Case Report - (2022) Volume 11, Issue 5
Management of hydrocephalus often involves placement of a Ventriculoperitoneal Shunt (VPS). This device removes fluid from the cerebral ventricles and delivers it to the peritoneal cavity where it can be reabsorbed. Replacement of a failed VPS often requires removing the previously placed system from the head and abdomen prior to placement of new device. Peritoneal adhesions may make removal problematic. This report documents the potential dangers of such adhesions and illustrates the need to beware of such scarring in order to avoid peritoneal cavity injury.
Ventriculoperitoneal shunt • Peritoneal adhesions • Revision
Hydrocephalus is a condition that develops most commonly due to inadequate reabsorption of Cerebrospinal Fluid (CSF) [1]. Subsequent ventriculomegaly (ventricular enlargement) can result in cortical dysfunction secondary to increased intracranial pressure and/or fiber tract (axonal distortion).
A VPS is a device that removes (diverts) fluid from the cerebral ventricles and delivers it to the peritoneal cavity where it can be reabsorbed [2]. The system consists of three elements: ventricular catheter, pressure-based flow regulating valve, and peritoneal catheter. Device malfunction or failure can result from damage to one or more of these components. Abnormal CSF pressure dynamics or mechanical obstruction of shunt tubing are common causes for shunt failure and require shunt replacement/revision in order to reestablish a functioning CSF diversionary device [3]. While complications from shunt replacement are rare, they can arise and may include infection, brain injury and abdominal injury [4].
RA 35-year-old woman presented to the Emergency Department GCS 7 following an unrestrained ejection through the windshield of a motor vehicle involved in a two-car collision. Her past medical history was notable for a previous severe closed head injury as a teenager that required a significant period for recovery to mRS 0. There was no history of prior abdominal surgery. Initial management included emergent right subdural hematoma evacuation, expansion duraplasty and decompressive fronto-temporo-parietal craniectomy with subsequent titanium plate cranioplasty 6 weeks later. Within 10 weeks the patient was GCS 15, mRS 3 yet had developed ventriculomegaly with communicating hydrocephalus. After a trial of lumbar drainage failed to resolve the issue, the patient underwent placement of a left frontal horn Medtronic Strata (Medtronic Corporation, Dublin, Ireland) programmable ventriculoperitoneal shunt. The peritoneal insertion was performed laparoscopically by General Surgery. Even when set at 0.5, this device failed to resolve the patient’s ventriculomegaly. A radionucleotide shuntogram confirmed the shunt’s expected function and patency with normal emptying into the peritoneal cavity and normal distribution. Repeated CSF sampling failed to disclose infection even after being held for 2-3 weeks to rule out indolent Propionibacterium acnes.
A diagnosis of idiopathic high compliance ventriculomegaly (ultra-low-pressure hydrocephalus) was made. The patient returned to the OR 3 weeks after initial shunt placement for revision of the entire system using a low-pressure Strata valve without an inline intrinsic antisiphon device. During this procedure the cranial incision was opened, and the shunt system was removed from the ventricle. The valve was next withdrawn from the patient using traction, yet the peritoneal tubing merely stretched. Despite significant traction force, the peritoneal tubing would not permit itself to be delivered. Suspecting an abdominal adhesion, the General Surgeon was asked to insert the laparoscope and found that the distal end of the peritoneal tubing was firmly adherent to the patient’s appendix at a point where a silk ligature had been placed to secure the tubing to an underlying tube-tube straight connector (Figure 1). Sharp dissection was necessary to separate the distal tubing from the appendix thus permitting device removal. The appendix was not removed Ventriculomegaly ultimately responded to the low-pressure valve sans antisiphon device with extended time spent in an upright position during awake and sleeping periods. The patient returned to her Rehabilitation Center to continue her recovery.
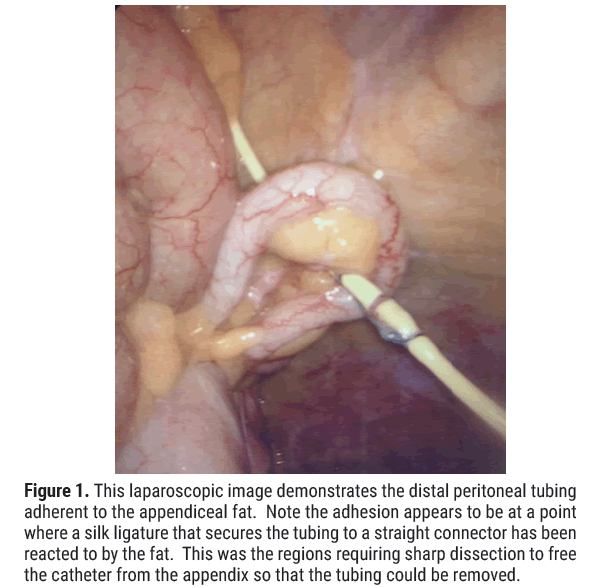
Figure 1: This laparoscopic image demonstrates the distal peritoneal tubing adherent to the appendiceal fat. Note the adhesion appears to be at a point where a silk ligature that secures the tubing to a straight connector has been reacted to by the fat. This was the regions requiring sharp dissection to free the catheter from the appendix so that the tubing could be removed.
Ventriculoperitoneal (VP) shunting remains the treatment of choice for nonobstructive hydrocephalus. This procedure involves a scalp incision and small cranial burr hole and dural-pial opening through which a silastic tube is inserted into the patient’s dilated ventricle. The shunt’s valve is positioned beneath the scalp’s galea and a long tunneling device is used to deliver the distal peritoneal tubing to the abdominal region where it can be inserted into the peritoneal cavity via either an open abdominal incision or using ports and laparoscopic techniques. In 1993, Schievink, et al reported using endoscopy for distal tubing peritoneal insertion [5]. In 2009 this report’s corresponding author (MBH) reported on the latter technique which has become more popular over time as it has proved safe and effective with a reduction in post insertion delayed ventral hernia formation [6].
VP shunt placement is most commonly complicated by infection, tubing blockage, mechanical disconnection or failure, incisional ventral hernia, peritoneal pseudocyst formation (generally secondary to Propionibacterium acnes infection), intestinal perforation, ascites, inguinal hernia, volvulus, organ injury and vascular injury. The above can occur acutely or in a delayed fashion [7]. The incidence of VP shunt associated bowel perforation can approach 1% with mortality rates of up to 15%. Of note, fewer than 30% of such patients present with peritonitis. During revision, total shunt removal may be difficult due to tubing calcifications, adhesion formation, and tubing encasement in a fibrous tunnel. If hardware cannot be safely removed, non-infectious peritoneal tubing can be left within the abdomen [8].
VP shunt revision is generally a simple procedure that can on occasion be complicated by peritoneal adhesions. While hollow organ, solid organ, and vascular injury is a rare sequela of virgin and repeat VP shunt implantation/explantation, mortality can occur if care is not taken. This report, while not illustrating an overly rare event, provides dramatic documentation of how peritoneal tubing can become intimately involved with the large intestine (in this case, appendix) even after only a short intra-peritoneal dwell time. Neurosurgical and General Surgical Residency training programs should continue to reinforce the above, so trainees remain vigilant for this uncommon, yet potentially dangerous event.
JB provided general surgical insights and text for this paper and assisted in the described surgical procedure.
KW provided general surgical insights and text for this paper and assisted in the described surgical procedure.
MH provided neurosurgical insights and text for this paper and assisted in the described surgical procedure.
The authors have no personal or financial conflicts of interest.
This paper is a case report. All identifying information has been excluded from the manuscript.
[Cross ref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
Citation: Bolden J, et al. Ventriculoperitoneal Tubing-Appendiceal Adhesions Laparoscopically Identified During Shunt Removal: The Hidden Dangers in Simple Procedures. J Biol Todays World, 11(5), 001-002
Received: 23-Sep-2022, Manuscript No. jbtw-22-75819; Editor assigned: 26-Sep-2022, Pre QC No. jbtw-22-75819 (PQ); Reviewed: 10-Oct-2022, QC No. jbtw-22-75819 (QC); Revised: 17-Oct-2022, Manuscript No. jbtw-22-75819 (R); Published: 27-Oct-2022, DOI: 10.35248/2322-3308.11.5.005
Copyright: © 2022 Bolden J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.