Case Reports - (2023) Volume 9, Issue 1
Acute Promyelocytic Leukemia (APML) is one of the distinct subtypes of AML with unique pathogenic and morphological features. It usually presents with coagulopathy and is aggressive clinically, therefore, it is imperative to diagnose APML quickly. It has commonly a distinct immunophenotypic profile with negative CD34 and HLADR negative. Here we present a case of APML with positive CD34 and HLADR positive expression and the diagnostic dilemma we faced. Our case reestablishes the importance of morphology and the pitfall in relying on flow cytometry alone without morphology.
Bone marrow, Leukaemia, immunophenotypic
Acute Promyelocytic Leukaemia (APML) is a subtype of acute myeloid leukaemia with distinct pathogenic and morphological features. It is characterized by translocation (15;17) (q22; q21) resulting in PML::RARA transcript which results in impairment in differentiation and expansion of myeloid progenitors leading to predominance of abnormal promyelocytes [1]. APML is associated with coagulopathy due to disease associated thrombocytopenia, disseminated intravascular coagulation and hyper fibrinolysis [2] and can become aggressive if not diagnosed soon. However, with the introduction of ALL-Trans Retinoic Acid (ATRA) and arsenic trioxide, the prognosis has drastically improved with nearly 100% cure [3]. It is therefore imperative to diagnose and treat these cases as soon as possible. The diagnosis of APML is mainly based on morphology and molecular detection however, flow cytometry aids in reaching the diagnosis. Morphologically APML can be of two types- hyper granular and hypo granular (micro granular) [4]. The abnormal promyelocytes (blast equivalents) are large with normal nuclear to cytoplasmic ratio, irregular folded nuclear membrane and moderate amount of cytoplasm containing numerous Auer rods. Faggot cells are also noted. The confirmation of APML diagnosis is by demonstration of fusion of RARA gene located on chromosome 17q21.2 with nuclear regulatory factor gene, PML , 15q 24.1[1]. This translocation is seen in 90%-95% cases of APML [1]. Depending on the position of breakpoint position of PML chromosome; 3 isoforms can be seen [5]. Long isoform (bcr1) present in intron 6 (55%-57%), variant isoform (bcr2) present in exon 6 (3%-5%) and short isoform (bcr3) located in intron 3 (40%). Atypical isoforms involving intron 4, exon 6 and exon 7 can also be identified in occasional cases [6]. RARA translocations always occur at intron 2[7]. These translocations can be detected by either conventional karyotyping or newer methods like RT-PCR or FISH. The flow cytometry classically shows high SSC and FSC with negative CD34 and HLADR [8]. They are commonly CD13, CD33, CD117 and CD64 positive [9]. APML is a rare malignancy in paediatric age group and has a peak incidence at 4th decade [10]. It accounts for only<10% of all paediatric AML [10]. Here we present a paediatric case of APML with positive HLADR and CD34.
A 9-year-old boy presents with complaints of weakness, shortness of breath and petechial spots on lower and upper limb for 3 weeks. On examination, there was mild pallor with no organomegaly or lymphadenopathy. CBC examination revealed leukocytosis. Subsequently bone marrow was done and sent to our referral lab for flow cytometry and cytogenetics by conventional karyotyping. The flow cytometry revealed a population of blasts (CD45 dim to negative) with high side scatter. The blasts were dim positive for CD34, CD117, CD38 and heterogeneous positive for HLADR. These were moderately positive for CD33 and MPO and expressed bright CD13. The blasts were negative for CD19, CD22, CD10, CD3 (cytoplasmic and surface), CD5 and CD7 (Figure 1). On morphology, the smears show ~88% blasts plus abnormal promyelocytes having irregular cleaved nuclear membrane and a granular cytoplasm. Occasional blasts show Auer rods. Faggot cells were not seen (Figure 2). Finally, together with immunohistochemistry and morphology, a provisional diagnosis of micro a distinct granular variant of APML was rendered. A FISH/RT-PCR for PML:RARα was advised. The hybrid transcript for PML::RARA (bcr1) was detected in the leukocytes of the specimen by RT-PCR (Figure 3). Subsequently patient was also screened for coagulopathy and was found to be normal. The patient was also positive for FLT3-ITD mutation. Conventional karyotyping report corroborated with RT-PCR and showed translocation 15;17 (Figure 4). Meanwhile patient was started on ATRA and is currently asymptomatic with normal CBC values. Repeat marrow with quantitative PML::RARA is planned at the end of induction as per ELN guidelines 2019[11].
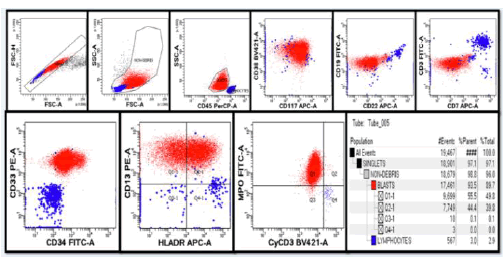
Figure 1: Flow cytometer showing CD34 and HLADR positivepromyelocytes.
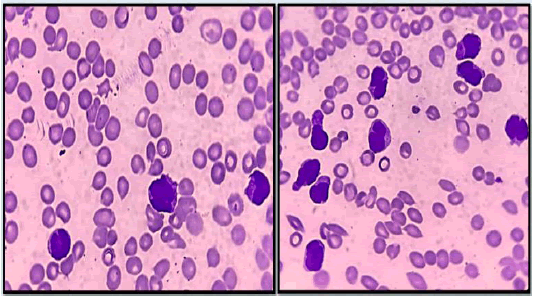
Figure 2: Bone marrow aspirate smears showing abnormal promyelocytes with irregular cleaved nuclear membrane (hypo granular APML)
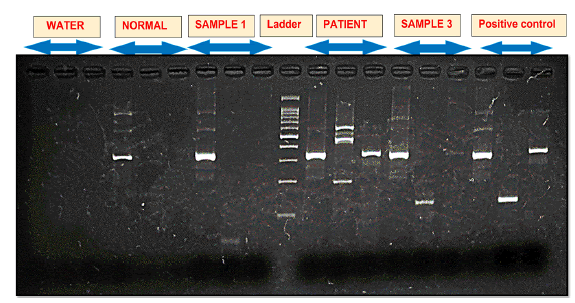
Figure 3: RT-PCR gel showing PML: RARA translocation.
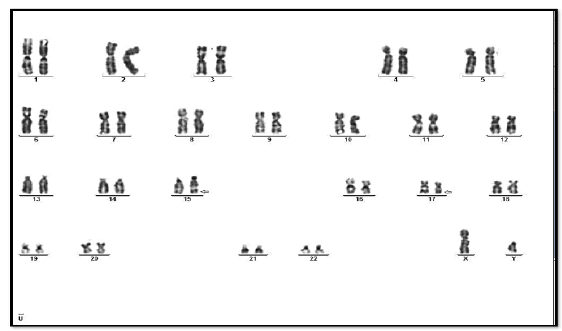
Figure 4: Conventional karyotyping showing characteristic APML translocation- t (15;17).
HLADR and CD34 expression is present on normal myeloblasts however as the maturation progresses it loses its expression from promyelocytes [12]. Therefore, a classical CD34 negative HLADR negative and MPO positive expression in blasts is pathognomonic of APML [8]. The other close differential is AML with NPM1 mutation. The expression of CD33, CD2 CD13 can help in their distinction [13]. But the morphology of the two is very different. Where APML has blobbed/cleaved nuclear membrane with presence of Auer rods and Faggot cells and very bright MPO stain on cytochemistry. AML with NPM1 mutations is generally associated with monocytic morphology and has classical nuclear cupping in>10% of the blasts with a weak MPO staining on cytochemistry [14]. Only few reported cases of HLADR and CD34 positive APML have been reported in the world. Mendoza AS et al has only reported 2 HLADR positive cases out of 45 cases of APML [15]. Few case reports such as Dong et al has reported only 5 positive cases of HLADR expression out of 327 cases where only one case show strong positivity (>20% blasts) [16]. According to that criterion in our case HLADR expression was seen in>40% of the blasts. Kanta Devi et al also reported one case of HLA-DR and CD34 positive APML with>30% blasts showing HLADR positivity [17]. In our case, along with PML:RARα translocation, FLT3 ITD mutation was also detected which is associated with CD2 expression on flow cytometry [18]. The CD34 expression has been reported in the APML rarely and is associated with high WBC count, CD2 expression, micro granular variant, bcr3 isoform and poor prognosis [19]. The presence of FLT3ITD mutation is also associated with poor prognosis [20]. In our case however, it was associated with bcr1 isoform.
With the advancement of science, in the last decade flow cytometry has become an essential tool for defining the lineage of blasts. We have developed a great tendency to rely on immunophenotypic markers for determination of the lineage. However, a case like this brings back the importance of morphology in our mind. Flow cytometry can no doubt aid us in the making of the diagnosis however the final verdict is always made on morphology. In our case, if morphology was not seen, diagnosis of APML would have been missed and patient would have been started on the line of standard AML chemotherapy drugs until the report of conventional karyotyping came which usually comes after 15 days or so. And patient might have been lost. Therefore, it is imperative to remember that APML can sometimes present with CD34 and HLADR expression and should be carefully verified on morphology so that the diagnosis is not missed.
Citation: Kundoo. A, et al. A Bizarre Case of CD34 and HLADR Positive Acute Promyelocytic Leukemia- Battle Between Morphology and Flow cytometry, Oncol Cancer Case Rep. 2023, 9(1), 1-2
Received: 08-Nov-2022, Manuscript No. OCCRS-22-79253; Editor assigned: 09-Nov-2022, Pre QC No. OCCRS-22-79253 (PQ); Reviewed: 16-Nov-2022, QC No. OCCRS-22-79253(Q) ; Revised: 19-Nov-2022, Manuscript No. OCCRS-22-79253 (R); Published: 20-Jan-2023, DOI: 10.35248/23.9.1.1-2
Copyright: ©2023 Kundoo, A. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC-BY, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.