Research Article - (2023) Volume 12, Issue 3
Objective: Multidrug resistant tuberculosis is currently a significant public health concern. This research aims to determine the prevalence of MDR-TB in patients with tuberculosis infection.
Materials and methods: Data for this retrospective study were collected from the national TB Information System (TBIS) between 2009 and 2019. A total of 989 cases of MDR-TB have been reported and associated risk characteristics have been determined, such as marital status, gender, ethnicity, employment status, consumption of alcohol, diabetic status and smoking status. A multivariate, descriptive and Pearson's chi-square statistical analysis was conducted using SPSS version 20 software.
Results: The incidence of MDR-TB among patients with TB infections in Malaysia was 0.34%. The findings showed major differences in MDR-TB incidence between male and female patients (0.44% vs. 0.20%, p<0.001), single and married patients (1.63% vs. 0.24%, p<0.001), race (p<0.001), working and nonworking patients (0.48% vs. 0.32%, p<0.001), alcoholic and non-alcoholic patients (0.44% vs. 0.32%, p<0.001), diabetic patients and non-diabetic patients (0.39% vs. 0.27%, p<0.001), followed by smoking and non-smoking patients (0.13% vs. 0.27%, p<0.001).
Conclusion: This study provides a significant assessment of the prevalence of MDR-TB and related risk factors that could be useful in Malaysia's national TB strategy.
Multidrug resistant tuberculosis • Prevalence data • Quality of life • Risk factors • TB surveillance and urban health
In 2019 about 600,000 MDR-TB cases were reported worldwide with an estimated 250 million annual deaths. Global TB report has stated that incidents of MDR-TB have continued to rise, potentially threatening to undermine the advances made in TB control. A variation of socio economic and health risk conditions account for the high incidences of MDR-TB worldwide. Multidrug resistant TB is basically an infectious disease caused by inadequate drug sensitive treatment of tuberculosis. In 2018, almost 480,000 new MDR-TB incidents with 100,000 Rifampicin Resistant (RR) incidents were reported worldwide. An approximate 500,000 new Isoniazid Resistant (IR) cases have been reported in 2018, of which 78% were MDR-TB cases. Despite this increase, however, the majority of patients diagnosed in 2017 and 2018 were only one in three or 32% of about 500,000 patients who have developed MDR-TB [1].
MDR-TB is known for its higher medication costs, a longer period of time for therapy and poor effectiveness as compared to other medical conditions. The MDR-TB epidemic is exacerbated by inadequate health education given to TB patients, an increasing number of respiratory infections and other health factors related to this disease. The frequency of MDR-TB cases is projected to increase in 2021 due to the lack of knowledge among TB patients and poor awareness of its contributing factors. In order to develop a comprehensive strategy for health care interventions, a broader understanding of the potential risk factors linked to MDR-TB infection is extremely essential [2].
However, most of MDR-TB related studies investigated were mainly in United States, Europe and Asia region. Hence, it is interesting and important to study on the prevalence of MDR-TB in Malaysia since the numbers of studies done in Malaysia are limited. The purpose of this study is to determine the prevalence of MDR-TB and highlight the relevant health risk factors associated to the development of MDR-TB infection in Malaysia as a tropical country [3].
The occurrence of MDR-TB infection in patients with TB was identified between years 2009 to year 2019. All registered TB patients who have been infected with MDR-TB are retrieved from national TB Information System (TBIS), Malaysia. Socio demographic characteristics such age, gender, ethnicity, marital status and employment, followed by clinical characteristics were recorded into a Microsoft excel data sheet [4].
Malaysian TB information system is a TB patient tracking system in the country that was introduced in 2003. MDR-TB data were collected and reported regularly by these TB clinics or treatment centers throughout the country using a uniform method. Throughout this process, all MDR-TB cases were reported to health department office which has served as a data center for the collection, surveillance, monitoring and recording of all MDR-TB cases in all the states. The data collected will be used to monitor cases involving MDR-TB, not only in treatment facilities but also at a national level. The mechanism of collecting data has helped in evaluating data at a national and global level. Furthermore, the collected data is contributed to the annual reports of the World Health Organization (WHO) [5].
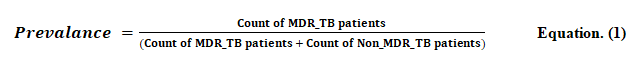
Initial information on TB treatment (TBIS 10A1) forms were used to collect data from individuals with MDR-TB in this study. TBIS 10A1 forms were also used with the intention of enrolling individuals with TB as well as a means to input information into the national TBIS database. Accurate and detailed information regarding the individual with MDR-TB, such as socio demographic, clinical data and initiation of TB therapy were included in the forms. Data obtained from TBIS is used to approximate the prevalence of MDR-TB as well as to identify the possible risk factors among TB patients. The data collected from TBIS were cleaned and converted into an excel spreadsheet. The Statistical Software (SPSS version 20) was used to analyze the data. A 95% confidence interval was used to describe the frequency of MDR-TB. Prevalence is a term used to describe the overall number of incidents in which the disease is transmitted by the population at risk. Cases that were not MDR-TB were selected randomly as control measures and to make comparisons. In order to calculate the prevalence, the following formula or equation (1) was used [6].
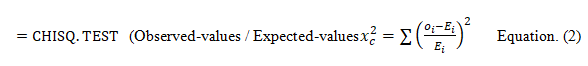
Seven risk factors for MDR-TB infected patients in Malaysia were evaluated: Gender, marital status, ethnicity, employment status, alcohol consumption, diabetic status and smoking status. For each risk factor, Pearson’s chi-square analysis was performed. The analysis involved the following steps:
• Extraction of observed values.
• Formulation of hypothesis.
• Calculation of expected values.
• Calculation of chi-square test significance.
The observed values and expected values were calculated based on equation (2).
To calculate the significance level, p-value, of the Pearson chi-square test, CHISQ.TEST was used [7].
A total of 989 MDR-TB cases were reported to Malaysian national TB surveillance from 2009 to 2019. The MDR-TB cases that were reported during the timeframe included the seven independent risk factors: Gender, marital status, ethnicity, employment status, alcohol consumption, diabetic status and smoking status as shown in Table 1. Meanwhile the total number of TB cases from 2009 to 2019 was 287,092. Similarly, data from TB cases from 2009 to 2019 also included the seven independent risk factors: Gender, marital status, ethnicity, employment status, alcohol consumption, diabetic status and smoking status as shown in Table 2 [8].
| Risk factors/Years | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| MDR-TB | 55 | 64 | 141 | 74 | 124 | 104 | 101 | 74 | 116 | 64 | 72 |
| Male | 37 (67%) | 45 (70%) | 92 (65%) | 57 (77%) | 92 (74%) | 84 (81%) | 82 (81%) | 61 (82%) | 77 (66%) | 51 (80%) | 54 (75%) |
| Female | 18 (32.7%) | 19 (30%) | 49 (35%) | 17 (23%) | 32 (26%) | 20 (19%) | 19 (19%) | 13 (18%) | 33 (28%) | 13 (20%) | 8 (11%) |
| Single | 35 (63.6%) | 26 (41%) | 43 (30%) | 24 (32%) | 46 (37%) | 42 (40%) | 13 (13%) | 25 (34%) | 48 (41%) | 29 (45%) | 26 (36%) |
| Married | 20 (36%) | 38 (59%) | 98 (70%) | 50 (68%) | 78 (63%) | 62 (60%) | 88 (87%) | 49 (66%) | 62 (53%) | 35 (55%) | 46 (64%) |
| Malay | 35 (63.6%) | 45 (70%) | 94 (67%) | 51 (69%) | 88 (70%) | 71 (68%) | 70 (69%) | 52 (70%) | 86 (74%) | 38 (59%) | 55 (76%) |
| Chinese | 5 (90.1%) | 5 (8%) | 7 (5%) | 6 (8%) | 6 (5%) | 5 (5%) | 4 (4%) | 4 (5%) | 5 (4%) | 4 (6%) | 4 (6%) |
| Indian | 11 (20%) | 10 (16%) | 35 (25%) | 13 (18%) | 28 (23%) | 25 (24%) | 24 (24%) | 17 (23%) | 22 (19%) | 21 (33%) | 12 (17%) |
| Others | 4 (7%) | 4 (6%) | 5 (4%) | 4 (5%) | 2 (2%) | 3 (3%) | 3 (3%) | 2 (3%) | 3 (3%) | 1 (1.5%) | 1 (1.4%) |
| Working | 10 (18%) | 12 (19%) | 49 (35%) | 26 (35%) | 35 (28%) | 12 (12%) | 24 (24%) | 16 (22%) | 29 (25%) | 15 (23%) | 11 (15%) |
| Not working | 45 (81%) | 52 (81%) | 92 (65%) | 48 (65%) | 89 (72%) | 92 (88%) | 77 (76%) | 58 (78%) | 87 (75%) | 49 (77%) | 61 (85%) |
| Alcoholic | 8 (14.5%) | 16 (25%) | 37 (26%) | 7 (9%) | 22 (18%) | 29 (28%) | 30 (30%) | 10 (14%) | 30 (26%) | 21 (33%) | 9 (13%) |
| Non-alcoholic | 47 (85%) | 48 (75%) | 104 (74%) | 67 (91%) | 102 (82%) | 75 (72%) | 81 (80%) | 64 (86%) | 78 (67%) | 43 (67%) | 63 (88%) |
| Diabetic | 42 (76%) | 55 (86%) | 72 (51%) | 65 (88%) | 78 (63%) | 52 (50%) | 70 (69%) | 48 (65%) | 77 (66%) | 53 (83%) | 60 (83%) |
| Non-diabetic | 13 (24%) | 9 (14%) | 69 (49%) | 9 (12%) | 46 (37%) | 52 (50%) | 31 (31%) | 26 (35%) | 39 (34%) | 11 (17% | 12 (17%) |
| Non-smoker | 4 (7%) | 2 (3%) | 7 (5%) | 4 (5%) | 5 (4%) | 6 (6%) | 5 (5%) | 3 (41% | 2 (2%) | 3 (5%) | 4 (6%) |
| Smoker | 51 (92.7%) | 62 (97%) | 134 (95%) | 70 (95%) | 119 (96%) | 98 (94%) | 96 (95%) | 71 (96%) | 114 (98%) | 61 (95%) | 68 (94%) |
| Note: ***Total of (MDR-TB) cases from year 2009 to year 2019:989 | |||||||||||
Table 1. MDR-TB cases from year 2009 to 2019.
| Risk factors/Years | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| TB | 25241 | 27450 | 27500 | 29021 | 29221 | 25031 | 24220 | 25240 | 26168 | 24300 | 23700 |
| Male | 15210 (60.29%) | 17720 (64.5%) | 16245 (59%) | 17510 (60.3%) | 16731 (57.2%) | 14500 (58%) | 13100 (54%) | 14620 (58%) | 14084 (54%) | 14150 (58.2%) | 12850 (54%) |
| Female | 10031 (39.74%) | 9730 (35.4%) | 11255 (40.9%) | 11511 (39.6%) | 12490 (42.7%) | 10531 (42%) | 11120 (46%) | 10620 (42%) | 12084 (46%) | 10150 (41.7%) | 10850 (45.8%) |
| Single | 2241 (8.87%) | 1675 (6.1%) | 2408 (8.7%) | 1825 (6.2%) | 2135 (7.3%) | 1772 (7%) | 1670 (6.9%) | 1665 (6.6%) | 1872 (7.2%) | 2438 (10%) | 1782 (7.5%) |
| Married | 23000 (91.1%) | 25775 (93.8%) | 25092 (91.2%) | 27196 (93.7%) | 27086 (92.6%) | 23259 (94%) | 22550 (93%) | 23575 (93%) | 24296 (93%) | 21862 (90%) | 21918 (92.4%) |
| Malay | 14855 (58.8%) | 17135 (62.4%) | 17137 (62.3%) | 17832 (61.4%) | 19601 (67%) | 15670 (62.6%) | 15437 (64%) | 16375 (65%) | 17618 (67%) | 15789 (65%) | 15556 (65.6%) |
| Chinese | 2996 (11.8%) | 3702 (13.4%) | 3501 (12.7%) | 3224 (11.1%) | 3102 (10.6%) | 3017 (12%) | 3275 (14%) | 3070 (12%) | 2972 (11.3%) | 3021 (12.4%) | 2752 (11.6%) |
| Indian | 5870 (23.2%) | 4872 (17.7%) | 5241 (19.0%) | 6423 (22.1%) | 5020 (17.1%) | 4772 (19%) | 4100 (17%) | 4370 (17%) | 4200 (16%) | 4172 (17.2%) | 4090 (17.2%) |
| Others | 1520 (6.02%) | 1741 (6.3%) | 1621 (5.9%) | 1542 (5.3%) | 1498 (5.1%) | 1572 (6.2%) | 1408 (6%) | 1425 (6%) | 1378 (5.3%) | 1318 (5.4%) | 1302 (5.5%) |
| Working | 4527 (17.9%) | 4383 (15.9%) | 4272 (15.5%) | 4307 (14.8%) | 4772 (16.3%) | 4326 (17.2%) | 3966 (16.4%) | 5271 (21%) | 4788 (18.2%) | 4624 (19%) | 4613 (19.4%) |
| Not Working | 20714 (82%) | 23067 (84%) | 23228 (84.4%) | 24714 (85.1%) | 24449 (83.6%) | 20705 (82%) | 20254 (84%) | 19969 (79%) | 21380 (81.7%) | 19676 (81%) | 19087 (80.5%) |
| Alcoholic | 5201 (20.6%) | 3724 (13.5%) | 4672 (16.9%) | 4407 (15.1%) | 4328 (14.8%) | 4269 (17%) | 4432 (18.2%) | 4170 (16%) | 3983 (15.2%) | 4007 (16.5%) | 4002 (16.9%) |
| Non-Alcoholic | 20040 (79.3%) | 23726 (86.4%) | 22828 (83%) | 24614 (84.8%) | 24893 (85%) | 20762 (83%) | 19788 (82%) | 21070 (83.4%) | 22185 (85%) | 20293 (83.5%) | 19698 (83%) |
| Diabetic | 15201 (60.2%) | 17720 (64.5%) | 16358 (59.4%) | 15520 (53.4%) | 15366 (52.5%) | 15201 (61%) | 15179 (63%) | 15073 (60%) | 14788 (56.5%) | 14702 (61%) | 14585 (61.5%) |
| Non-Diabetic | 10040 (39.7%) | 9730 (35.4%) | 11142 (40.5%) | 13501 (46.5%) | 13855 (47.4%) | 9830 (39%) | 9041 (37%) | 10167 (40%) | 11380 (43.4%) | 9598 (39.4%) | 9115 (38.4%) |
| Non-Smoker | 3856 (15.2%) | 2129 (7.7%) | 2277 (8.2%) | 2539 (8.7%) | 2867 (9.8%) | 2729 (11%) | 2614 (11%) | 3729 (15%) | 1484 (5.7%) | 4088 (17%) | 5216 (22%) |
| Smoker | 21385 (84.7%) | 25321 | 25321 (92.2%) | 26482 (91.2%) | 26354 (90%) | 22302 (89%) | 21606 (89%) | 21511 (85%) | 24684 (94.3%) | 20212 (83%) | 18484 (78%) |
| Note: ***Total of TB cases from year 2009 to year 2019: 287,092 | |||||||||||
Table 2. TB cases from year 2009 to 2019.
Based on national TB surveillance data for Malaysian TBIS, the overall estimate of the MDR-TB occurrence among TB infected individuals in Malaysia is determined based on the count, (MDR-TB patients/MDR-TB patient’s count+non-MDR-TB patients count) as shown in Table 3. Overall prevalence of (MDRT-TB/Total TB) from 2009 to 2019 is shown in Figure 1. As for 2011, the cumulative incidence of MDR-TB over total TB was recorded as the highest compared to other years. In 2012 and 2018, MDR-TB incidence dropped drastically. The frequency of MDR-TB among Malaysian TB patients is still relatively low, which is approximately at 0.34% between 2009 and 2019. Independent risk factors, such as socio demographic characteristics, are also linked to MDR-TB occurrence in Malaysia [9].
| Risk factors/Years | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total | P-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDR-TB/Total TB | 0.22% | 0.23% | 0.51% | 0.25% | 0.42% | 0.41% | 0.42% | 0.29% | 0.44% | 0.26% | 0.30% | 0.34% | <0.001 |
| Male | 0.24% | 0.25% | 0.56% | 0.32% | 0.55% | 0.58% | 0.62% | 0.42% | 0.54% | 0.36% | 0.42% | 0.44% | <0.001 |
| Female | 0.18% | 0.19% | 0.43% | 0.15% | 0.26% | 0.19% | 0.17% | 0.12% | 0.27% | 0.36% | 0.07% | 0.20% | |
| Single | 1.54% | 1.53% | 1.75% | 1.30% | 2.11% | 2.32% | 0.77% | 1.48% | 2.50% | 1.18% | 1.44% | 1.63% | <0.001 |
| Married | 0.09% | 0.15% | 0.39% | 0.18% | 0.29% | 0.27% | 0.39% | 0.21% | 0.25% | 0.16% | 0.21% | 0.24% | |
| Malay | 0.24% | 0.26% | 0.55% | 0.29% | 0.45% | 0.45% | 0.45% | 0.32% | 0.49% | 0.24% | 0.35% | 0.37% | <0.001 |
| Chinese | 0.17% | 0.13% | 0.20% | 0.19% | 0.19% | 0.17% | 0.12% | 0.13% | 0.17% | 0.13% | 0.15% | 0.16% | |
| Indian | 0.19% | 0.20% | 0.66% | 0.20% | 0.55% | 0.52% | 0.58% | 0.39% | 0.52% | 0.50% | 0.29% | 0.41% | |
| Others | 0.26% | 0.23% | 0.31% | 0.26% | 0.13% | 0.19% | 0.21% | 0.14% | 0.22% | 0.08% | 0.08% | 0.20% | |
| Working | 0.22% | 0.27% | 1.13% | 0.60% | 0.73% | 0.28% | 0.60% | 0.30% | 0.60% | 0.32% | 0.24% | 0.48% | <0.001 |
| Not working | 0.22% | 0.22% | 0.39% | 0.19% | 0.36% | 0.44% | 0.38% | 0.29% | 0.41% | 0.25% | 0.32% | 0.32% | |
| Alcoholic | 0.15% | 0.43% | 0.79% | 0.16% | 0.51% | 0.67% | 0.45% | 0.24% | 0.75% | 0.52% | 0.22% | 0.44% | <0.001 |
| Non-Alcoholic | 0.23% | 0.20% | 0.45% | 0.27% | 0.41% | 0.36% | 0.41% | 0.30% | 0.35% | 0.21% | 0.32% | 0.32% | |
| Diabetic | 0.28% | 0.31% | 0.44% | 0.42% | 0.51% | 0.34% | 0.46% | 0.32% | 0.52% | 0.36% | 0.41% | 0.39% | <0.001 |
| Non-Diabetic | 0.13% | 0.09% | 0.62% | 0.07% | 0.33% | 0.53% | 0.34% | 0.26% | 0.34% | 0.11% | 0.13% | 0.27% | |
| Non-Smoker | 0.10% | 0.09% | 0.31% | 0.16% | 0.17% | 0.22% | 0.19% | 0.08% | 0.13% | 0.07% | 0.08% | 0.13% | <0.001 |
| Smoker | 0.24% | 0.24% | 0.53% | 0.26% | 0.45% | 0.44% | 0.44% | 0.33% | 0.46% | 0.30% | 0.37% | 0.37% | |
| Note: ***Incidence of (MDR-TB) from year 2009 to 2019: 0.34% | |||||||||||||
Table 3. Overall incidence of MDR-TB cases from 2009 to 2019.
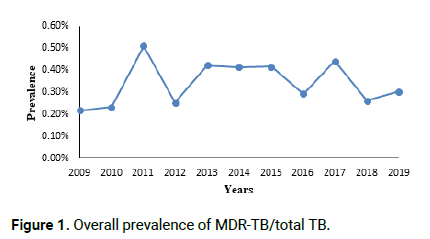
Figure 1: Overall prevalence of MDR-TB/total TB.
Table 4 shows the association of independent factors which have contributed to the incidence of MDR-TB in Malaysia. The frequencies of MDR-TB cases among male patients are 732 (74%) and for female patients are 241 (24.3%). For TB patients the frequencies for male patients are 166,720 (58%) and followed by female patients are 120,372 (42%). The proportion of males in the MDR-TB group is equal to the proportion of females in the MDR-TB group. The frequencies of MDR-TB cases among single patients are 357 (36%) and for married patients are 626 (63%). The crude odds ratio for married patients is (OR: 7.051 p<0.001) and for single patients is (OR: 0.142 p<0.001). For TB patients the frequencies for single patients are 21,483 (7.5%) and followed by married patients are 256,609 (92.5%). The proportion of singles in the MDR-TB group is equal to the proportion of marrieds in the MDR-TB group. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between singles and married patients (1.63% vs. 0.24%, p<0.001) [10].
| Independent risk factors | Number (Prevalence) | P-value |
|---|---|---|
| Gender | ||
| Male | 166,720 (0.44%) | <0.001 |
| Female | 120,372 (0.20%) | |
| Marital status | ||
| Single | 21,483 (1.63%) | <0.001 |
| Married | 256,609 (0.24%) | |
| Ethnic groups | ||
| Malay | 183,008 (0.37%) | <0.001 |
| Chinese | 34,632 (0.16%) | |
| Indian | 53,130 (0.41%) | |
| Other | 16,325 (0.20%) | |
| Working status | ||
| Working | 49,849 (0.48%) | <0.001 |
| Not working | 237,243 (0.32%) | |
| Alcohol consumption | ||
| Alcoholic | 47,195 (0.44%) | <0.001 |
| Non-alcoholic | 239,897 (0.32%) | |
| Diabetic status | ||
| Diabetic | 169,693 (0.39%) | <0.001 |
| Non-diabetic | 117,399 (0.27%) | |
| Smoking status | ||
| Smoking | 253,564 (0.13%) | <0.001 |
| Non-smoking | 33,528 (0.27%) | |
Table 4. Independent risk factors related to MDR-TB prevalence.
The frequencies of MDR-TB cases among Malay patients are 685 (69.2%), Chinese patients are 55 (5.6%), Indian patients are 218 (22%) and others are 32 (3.2%). For TB patients the frequencies for Malay patients are 183,005 (63.7%), Chinese patients are 34,632 (12%), Indian patients are 53,130 (19%) and others are 16,325 (5.7%). The proportion of all ethnic’s groups in the MDR-TB group is equal. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between ethnic’s groups (p<0.001). The frequencies of MDR-TB cases among working patients are 239 (24%) and not working are 750 (75.8%) patients. For TB patients the frequencies for working patients are 49,849 (17.4%) and not working patients are 237,243 (82.6%). The proportion of working patients in the MDR-TB group is equal to the proportion of not working patients in the MDR-TB group. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between working patients and not working patients (0.48% vs. 0.32%, p<0.001). The frequencies of MDR-TB cases among alcoholic patients are 209 (21%) and non-alcoholic are 772 (78%) patients. For TB patients the frequencies for alcoholic patients are 47,195 (16.4%) and non-alcoholic patients are 239,897 (83.5%). The proportion of alcoholic patients in the MDR-TB group is equal to the proportion of non-alcoholic patients in the MDR-TB group. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between alcoholic patients and non-alcoholic patients (0.44% vs. 0.32%, p<0.001) [11].
The frequencies of MDR-TB cases among diabetic patients are 672 (0.67%) and non-diabetic patients are 317 (32%). For TB patients the frequencies for diabetic patients are 169,693 (59.1%) and non-diabetic patients are 117,399 (40.9%). The proportion of diabetic patients in the MDR-TB group is equal to the proportion of non-diabetic patients in the MDR-TB group. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between diabetic patients and non-diabetic patients (0.39% vs. 0.27%, p<0.001).
The frequencies of MDR-TB cases among smoking patients are 944 (95.4%) and non-smoking patients are 45 (4.6%). For TB patients the frequencies for smoking patients are 253,564 (88.3%) and non-smoking patients are 33,528 (11.7%). The proportion of smoking patients in the MDR-TB group is equal to the proportion of non-smoking patients in the MDR-TB group. Pearson’s chi-square indicated that there is a significance difference in the prevalence of MDR-TB between smoking patients and non-smoking patients (0.13% vs. 0.27%, p<0.001).
The association of risk factors with MDR-TB and non MDR-TB patients are shown in (Table 5). The proportion of MDR-TB has been found to be higher in male patients 75.23% (n=732) compared to female patients 24.77% (n=241) with (p-value<0.001). Marital status distribution shows a statistically significant between married and single patients whereby the proportion of married patients are higher 63.68% (n=626) than single patients 36.32 (n=357). The crude OR value shows single patients are higher (7.051 at 95% CI) compared to married patients. The association among different ethnicity groups also to be reported as statically significant (p-value<0.001). The proportion of Malay are higher 69.19% (n=685) compared to Indian 22.02% (n=218), followed by Chinese 5.56% (n=55) and others 3.23% (n=32). Those non-working MDR-TB patients shows higher proportion 75.83% (n=750) than working MDR-TB patients 24.17% (n=239). Similarly, the proportion of non MDR-TB has also found to be higher in male patients 58.07% (n=166,720) compared to female patients 41.93% (n=120,372). Meanwhile the proportion of married non MDR-TB patients 95.52% (n=265,609) is much higher than single non MDR-TB patients 7.48% (n=21,483). Apart from that, the proportion among different ethnicity groups found that Malay patients are to be higher 63.74% (n=183,005) compared to Indian patients 18.51% (n=53,130), followed by Chinese patients 12.06% (n=34,632) and others 5.69% (n=16,325).
| Risk factors | MDR-TB | Non MDR-TB | P-value | Adjusted OR (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Number (%) (n=) | Number (%) (n=) | |||||||
| % | n | % | n | OR | 95% CI | |||
| Gender | ||||||||
| Male | 75.23 | 732 | 58.07 | 166720 | 0.001 | 2.193 | 1.896 | 2.537 |
| Female | 24.77 | 241 | 41.93 | 120372 | Reference | 0.394 | 0.528 | |
| Marital status | ||||||||
| Single | 36.32 | 357 | 7.48 | 21483 | 0.001 | 7.051 | 6.187 | 8.036 |
| Married | 63.68 | 626 | 92.52 | 265609 | Reference | 0.124 | 0.162 | |
| Ethnicity | ||||||||
| Malay | 69.19 | 685 | 63.74 | 183005 | 0.001 | 1.277 | 1.116 | 1.462 |
| Chinese | 5.56 | 55 | 12.06 | 34632 | 0.429 | 0.327 | 0.563 | |
| Indian | 22.02 | 218 | 18.51 | 53130 | 1.243 | 1.07 | 1.446 | |
| Others | 3.23 | 32 | 5.69 | 16325 | Reference | 0.389 | 0.788 | |
| Employment status | ||||||||
| Working | 24.17 | 239 | 17.36 | 49849 | 0.001 | 1.517 | 1.311 | 1.755 |
| Non-working | 75.83 | 750 | 82.64 | 237243 | Reference | 0.570 | 0.763 | |
| Alcoholic | ||||||||
| Yes | 21.3 | 209 | 16.44 | 47195 | 0.001 | 1.376 | 1.181 | 1.604 |
| No | 78.7 | 772 | 83.56 | 239897 | Reference | 0.623 | 0.847 | |
| Diabetic | ||||||||
| Yes | 67.95 | 672 | 59.11 | 169693 | 0.001 | 1.467 | 1.283 | 1.676 |
| No | 32.05 | 317 | 40.89 | 117399 | Reference | 0.596 | 0.779 | |
| Smoking | ||||||||
| Yes | 95.45 | 944 | 50 | 253564 | 0.001 | 2.774 | 2.056 | 3.742 |
| No | 4.55 | 45 | 50 | 253564 | Reference | 0.267 | 0.486 | |
Table 5. Association (adjusted OR) of MDR-TB risk factors.
On multivariate analysis, the regression model showed that male patients (OR 2.193, 95% CI=1.896-2.537) and the married patients showed (OR 7.051, 95% CI=6.187-8.036). Following on the ethnicity groups the Malay patients showed higher (OR 1.277, 95% CI=1.116-1.462), Indian (OR 1.243, 95% CI=1.243), Chinese (OR 0.429 95% CI=0.327-0.563) and others (OR 0.554 95% CI=0.389-0.788). Meanwhile working patients (OR 1.517, 95% CI=1.311-1.755) are more likely associated with MDR-TB infections compare to non-working patients (OR 0.659 95% CI=0.570-0.763). On binary logistic regression analysis, the crude odds ratio (OR) showed that alcoholic (OR 1.376, 95%Confidence Interval (CI) 1.181-1.604). For diabetic patients (OR 1.467, 95% CI=1.283-1.676) and smoking patients (OR 2.774, 95%CI=2.056-3.742) were significantly associated with MDR-TB. All risk factors such as gender, marital status, ethnicity groups, employment status, alcoholic, diabetic and smoking has proven that statistically significant associated with MDR-TB infections with (p<0.001).
In Malaysia, the MDR-TB frequency is low and can be attributed to patients' positive response to first line antibiotics such as isoniazid and rifampicin. According TB patients with isoniazid resistant can be cured at a risk of relapse of less than 5%. Men are at greater risk of being infected with MDR-TB compared to women identified in this study. One potential explanation, according to is that men primarily smoke, drink alcohol and use drugs compared to women. According to younger and single individuals tend to be more vulnerable to MDR-TB due to their high participation in social behaviors which includes alcohol intake and smoking compared to older and married individuals. Evidence from this study indicates that MDR-TB infections between different ethnicities may rely on their behavioral activities. Malay and Indian ethnic groups have a higher incidence of MDR-TB relative to other ethnic groups in Malaysia and this may be attributed to social behavioral factors such as smoking habits, use and abuse of substance and alcohol consumption. Jobless TB infected individuals are more vulnerable to transmission of MDR-TB than those working due to their poverty line, which prevents them from follow up with routine health checks with clinicians in TB centers and purchasing of medicines. A study has revealed that there is a likelihood of a 3.54 fold increase in MDR-TB transmission between alcoholics compared to non-alcoholics, indicating the possibility of disease recurrence. The substantial proportion of MDR-TB multidrug resistant tuberculosis among diabetic patients appears to be growing steadily compared to non-diabetic patients. Smoking is associated with the cessation of TB/MDR-TB treatment and it has been found that this association is independent of alcohol or illicit drug usage.
To date, MDR-TB cases in Malaysia is relatively low (<0.34%) compared to the cases reported globally. In Malaysia, some MDR-TB patients go through heavy financial burdens for their diagnosis and treatments. Multi drug resistance to TB is developed either due to infection with a resistant strain, or as a result of inadequate treatment and poor patient compliance. Hence, proper patient care and commitment to the completion of anti-TB therapy are recommended. The results of the study revealed that all contributing risk factors including age, gender, ethnicity, marital status, smoking, job, diabetic and alcohol intake are associated significantly with MDR-TB prevalence and it is relatively low (<2.0%) in Malaysia. Reliable MDR-TB prevalence estimates will theoretically help to improve prevention measures, guide successful intervention and follow up interventions in vulnerable populations and assist in overall clinical decision making. Inadequate treatment for Tuberculosis (TB) patients and transmission are two main ways for MDR-TB infection and MDR-TB prevalence was higher in persons with previously treated TB patients than that is persons without, proven in many studies. In terms of improving public health related to the condition, development of a national guideline for surveillance and monitoring of MDR-TB and engagement with non-profit organization, civil society and communities for treatment support should be prioritized and strengthened.
The authors would like to acknowledge the University of Malaya (UM), Secretariat of National Institutes of Health (NIHSEC) of Ministry of Health, Malaysia (MOH) and Institute for Respiratory Medicine (IPR) Kuala Lumpur, Malaysia for this study.
The authors extend their profound gratitude to university of Malaysia, institute for respiratory Malaysia, national medical research registry and Malaysian national tuberculosis information system for providing MDR-TB data and for supporting this study. This work did not require informed consent as it was based on data collected from TBIS, Malaysia (NMRR 19-1460-46943).
The authors declare no conflict of interest, financial or otherwise.
The authors would like to acknowledge the University of Malaya (UM), Secretariat of National Institutes of Health (NIHSEC) of Ministry of Health, Malaysia (MOH) and Institute for Respiratory Medicine (IPR) Kuala Lumpur, Malaysia for this study.
National institutes of health and medical research ethics committee. NMRR-19-1460-46943.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Aghamohammadi N, et al., "Prevalence and Associated Risk Factors of Multidrug Resistant Tuberculosis in Malaysia." J Biol Todays World, 2023, 12(3), 1-7.
Received: 02-Nov-2022, Manuscript No. JBTW-22-78847; Editor assigned: 04-Nov-2022, Pre QC No. JBTW-22-78847 (PQ); Reviewed: 18-Nov-2022, QC No. JBTW-22-78847; Revised: 15-Feb-2023, Manuscript No. JBTW-22-78847 (R); Published: 22-Feb-2023, DOI: 10.35248/2322-3308.23.12.3.002
Copyright: © 2023 Aghamohammadi N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.