emissions | ||||
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| No | 146 (58.4) | 154 (61.6) | 178 (71.2) | 111 (44.40) |
Table 8. Industrial air pollution.
| Interview | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Proxy | 447 (40.8) | 519 (48.7) | 512 (46.5) | 533 (49.3) |
| Direct | 649 (59.2) | 546 (51.3) | 588 (53.5) | 548 (50.7) |
Table 9. Distribution of interview.
| Smoking | Industrial area | commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Smoker | 75 (10.1) | 104 (15.1) | 88 (12.3) | 71 (11.2) |
| Non-smoker | 667 (89.9) | 585 (84.9) | 627 (87.7) | 564 (88.8) |
| Type of tobacco smoke | ||||
| Cigarette | 27 (36.0) | 19 (18.3) | 29 (33.0) | 16 (22.5) |
| Bidi | 47 (62.7) | 84 (80.8) | 56 (63.6) | 55 (77.5) |
| Hukka | 1 (1.3) | 0 (0.0) | 1 (1.1) | 0 (0.0) |
| Others | 0 (0.0) | 1 (1.0) | 2 (2.3) | 0 (0.0) |
| Frequency of smoke | ||||
| <3 | 20 (26.7) | 7 (6.7) | 4 (4.6) | 5 (6.0) |
| 04-10 | 24 (32.0) | 34 (32.7) | 31 (35.3) | 21 (29.5) |
| 11-20 | 26 (34.7) | 60 (57.8) | 50 (56.7) | 36 (50.7) |
| 21-30 | 5 (6.6) | 3 (2.9) | 3 (3.3) | 7 (9.8) |
| 31-40 | 0 (0.0) | 0 (0.0) | 0 (0..0) | 2 (2.8) |
| Duration of smoke | ||||
| 01-05 | 18 (23.9) | 10 (9.7) | 10 (11.3) | 5 (7.0) |
| 06-20 | 39 (51.9) | 69 (66.3) | 52 (59.0) | 41 (56.2) |
| 21-50 | 18 (24.0) | 25 (24.1) | 23 (26.0) | 25 (35.1) |
| >50 | 0 (0.0) | 0 (0.0) | 3 (3.3) | 1 (1.4) |
Table 10. Smoking habit.
| Respiratory assessment | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Cough | ||||
| Cough in the morning | 82 (11.1) | 59 (8.6) | 35 (4.9) | 41 (6.5) |
| 3 months of the year | 69 (9.3) | 59 (8.6) | 31 (4.3) | 39 (6.1) |
| For two consecutive years | ||||
| £5 | 46 (56.1) | 28 (47.5) | 17 (48.5) | 16 (39.1) |
| 6-10 | 15 (18.2) | 22 (37.3) | 12 (34.3) | 15 (36.6) |
| >10 | 21 (25.6) | 9 (15.3) | 6 (17.3) | 10 (24.3) |
| Sputum | ||||
| Sputum in the morning | 71 (9.6) | 50 (7.3) | 28 (3.9) | 34 (5.4) |
| 3 months of the year | 64 (8.6) | 49 (7.1) | 25 (3.5) | 1 (0.2) |
| For two consecutive years | ||||
| £5 | 36 (50.7) | 24 (48.0) | 14 (50.0) | 17 (50.0) |
| 6-10 | 15 (21.1) | 19 (38.0) | 10 (35.6) | 10 (14.6) |
| >10 | 20 (28.0) | 7 (14.0) | 4 (14.3) | 7 (20.6) |
| Breathlessness | ||||
| Yes | 79 (10.6) | 29 (4.2) | 24 (3.4) | 13 (2.0) |
| No | 663 (89.4) | 660 (95.8) | 691 (96.6) | 622 (98.0) |
| Wheezing | ||||
| Noisy wheezing | 26 (3.5) | 9 (1.3) | 2 (0.3) | 1 (0.2) |
| Attacks of wheezing | ||||
| 1-3 | 5 (19.2) | 2 (22.2) | 0 (0.0) | 0 (0.0) |
| 4-5 | 12 (46.2) | 6 (66.7) | 1 (50.0) | 1 (100.0) |
| >5 | 9 (34.6) | 1 (11.1) | 1 (50.0) | 0 (0.0) |
| Age of occurrence | ||||
| <5 | 5 (19.2) | 3 (33.3) | 0 (0.0) | 0 (0.0) |
| 5-10 | 5 (19.1) | 2 (22.2) | 0 (0.0) | 0 (0.0) |
| >10 | 16 (60.9) | 4 (44.4) | 2 (100.0) | 1 (100.0) |
| Hemoptysis | ||||
| Coughed blood | 2 (0.3) | 1 (0.1) | 1 (0.1) | 2 (0.3) |
| At what Age | ||||
| <5 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) |
| ³5 | 2 (100.0) | 1 (100.0) | 1 (100.0) | 1 (100.0) |
Table 11. Respiratory assessment.
| Cardiovascular assessment | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=742 | N=689 | N=715 | N=635 | |
| Have you ever had pain in your chest | 61 (8.2) | 44 (6.4) | 27 (3.8) | 29 (4.6) |
| Get this pain when walk up hill or fast | 22 (2.9) | 29 (4.2) | 20 (2.8) | 19 (2.9) |
| Get it when walk at an ordinary pace | 25 (3.4) | 37 (5.4) | 24 (3.4) | 25 (3.9) |
| Stop while you walking | 30 (4.0) | 31 (4.5) | 16 (2.2) | 27 (4.3) |
| Does it go away when you stop | 25 (3.4) | 38 (5.5) | 21 (2.9) | 24 (3.8) |
| How soon does it go away | 9 (1.2) | 27 (3.9) | 15 (2.1) | 15 (2.4) |
| Anywhere else | 15 (2.0) | 4 (0.6) | 4 (0.6) | 1 (0.2) |
| Have you ever had severe pain | 20 (2.7) | 17 (2.5) | 7 (1.0) | 8 (1.3) |
| Have you ever been told that you had high BP | 108 (14.6) | 123 (17.9) | 112 (15.7) | 60 (9.4) |
| Have you started on treatment for high BP | 84 (11.3) | 114 (16.6) | 106 (14.8) | 54 (8.5) |
| Were you ever told that you had heart trouble | 30 (4.0) | 18 (2.6) | 8 (1.1) | 10 (1.6) |
| Did you have stroke | 9 (1.2) | 11 (1.6) | 6 (0.8) | 7 (1.1) |
Table 12. Cardiovascular assessment.
| General health status | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=354 | N=376 | N=385 | N=446 | |
| Rating of child health | ||||
| Excellent | 77 (21.8) | 55 (14.6) | 126 (32.7) | 118 (26.5) |
| Good | 266 (75.1) | 304 (80.9) | 218 (56.6) | 301 (67.5) |
| Fair | 10 (2.8) | 17 (4.5) | 36 (9.4) | 23 (5.2) |
| Poor | 1 (0.3) | 0 (0.0) | 5 (1.3) | 4 (0.9) |
| Was the child premature | 19 (5.4) | 3 (0.8) | 14 (3.6) | 1 (0.2) |
| Did the child stay in the hospital after birth | 153 (43.2) | 186 (49.5) | 173 (44.9) | 181 (40.6) |
| If yes how long | ||||
| 01-05 | 96 (63.2) | 159 (83.7) | 156 (90.7) | 170 (94.9) |
| 06-10 | 44 (29.0) | 24 (12.7) | 15 (8.7) | 7 (4.0) |
| >10 | 12 (7.9) | 7 (3.6) | 1 (0.6) | 2 (1.2) |
| Child missed school due to illness | ||||
| 01-05 | 28 (24.4) | 57 (15.2) | 5 (1.3) | 1 (0.2) |
| 06-10 | 12 (3.4) | 58 (15.4) | 19 (4.9) | 6 (1.3) |
| >10 | 3 (0.9) | 0 (0.0) | 0 (0.0) | 1 (0.2) |
| Doctor ever said that your child missed school because of illness | 8 (2.3) | 3 (0.8) | 12 (3.1) | 4 (0.9) |
Table 13. General health status.
| Respiratory assessment | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=354 | N=376 | N=385 | N=446 | |
| Chest illness before the age of 2 years | 49 (13.8) | 36 (9.6) | 27 (7.0) | 29 (6.5) |
| Child has asthma | 5 (1.4) | 6 (1.6) | 15 (3.9) | 18 (4.0) |
| Doctor seen for this illness | 5 (1.4) | 5 (1.3) | 14 (3.6) | 18 (4.0) |
| Child hospitalized for severe chest illness | 11 (3.1) | 19 (5.1) | 13 (3.4) | 15 (3.4) |
Table 14. Respiratory assessment.
| Cough | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=354 | N=376 | N=385 | N=446 | |
| Cough first thing in the moring | 16 (4.5) | 17 (4.5) | 18 (4.7) | 8 (1.8) |
| Present as much as three month in a year | 10 (2.8) | 12 (3.2) | 18 (4.7) | 8 (1.8) |
| Child cough at other times of the day | 12 (3.4) | 10 (2.7) | 18 (4.7) | 7 (1.6) |
| If yes, this cough present as much as three month in a year | 8 (2.3) | 10 (2.7) | 17 (4.4) | 7 (1.6) |
| Bring up phlegm with cold | 11 (3.1) | 14 (3.7) | 20 (5.2) | 9 (2.0) |
| If yes, has this been present for as much as three months in a year | 9 (2.5) | 11 (2.9) | 20 (5.2) | 8 (1.8) |
Table 15. Child cough.
| Illness in last three months | Industrial area | Commercial area | Residential area | Control area |
|---|---|---|---|---|
| N=354 | N=376 | N=385 | N=446 | |
| Had any illness | 20 (5.6) | 7 (1.9) | 12 (3.1) | 10 (2.2) |
| No. of days unable to do work | ||||
| 0 | 2 (10.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) |
| 01-05 | 8 (40.0) | 3 (42.9) | 4 (33.3) | 3 (30.0) |
| 06-10 | 2 (10.0) | 1 (14.3) | 5 (41.7) | 1 (10.0) |
| >10 | 8 (40.0) | 2 (28.6) | 15 (25.0) | 6 (60.0) |
| Weather seen by a doctor | 20 (5.7) | 6 (1.6) | 12 (3.1) | 9 (1.9) |
| Doctor visits for this problem | ||||
| 01-05 | 12 (60.0) | 5 (83.4) | 10 (83.3) | 6 (66.6) |
| 06-10 | 6 (30.0) | 1 (16.7) | 2 (16.7) | 1 (11.1) |
| >10 | 2 (10.0) | 0 (0.0) | 0 (0.0) | 2 (22.2) |
Table 16. Illness in last three months.
A cross-sectional study was conducted in Ludhiana city of Punjab located in northern India. Air pollution and morbidity data was collected from 2003 to 2004. SPM was measured by Gravimetric method and NOx and SO2 by chemical method. The levels of NOx (19.1 mg/m3) and SOx (26.2 mg/m3) obtained in the study were lower than the levels observed in China (66.6 and 44.7 μg/m3) [20,21]. The classification of the sites into residential, commercial and industrial areas was also not very satisfactory as the SPM levels and other air quality parameters in a commercial area were higher than the levels found in the industrial area. Air Pollution levels of were more than permissible limit in Industrial (814.2-559.2 mg/m3) and residential areas (590.2-290.8 mg/m3) as compared to Non-industrial Town (358.2-239.7 mg/m3). Similarly a study from New Delhi also reported good correlation (personal communication, Rangarajan U) between visibility and RSPM. In this study in adults of industrial, commercial and residential areas symptom of respiratory morbidity i.e. cough (11.1%, 8.6%, 4.9% respectively), sputum (9.6%, 7.3%, 3.9% respectively), breathlessness (10.6%, 4.2%, 3.4% respectively) and wheezing (3.5%, 1.3%, 0.3% respectively) were more as compared to control area i.e. cough (6.5%), sputum (5.4%), breathlessness (2.0%) and wheezing (0.2%). Symptoms of ever had pain in his chest were higher, in industrial area (8.2%) and in commercial (6.4%) as compare to in residential area (3.8%) and control area (4.6%). High BP problem were more in industrial area (14.6%), in commercial (17.9%) and in residential area (15.7%) as compare to control area (9.4%). Symptoms of cough first thing in the morning were more in industrial (4.5%), commercial (4.5%) and residential area (4.7%) as compared to control area (1.8%). Cough present as much as three month in a year, child cough at other times of the day and cough present as much as three month in a year, were more in industrial (2.8%, 3.4%, 2.3% respectively), commercial (3.2%, 2.7%, 2.7% respectively) and residential area (4.7%, 4.7%, 4.4% respectively) as compared to control area (1.8%, 1.6%, 1.6% respectively). Phlegm with cold and as much as three months in a year was more in industrial (3.1%), commercial (3.7%) and residential area (5.2%) as compared to control area (2.0%).
Studies conducted in various parts of the world showed a significant association of RSPM levels and daily mortality (0.5%-2%). Though in this study we could not test the association of RSPM with mortality, but a significant association was observed between SPM, a marker for poor air quality, and different morbidities. There is a need for monitoring of air quality daily at all sites in various Indian cities for making more valid epidemiological conclusions.
We are thankful to WHO and Ministry of Environment and Forest, Govt. of India for providing financial support.t.
Citation: Kumar M. A Health Risk Assessment Study Due to Air Pollution in Industrial Town (Ludhiana) vs. Non-Indusrial Town (Samrala) of Nothren India. Med Rep Case Stud, 2021, 06(6), 227
Received: 08-Oct-2021 Published: 29-Oct-2021, DOI: 10.35248/2572-5130.21.6.227
Copyright: © 2021 Kumar M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO