Research Article - (2023) Volume 5, Issue 3
After tooth extraction, host bone resorption and atrophy of the alveolar ridge are observed. Sutton et al. classified different degrees of alveolar ridge atrophy. Bone resorption occurs especially in the incisors and premolar area of the jaw in the region of thin buccal lamella which may lead to a change in contour. Total clinical bone loss height of approximately 2 mm-5 mm at first 6 months may be observed in a vertical dimension, after 12 months alveolar ridge may lose up to 50% of its width.
Endosseous implants are the treatment of choice for oral and craniofacial reconstruction, serving as transmucosal structures to support single teeth, bridges, complete arch reconstructions, and complete removable dentures or to reconstruct maxillofacial defects. They include a wide spread of sizes shapes surface treatments and prosthetic components with the main objective always being the lifelong success of the osseointegrated interface and uncomplicated function of the prosthetic replacement.
Prosthetic replacement • Maxillofacial defects • Atrophy • Transmucosal structures • Bones
ADDG: Autogenous Demineralized Dentin Graft; AR: Ahmed Reda; ARP: Alveolar Ridge Preservation; ATG: Autogenous Dentin Matrix; AWTG: Autogenous Whole Tooth Graft; CH: Cherine Hamada; DFDBA: Demineralized Freeze Dried Bone Allograft; MS: Mona Shoeib; PES: Pink Esthetic Score; TBG: Tooth Bone Graft
The effect of gap width on bone healing around implants placed into simulated extraction socket defects of varying widths in 10 mongrel dogs is evaluated. All premolars were removed and the alveolar ridges were reduced to a width of 7 mm. Nine weeks later, a total of 80 implants, 10 mm long by 3.3 mm wide, were placed into osteotomy sites prepared to 3 different diameters in the coronal half, simulating extraction sockets.
Recently augmentation with bone grafting became one of the most common techniques surgically; progressive bone resorption may be prevented by using augmentation procedures with the use of graft materials.
The gold standard in regenerative procedures is autogenous bone graft because osteoinduction, osteoconduction, and osseointegration properties are required in regeneration. In an autogenous bone graft, there is a need for a second surgical site, and donor site morbidity and limited availability will lead to challenges for alternative biomaterials.
Different methods of alveolar ridge preservation have been described to prevent this bone atrophy and resorption. Augmentation of extracted sockets with bone is well known and it is the gold standard. Clinical techniques like socket shields were also performed to prevent alveolar bone resorption. Studies have shown osseointegration of implants inserted indicating biocompatibility of autologous tooth material. Applying dentin as a bone substitute for augmentation may be useful to become an alternative to allogenic materials.
Teeth, jaw bones and alveolar bone develop from cells of neural crest origin and many proteins common to dentine, bone, and cementum. Not surprising that previous studies have shown methods of processing bovine dentin into particulate and sterile grafting material for the preservation of alveolar ridge described and tried in animals. Root-canaled teeth should not be employed in this procedure because of contamination with foreign materials. But crown and fillings can be removed and clean dentin of the tooth crown may be used for immediate grafting [1-5].
Extracted healthy non-functional teeth from humans are considered to be dental waste all over the world. A high proportion of extracted sockets are left untreated for physiological healing. Inadequate or failure of bone healing in sockets has been seen due to the absence of bone graft material. The human tooth is rich in stem cells, matrix, trace metal ions, and growth factors. Bone and dentin tissue structures are different but the ratio of components is similar (mineral 70%, collagen 20%, and body fluid 10% by weight). Dentin after demineralization is mainly composed of type 1 collagen 95% and non-collagenous proteins as growth factors.
Dentin composes more than 85% of tooth structure and can serve as native bone grafting material. Teeth become grafts that gradually and slowly being replaced by bone.
Chemically dentin shows a close relationship to bone and shows good osseous regeneration in animals [6].
It is cost-effective because there are no expenses for graft material and also decreases postoperative infection in patients using their tooth structure.
We hypothesized that the purpose of putting dentin chips in the jumping gap between the thin buccal bone and implant placed we asked to determine with the xenograft is Na null hypothesis: regarding soft tissue aesthetic.
Current evidence has a gap of knowledge regarding whether we can use dentin chips not only in socket preservation and delayed implant placement but can we use it with immediate implants or not?
Study design and registration
The current study was designed as a single-blind, randomized, parallel arms-controlled clinical trial, in compliance with the EQUATOR guidelines, with a 1:1 allocation ratio to compare (dentine chips group) to xenograft (control group).
The research protocol was registered on www.clinicaltrials.gov in May 2018 (NCT03544580). Research protocol, informed consent templates, and biological sample collection requests were approved by the research ethics committee, faculty of dentistry, Cairo university, in September 2018 [7-10].
The study was carried out in compliance with the ethical principles of the Helsinki declaration for medical research involving human subjects as revised in Seoul, 2008.
Recruitment of participants
The study was conducted at the faculty of dentistry, Cairo university, Egypt. Participants were recruited from the outpatient clinic, and study procedures were conducted at the postgraduate periodontology clinic at the department of oral medicine and periodontology, faculty of dentistry, Cairo university.
Potential applicants are systemically fit to undergo minor oral surgical procedures free from any systemic diseases or drugs that may contraindicate dental implant therapy.
Non-restorable tooth/teeth in the maxillary aesthetic zone, Thin facial plate of bone (thin<2 mm), Free from any pathology, having a sufficient periapical bone to gain primary stability for the immediate implant.
Smokers, pregnant women, and those with teeth that have to be extracted due to advanced periodontal bone loss, trauma in an aesthetic area, or periapical infection at the site of extraction were excluded [11,12].
Sample size determination
Based on a previous study by Arora and Ivanovski 2017 the difference in PES between 2 groups is 1 ± 0.59.
Using power 80% and 5% significance level we will need to study 7 in each group this number has been increased to a sample size of 8 in each group to adjust for using a nonparametric test. The number is increased again to 10 in each group to compensate for losses during follow-up. Sample size calculation was achieved using PS: Power and sample size calculation software version 3.12.
Randomization
Extraction sites were randomly assigned to undergo a traumatic extraction then either dentin chips with immediate implantation (dentin chips group) or xenograft with immediate implantation (control group) with a 1:1 allocation ratio [13-15].
Sequence generation and concealment were carried out by a single investigator (MS) using www.random.org. Allocation was concealed in serially numbered, identical, and opaque sealed envelopes. AR was responsible for assigning the allocation of participants into the corresponding study group. All participants were enrolled and equally prepared for the surgical procedure by a single investigator (CH). After tooth extraction and grinding, the intervention allocation was revealed (AR) to the investigator (CH) according to the sequence generated.
Blinding
Study participants were blinded to the treatment received. Blinding of the investigator was not applicable. Outcome assessors and biostatisticians were blinded. Participants identity and their corresponding study groups were concealed by assigning an identification number to all data files and reports for the transfer of data to and from assessors [16-18].
Preoperative phase
Following inclusion, the patient’s medical history was documented, teeth of interest were clinically examined, and initial periapical radiographs were taken. Following a detailed explanation of the aim of the study, benefits to participants, surgical procedures, harms, and timeline, participants read and undersigned informed consents.
Professional periodontal debridement was performed, and oral hygiene techniques were explained and emphasized. CBCT scan using on demand 3D is performed to record preoperative ridge width and height measurements and especially crestal bone in the aesthetic area.
Surgical procedures
The main operator (C.H) performed all procedures under local anesthesia (4% articaine with 1/200 000 adrenaline Solution), using a local infiltration technique.
A 1 capsule loading dose of antibiotic 875 mg of amoxicillin and 125 mg of Clavulanic acid tablet (1 g amoxicillin clavulanate) 3 are given orally to the patient 1 hour before the procedure for insuring aseptic condition for the surgery [19-21].
Dentin chips group: Starting with the extraction of a non-restorable tooth a traumatically using a periotome (Figures 1 and 2). Then the root was scraped with a curette to clean it from any periodontal ligament remnants and a bur was used to remove cementum, enamel, and pulp or endo filling (Figure 3).
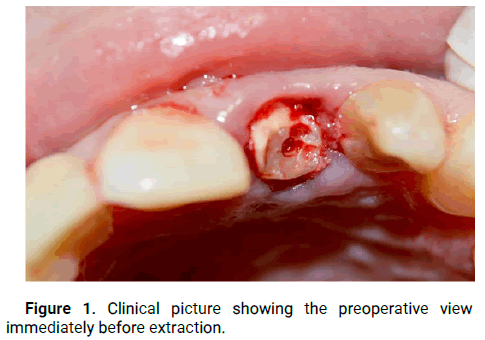
Figure 1: Clinical picture showing the preoperative view immediately before extraction.
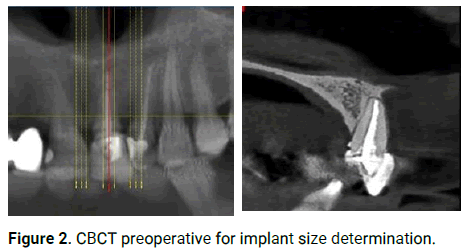
Figure 2: CBCT preoperative for implant size determination.
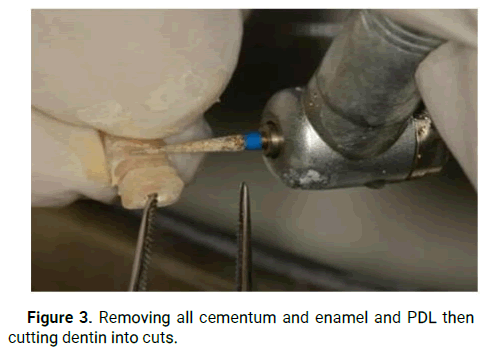
Figure 3: Removing all cementum and enamel and PDL then cutting dentin into cuts.
Followed by dentin was cut into small blocks, and milled in a bone mill to obtain dentin chips used after implant placement.
Dentin particles were immersed in 70% ethanol (El-Gomhouria CO. Egypt) in a sterile container for 10 minutes to remove any soft tissue remnants, bacteria, and smear layer (defatting and sterilization) (Figure 4).
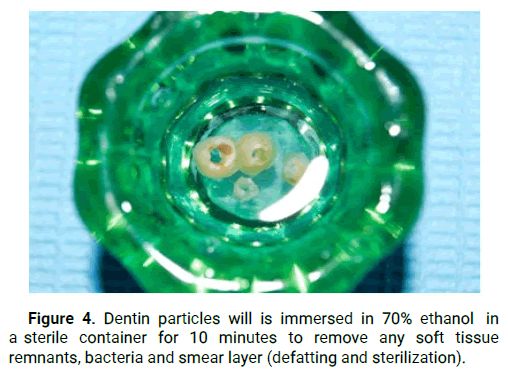
Figure 4: Dentin particles will is immersed in 70% ethanol in a sterile container for 10 minutes to remove any soft tissue remnants, bacteria and smear layer (defatting and sterilization).
Tooth particles were demineralized using 37% HCL (El-Gomhouria CO. Egypt) for 20 minutes to expose the dentin organic matrix (Figure 5).
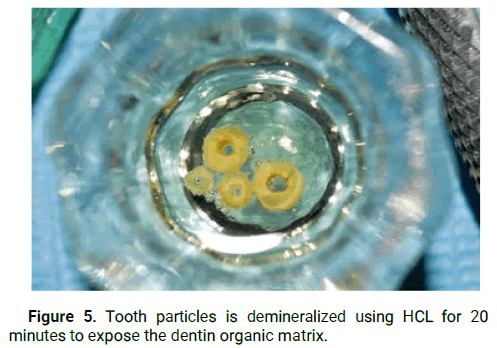
Figure 5: Tooth particles is demineralized using HCL for 20 minutes to expose the dentin organic matrix.
The bacteria free particulate dentin was washed with phosphate buffered saline6 (El-Gomhouria CO. Egypt) twice for 5 minutes to restore the pH balance (Figures 6 and 7).
Figure 6: The bacteria free particulate dentin will be washed with phosphate buffered saline twice for 5 minutes to restore the pH balance.
Figure 7: Cut the dentin into small blocks, milling it in a bone mill to obtain dentin chips used after implant placement.
Then osteotomy site was done using appropriate drill sizes.
A paralleling pin was applied to assure the implant's future position behind the dentin chips and a periapical x-ray was taken (Figure 8).
Figure 8: Dentin chips.
Implant 7 was inserted in place submerged 2 mm under bone crest flapless technique, and also was put the ground dentin chips with the bone mill 8 in the jumping gap and another periapical was then taken. We always used a smaller diameter of the implant to leave a great space for graft (Figure 9).
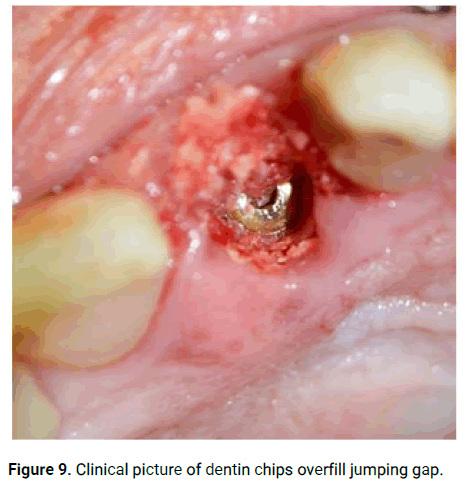
Figure 9: Clinical picture of dentin chips overfill jumping gap.
Control group
Same as the dentin chips group, but we used xenograft (Bio-Oss.) instead of dentin chips in the jumping gap between the implant and buccal bone (Figures 10-17).
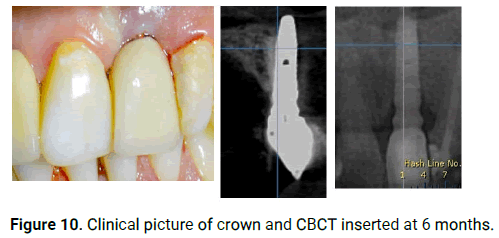
Figure 10: Clinical picture of crown and CBCT inserted at 6 months.
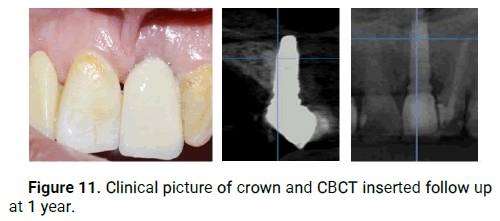
Figure 11: Clinical picture of crown and CBCT inserted follow up at 1 year.
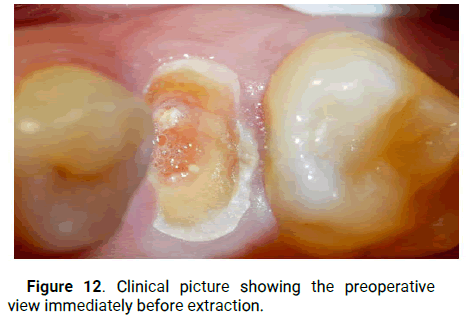
Figure 12: Clinical picture showing the preoperative view immediately before extraction.
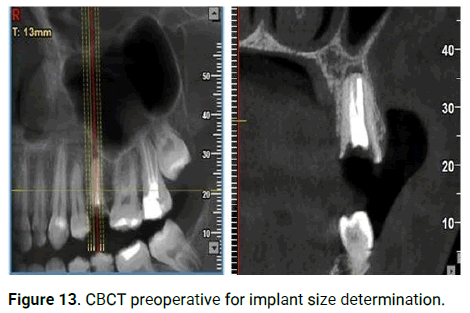
Figure 13: CBCT preoperative for implant size determination.
Figure 14: Xenograft.
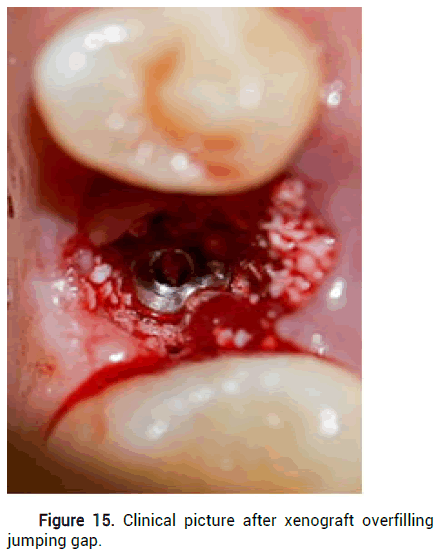
Figure 15: Clinical picture after xenograft overfilling jumping gap.
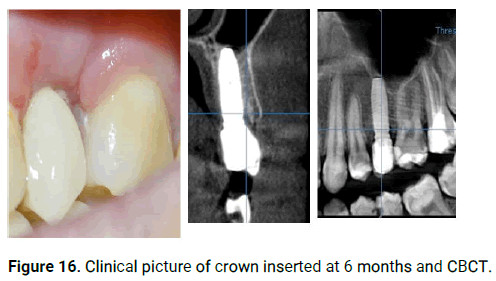
Figure 16: Clinical picture of crown inserted at 6 months and CBCT.
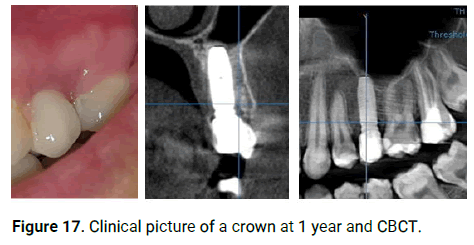
Figure 17: Clinical picture of a crown at 1 year and CBCT.
Postoperative care and follow-up
Post-surgically patients were prescribed cold therapy immediately after the surgery. 1 g amoxicillin clavulanate (875 mg of amoxicillin and 125 mg of clavulanic acid tablet) 10 twice daily for 7 days, anti-inflammatory tablet (50 mg diclofenac) (cataflam 50 mg) 11 three times daily and Povidone Iodine (1%) mouthwash (bBetadine mouthwash) 12 twice daily were prescribed.
Immediately after the surgery standardized radiographic was performed indicating the position of the dentin chips. Again a CBCT was taken after 6 and 12 months to ensure that dentin chips are replaced by bone or not and the amount of buccal bone resorption width gained with the level of crestal bone. Also, pain scales were assessed during such appointments (Figures 18-22).
Appointments were assigned once weekly for the next 2 weeks to assess the pain and swelling and collection of the assessment records at the end of the 2 weeks.
After 6 months we started exposure of implants and prosthetic parts in form of a zirconium crown.
• On demand 3D, Cybermed Inc., Techno Ville, Gasandong,
Geumcheon-gu, Seoul, South Korea.
• Septodont, France.
• Hibiotic 1 gm, Amoun pharmaceuticals, El Obour city, Cairo,
Egypt.
• (El-Gomhouria CO. Egypt).
• Neobiotech USA. Inc., Korea.
• MCTBIO co., Ltd., 46 choburo, Mohyeon-Cheoin-gu,
Yongin-Si, Gyeonggi-do.17037,korea.
• Geistlich Pharma AG Bahnhofstrasse 40 CH-6110 Wolhusen.
• Hibiotic 1 gm, Amoun pharmaceuticals, El Obour city, Cairo,
Egypt.
• Cataflam 50 mg, Novartis pharma S.A.E, El Sawah St., El
Amriya, Cairo, Egypt.
• Betadine mouthwash, El Nile, licensed Mundipharma AG, 41
Farid St., Heliopolis, Cairo, Egypt.
Outcomes
Pink aesthetic score: Was measured using photos preoperatively, 6 months and 1 year as follows
• Mesial papilla.
• Distal papilla.
• The curvature of the facial mucosa and the level of the facial
mucosa.
• Root convexity.
• Soft tissue colour and texture at the facial aspect of the
implant site and a score was given of 2, 1, or 0 is assigned to
each of the five PES parameters with maximum total PES of 10
possible.
Buccal bone resorption, crestal bone
Both are measured on CBCT preoperatively, 6 months and 1 year as follows:
Buccal bone: In the middle of the root before extraction and in the middle of an implant after placement as shown in the picture.
Crestal bone: Is measured from the bone crest to the end of the root before extraction and after extraction from the crest to the end of the implant.
Implant stability: Using osstel.
• Pain: Using a score.
Groups characteristics
Participants were recruited, treated, and followed up between July 2018 and January 2020. All participants in both groups completed the follow-up period and were included in the analysis.
Two failed implants of our patients were observed.
Sixteen participants with single rooted teeth indicated for extraction were randomly allocated into the test (DC with immediate implant) and control group (xenograft with immediate implant) with 8 participants per group.
Reasons for extraction were advanced caries or fracture of teeth beyond restoration.
The dentin chips group included 5 females and 3 males with a mean age of 34.4 years ± 11.3 years, while the control group included 0 males and 8 females with a mean age of 37.1 years ± 7.5 years.
Regarding extracted teeth distribution, the dentin chips group included 8 maxillaries with 6 sites in the anterior teeth segment and 2 in the premolar segment.
For the control group, 6 maxillaries with 0 anterior and 8 premolar extraction sites. There was no statistically significant difference between mean age values in the two groups. Also, no statistically significant difference was found between gender distributions in the two groups (Table 1).
| Time | Intervention (n = 8) | Control (n = 8) | 95% CI for the mean difference | P-value | Effect size (d) | |
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Lower limit | Upper limit | |||
| Pre-operative | 9 (9-9.75) | 10 (9-10) | -1.1 | 0.4 | 0.227 | 0.574 |
| 6 months | 8 (1.75-9) | 8.5 (8-9) | -5.1 | 0.9 | 0.343 | 0.458 |
| 12 months | 8 (2-8) | 8 (8-8.75) | -5 | 0.8 | 0.199 | 0.544 |
| *: Significant at P ≤ 0.05 | ||||||
Table 1: Descriptive statistics and results of Mann-Whitney U test for comparison between PES scores in the two groups.
Pink Esthetic Score (PES)
Comparison between the groups: Pre-operatively, after 6 as well as 12 months; there was no statistically significant difference between PES scores in the two groups (P-value=0.227, Effect size=0.574), (P-value=0.343, Effect size=0.458) and (P-value=0.199, Effect size=0.544) (Table 2).
| Time | Intervention (n=8) | Control (n=8) | 95% CI for the mean difference | P-Value | Effect size | |
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Lower limit | Upper limit | |||
| 6 months | 0.15 (0-0.2) | 0.1 (0-0.19) | -0.08 | 0.14 | 0.546 | 0.292 |
| 12 months | 0 (0-0.08) | 0.05 (0-0.1) | -0.08 | 0.03 | 0.268 | 0.486 |
Table 2: Descriptive statistics and results Hoffmann-Whitney U test for comparison between buccal bone resorption (mm) in the two groups.
Changes within each group: In both groups; there was a statistically significant change in median PES scores by time (P-value=0.010, Effect size=0.581) and (P-value=0.003, Effect size=0.74), respectively. Pair wise comparisons between periods revealed that there was a statistically significant decrease in median PES scores after 6 months followed by a non-statistically significant change from 6 months to 12 months. The median PES score after 12 months showed a statistically significantly lower median score than the pre-operative score (Figure 18).
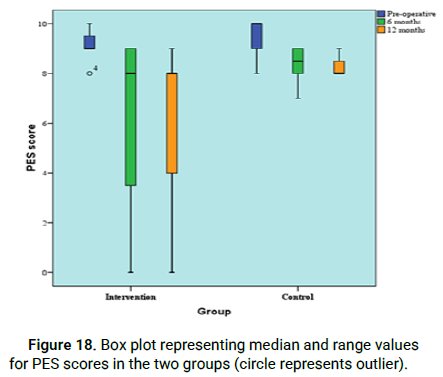
Figure 18: Box plot representing median and range values for PES scores in the two groups (circle represents outlier).
Buccal bone resorption (mm)
Comparison between the groups: After 6 as well as 12 months; there was no statistically significant difference between buccal bone resorption in the two groups (P-value=0.546, effect size=0.292) and (P-value=0.268, effect size=0.486) (Table 3).
| Time | Intervention (n=8) | Control (n=8) | 95% CI for the mean difference | P-Value | Effect size (d) | |
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Lower limit | Upper limit | |||
| 6 months | 0.33 (0.21-0.58) | 0.85 (0.45-1.08) | -0.72 | -0.05 | 0.031* | 1.277 |
| 12 months | 0.1 (0-0.14) | 0.2(0.13-0.39) | -0.33 | 0.04 | 0.029* | 1.277 |
| *: Significant at P ≤ 0.05 | ||||||
Table 3: Descriptive statistics and results of Mann-Whitney U test for comparison between crestal bone loss (mm) in the two groups.
Changes within each group: In both groups; there was no statistically significant change in median buccal bone resorption by time (P-value=0.071, effect size=1.661) and (P-value=0.293, effect size=0.801), respectively (Figure 19).
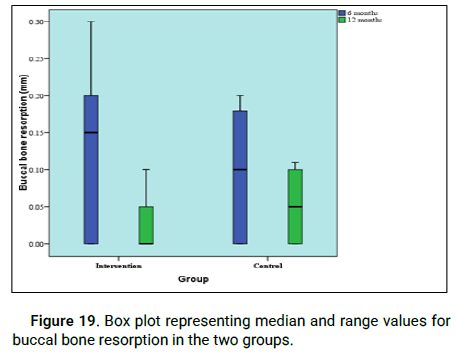
Figure 19: Box plot representing median and range values for buccal bone resorption in the two groups.
Crestal bone loss (mm)
Comparison between the groups: After 6 as well as 12 months; the intervention group showed statistically significantly lower median crestal bone loss than the Han control group (P-value=0.031, effect size=1.277) and (P-value=0.029, effect size=1.277), respectively (Table 4).
| Time | Intervention (n = 8) | Control (n = 8) | 95% CI for the mean difference | P-value | Effect size (Partial eta squared) | |
|---|---|---|---|---|---|---|
| Mean | Mean | Lower limit | Upper limit | |||
| On insertion | 68 | 65 | -12.7 | 6.7 | 0.514 | 0.036 |
| On loading | 74.8 | 70.1 | -15 | 5.6 | 0.34 | 0.076 |
Table 4: Descriptive statistics and results of repeated measures ANOVA test for comparison between implant stability in the two groups.
Changes within each group: In both groups; there was a statistically significant decrease in median crestal bone loss after 12 months (P-value=0.021, effect size=3.955) and (P-value=0.012, effect size=3.932), respectively (Figure 20).
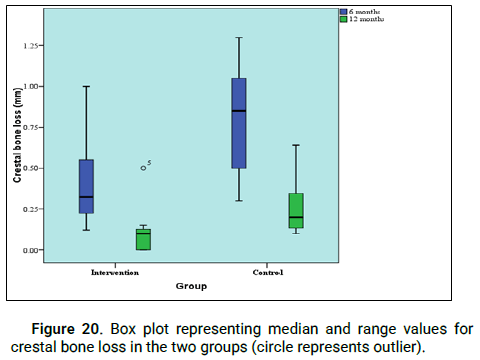
Figure 20: Box plot representing median and range values for crestal bone loss in the two groups (circle represents outlier).
Implant stability
Comparison between the groups: After 6 as well as 12 months; there was no statistically significant difference between mean implant stability values in the two groups (P-value=0.514, effect size=0.036) and (P-value=0.340, effect size=0.076), respectively (Table 5).
| Time | Intervention (n=8) | Control (n=8) | 95% CI for the mean difference | P-value | Effect size (d) | |
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Lower limit | Upper limit | |||
| Day 1 | 8 (7.25-9) | 8.5 (8-9) | -1.3 | 0.6 | 0.436 | 0.374 |
| Day 2 | 7 (6-7.75) | 6.5 (6-7) | -0.6 | 1.3 | 0.436 | 0.374 |
| Day 3 | 5 (5-6) | 5 (5-6) | -0.6 | 0.6 | 1 | 0 |
| Day 4 | 4 (4-5) | 4 (4-5) | -0.8 | 0.8 | 1 | 0 |
| Day 5 | 3 (3-3.75) | 3 (3-3.75) | -0.7 | 1 | 0.903 | 0.053 |
| Day 6 | 1.5 (1-2) | 2.5 (1.25-3) | -2.3 | 0.3 | 0.136 | 0.758 |
| Day 7 | 0 (0-0.75) | 0.5 (0-1) | -1 | 0.3 | 0.268 | 0.486 |
Table 5: Descriptive statistics and results of Mann-Whitney U test for comparison between pain (VAS) scores in the two groups.
Changes within each group: In both groups; there was a statistically significant increase in mean implant stability value on loading (P-value<0.001, effect size=0.893) and (P-value<0.001, effect size=0.862), respectively (Figure 21).
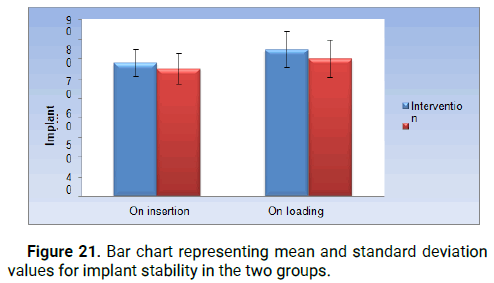
Figure 21: Bar chart representing mean and standard deviation values for implant stability in the two groups.
Pain (VAS) scores
Comparison between the groups: After one day, two, three, four, five, six as well as seven days; there was no statistically significant difference between pain (VAS) scores in the two groups (P-value=0.436, effect size=0.374), (P-value=0.436, effect size=0.374), (P-value=1, effect size=0), (P-value=1, effect size=0), (P-value=0.903, effect size=0.053),(P-value=0.136, effect size=0.758) and (P-value=0.268, effect size=0.486), respectively.
Changes within each group: In the intervention group; there was a statistically significant change in median VAS scores over time (P-value<0.001, Effect size=0.981). Pair-wise comparisons between periods revealed that there was a statistically significant decrease in median VAS scores on day 2, from day 2 to 3, 3 to 4, 4 to 5, 5 to 6 as well as 6 to day 7. In the control group; there was a statistically significant change in median VAS scores over time (P-value<0.001, Effect size=0.942). Pair-wise comparisons between periods revealed that there was a statistically significant decrease in median VAS scores on day 2, from day 2 to 3, 3 to 4 as well as from day 4 to day 5. From day 5 to day 6, there was no statistically significant change in median pain scores followed by a statistically significant decrease in median pain scores on day 7 (Figure 22).
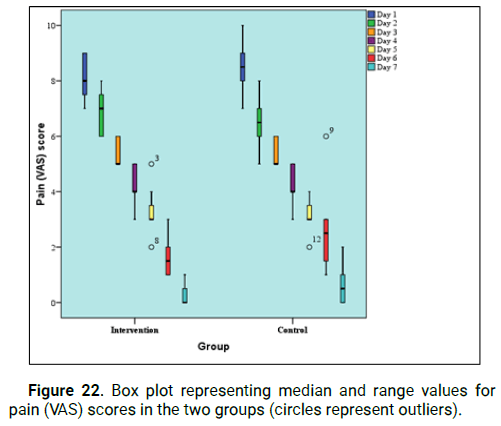
Figure 22: Box plot representing median and range values for pain (VAS) scores in the two groups (circles represent outliers).
Harms
Any temporary or permanent adverse effect will be recorded and documented.
The present study aimed to compare the Autogenous Demineralized Dentin Graft (ADDG) versus xenograft (Bioss) for their effect on PES after 6 months and one year also on buccal bone resorption, crestal bone volumetric changes assessed by 3D cone beam Computed Tomography (CBCT) and Implant stability using osstel.
To minimize confounders, different measures for the selection of participants have been taken in the study. Smokers were excluded because smoking has unfavorable effects on bone healing, not only it adversely affects host cells function and causes alternations to the inflammatory response, but also it reduces the blood supply which leads to a decrease in tissue perfusion and ischemia and turns, negatively affects healing processes following tooth extraction. Clinically, smoking can increase the post-extraction alveolar crest loss by 0.5 mm. Pregnant females were excluded to avoid the teratogenic effect of high radiation exposure when performing CBCT scans.
Some metabolic diseases such as diabetes or hyperthyroidism as well as systemic medications such as chemotherapy or bisphosphonates are further known to affect bone remodeling. Accordingly, patients reporting having any of these conditions were excluded.
Only patients over 18 years were included to provide informed consent and avoid the effect of bone growth and passive eruption of teeth on the quantitative measurements.
In addition to the above mentioned general exclusion criteria, local site specific criteria have been set as well. The exclusion of molars was done because bone quality as well as the size and configuration of molar sockets are different than single-rooted teeth and consequently, healing time and processes are considered dissimilar.
Damaged extraction sockets are generally believed not to be suitable for supporting graft material and require wall replacement by block graft and therefore, such defects were excluded.
Finally, local infection at the site of extraction is known to delay healing, the high acidity is due to inflammation and bacterial byproducts can cause graft particles to dissolve via a cellmediated process or solution-mediated process, and hence no infected site was included.
For the surgical technique used in this study, the flapless approach was chosen since flap elevation is known to cause crestal bone resorption due to the transient deprivation of osteogenic cells and blood supply. In a systematic review it was concluded that leaving the periosteum undisturbed through a flapless approach shows the less alveolar bone height and width resorption in comparison to flap elevation, making it the recommended approach to preserve the bone crest.
When compared to conventional forceps, periotomes required more surgical time but resulted in less buccal bone fracture, less root fracture, less soft tissue laceration, and less postoperative pain.
Hydrochloric Acid (HCL) was used for the preparation of the ADDG as it is one of the strongest demineralizing agents, it has a germicidal effect and at the same time, it does not cause denaturation of collagen fibrils in the dentin matrix, hereby it is the most commonly employed acid in clinical use. The graft particles were immersed in 0.6 N HCl for 30 minutes as recommended by Park, et al. who reported that there was a significant difference concerning graft mineral content and crystalline structure between 10 minutes and 30 minutes of acid application, but there was not any different when increasing the demineralized period beyond that.
The same acid and time application was experimented with in ARP clinically by Um, et al. and showed to be an effective processing technique for ADDG.
Esthetic outcome assessment has been an emerging area of focus in implant dentistry. To sustain an esthetic appearance, it is essential to consider the characteristics of the surrounding soft and hard tissues. Therefore The Pink Esthetic Score (PES) was used to evaluate the esthetic outcomes with the clinical photographs before the treatment and after the follow-up period. The PES includes seven variables (the mesial papilla, the distal papilla, the midfacial level, the midfacial contour, the alveolar process deficiency, the soft tissue color, and the soft tissue texture), and was assessed by using a 0-1-2 score, with 0=lowest score, and 14=highest score.
The PES is a tool for reproducibly evaluating the esthetic appearance of the soft tissue around single tooth implant crowns.
Pink esthetic in our study is statistically non-significant between immediate implants with dentin chips and immediate implants with xenograft in 6 months and 12 months.
But we have an implant that failed after 1 month due to trauma the patient faced in the intervention group and another one failed after 6 months before loading of unknown cause but we have found that asymptomatic endodontically treated teeth with a normal periapical radiographic appearance could be the cause of an implant failure. They also suggested that microorganisms may persist, even though the endodontic treatment is considered radiographically successful, because of inadequate obturation or an incomplete seal.
To our knowledge, there has not been any published comparison between dentin chips and other grafts with immediate implants.
A significant decrease of PES was observed in each group at 6 months and 12 months with no clinical relevance which is inconsistent with who said that the esthetic outcome of soft tissue around the single tooth implant had improved significantly at followup compared with baseline according to PES assessment. As that may be explained by the immediate restoration of immediate implants in his study. His results suggested that the potential for significant changes in soft tissue levels after restorative therapy needs to be considered for single implant therapy in the anterior maxilla.
Crestal bone loss showed statistically significant more bone loss from 0 months-6 months than from 6 months-12 months in the two groups statistically significant bone loss was observed in the control group than in the interventional group which is inconsistent with Showed that implants placed in post-extraction sockets augmented with DFDBA exhibited minimal marginal bone loss similar to implants placed in native bone.
Our results are in contrast to reported that No matter whether using autogenous tooth bone or xenograft, the horizontal bone loss at the first or the latter 6 months was almost the same in the level 0 mm, 3 mm and 6 mm of the implant facial part and no matter what the follow-up period is, and bone graft material used, the horizontal bone loss at the level of 6 mm was much less than the level of 0 mm and 3 mm in the facial of the implant. All implants achieved the success criteria without claiming that grafting of extraction sockets is beneficial in terms of limiting the dimensional changes of the alveolar ridge following tooth/teeth extraction.
In our present study pain (VAS) scores successfully decrease day to day.
A study was conducted in past in implant surgery and found that the female gender was significantly associated with pain, and another study claimed that women had a significantly higher anxiety level than men and that this again led to more pain. Accordingly, in our study, women experienced more pain than men on the second postoperative day. However, other studies found no difference between genders in pain perception. In many experimental studies on pain, though, women reported more severe pain and a longer duration of pain than men.
With all of the advantages of the ATG, it also exhibits limitations. The process of chair side preparation includes cleaning, grinding, and disinfection which require time and effort. As an autogenous graft, it is only available in limited quantity. It requires the extraction of a tooth for graft preparation and hence cannot be used in individuals that do not have any teeth indicated for the extraction or in completely edentulous subjects. A possible solution to this problem can be done by using tooth derived graft materials obtained from allogenic sources but the practice of using allogenic tooth bone graft has been only investigated in a handful of clinical studies with concerns about effective preparation and donor screening for commercial release.
Also, the small sample size, self-funding of research, setting of the study was in a university clinic not like private clinic and we didn’t use a dentin grinder as it’s expensive so we used a bone mill thus further larger RCTs are needed.
AWTG or ADDG employed in ARP is equally effective at reducing dimensional losses after 6 months, with no adverse effects. Histologically, both grafts were biocompatible and osteoconductive, with ADDG seeming to exert higher osteoinductive properties. Chair side preparation and application of ATG are feasible, cost-effective, and can provide an alternative source to commercially available grafting materials.
Said that there is a lack of scientific data related to demineralized dentin and further studies are still needed to validate the performance of demineralize dentin matrix for clinical purposes.
Claimed that more studies have to be done with a large number and a longer follow up, comparing with a gold standard, also to evaluate and understand the real impact of the demineralized tooth graft materials in bone augmentation of oral and maxillofacial procedures.
Clinically and histologically, the dentin graft can act at least in comparison to mostly used xenogeneic or allogenic biomaterials and more studies are necessary to confirm these data.
• The use of autogenous dentin chips proved to be a valid
alternative to bone grafting materials to fill the jumping gap
in conjunction with immediate implants in the aesthetic zone.
• The use of slowly resorbing grafting substitutes as said by Kim,
et al. 2010 simultaneously with immediate implants helped to
preserve the contour of the facial bone plate in the aesthetic
zone.
• Autogenous dentin chips when used with immediate implants
decrease the crestal bone loss more than Bio-Oss®.
• Although the total time for the procedure in the intervention
group was slightly longer than that f or the control group, no
statistical significance existed between both groups regarding
the pain reported by the patients enrolled in each group.
• Regarding the (PES), the overall difference between the control
and the intervention groups showed no statistical significance.
The authors would like to sincerely thank Dr. Abdullah Mattar for his support during the clinical evaluation. This study was selffunded.
All authors explicitly state that they have no conflicts of interest with this article.
No financial support from any sources of institutional, private or corporate support for the work.
The data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
• Cherine Hamada, concept/design, data analysis/interpretation,
drafting article, funding secured by, data collection.
• Ahmed Reda, concept/design, data analysis/interpretation,
critical revision of the article, approval of the article, substantial
contributions to research design analysis or interpretation of
data.
• Mona Shoeib, concept/design, data analysis/interpretation,
critical revision of the article, approval of article, statistics.
Drafting the paper or revising it critically, and approval of
the submitted and final versions.
• All authors have read and agreed to the published version
of the manuscript.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shoeib M, et al. "Pink Esthetic Score with Autogenous Dentin Chips versus Xenograft with Conventional Immediate Implantation in Thin Buccal Bone: Randomized Controlled Clinical Trial". J Dent Res Pract, 2023, 5(3), 1-10.
Received: 08-Jul-2023, Manuscript No. JDRP-23-94842; Editor assigned: 10-Jul-2023, Pre QC No. JDRP-23-94842 (PQ); Reviewed: 24-Jul-2023, QC No. JDRP-23-94842; Revised: 08-Aug-2023, Manuscript No. JDRP-23-94842 (R); Published: 16-Aug-2023, DOI: 10.35248/JDRP.23.5(3).046
Copyright: © 2023 Shoeib M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.