Review Article - (2023) Volume 5, Issue 3
In light of the overwhelming popularity of Self-Contained Underwater Breathing Apparatus (SCUBA) diving, general dental practitioners should be prepared to address complications arising as a result of diving and to provide patients with accurate information. The aim of this article was to introduce the concepts of diving medicine and dentistry to the dentist, and to supply the dental practitioner with some diagnostic tools as well as treatment guidelines. The literature was reviewed to address diving barotrauma (pressure induced injury related to an air space) to the head, face and oral regions, as well as scuba mouthpiece related oral conditions. The relevant conditions for dentists who treat divers include diving associated headache (migraine, tension type headache), barosinusitis and barotitis media (sinus and middle ear barotrauma, respectively), neuropathy, trigeminal (CN V) or facial (CN VII) nerve baroparesis (pressure induced palsy), dental barotrauma (barometric related tooth injury), barodontalgia (barometric related dental pain), mouthpiece associated herpes infection, pharyngeal gag reflex and temporomandibular joint disorder (dysfunction).
Pharyngeal gag reflex • Temporomandibular joint • Neuropathy • Barotrauma • Nerve baroparesis
The massive increase in the popularity of Self-Contained Underwater Breathing Apparatus (SCUBA) diving has put the dentists in a responsible role to diagnose, prevent and treat complications arising from the adverse effect of pressure change on the oral cavity.
All sports carry the risk of accidents and injuries; SCUBA diving is not an exception. The majority of diving injuries can result from the potential toxic effects of the inhaled gas, the mechanical effects from changes in ambient pressure, Decompression Sickness (DCS), equipment malfunction or anatomic characteristics that predispose divers to increased risk of injury [1].
Royal Jordanian medical services/dental department manage a good number of military divers, frog men and is the referral center for most medical cases especially in the southern part of Jordan where the Red Sea shores are the center of amusement for a lot of SCUBA divers both Jordanian and Tourists from around the globe. Baring this in mind, the aim of this article was to draw the attention of health care givers to the concepts of diving medicine and dentistry.
Barotrauma
In order to understand, diagnose and treat maxillofacial complications related to diving a good knowledge about diving medicine and physiology is mandatory [1,2].
Most diving pathologies are due to pressure changes that will cause gas volume change leading to tissue damage or cause pain.
Pressure is defined as the amount of force applied per unit area. Pressure units commonly found in diving include pounds per square inch (psi), kilograms per square centimeters (kg/cm2), atmospheres (atm) and millimeters of mercury (mmHg). Atmospheric pressure is the amount of force or pressure exerted by the earth’s atmosphere. At sea level, it is equal to 14.7 psi, 760 mm Hg, 1.03 kg/cm2 or 1 atm. This becomes the standard 1 atm or absolute pressure (1 ATA) [3].
Because pressure changes in water are linear, ambient pressure increases by 1 atm for each 33 feet of sea water depth (10.23 m) or 34 feet of fresh water depth (10.54 m) [4].
According to the law of Boyle-Mariotte, the pressure of an ideal gas is inversely proportional to the volume, provided that the temperature and the amount of gas are constant.
Most pathology in diving are related to barotrauma or tissue damage resulting from changes in the volume of gas (air) due to the changes in ambient pressure. If pressure rises during the descent of a dive, the volume of the gas declines, the gas volume increases during the ascent of a dive when the pressure decreases. Barotrauma results when divers fail to equalize the pressure in the body’s air containing cavity to outside pressure [5].
Traumas due to pressure (barotraumas) in the orofacial area comprise barotitis media, barosinusitis, pressure induced headache, dental barotraumas and barodontalgia [6].
Barotitis media (also known as middle ear barotrauma) is an acute or chronic traumatic inflammation in the middle ear space do to a pressure differential between the air in the tympanic cavity and the surrounding atmosphere.
Barosinusitis (known as sinus barotrauma or sinus squeeze) is an acute or chronic inflammation of one or more of the paranasal sinuses, produced by the development of a pressure difference between the air in the sinus cavity and that of the surrounding atmosphere [7].
“Sinus squeeze,” often involves the frontal and maxillary sinuses.
Facial nerve injury facial baroparesis has been reported as a complication of middle ear barotrauma. The most accepted hypothesis for facial baroparesis is ischemic neuropraxia. This theory states that excessive middle ear pressure transmitted through a dehiscence of the facial canal decreases the blood flow in the vasa nervorum of the facial nerve. This causes ischemia and consequently neuropraxia.
Referred pain from extra oral facial barotrauma (barotitis media, external otitic barotraumas, and barosinusitis) can be manifested as a toothache and should therefore appear in the differential diagnosis list of barodontalgia [8].
Dental barotrauma is defined as damage to teeth and/or dental restorations (tooth fracture and restoration reduced retention) which can manifest with or without pain when ambient pressure changes. It is assumed that they occur in connection with defective restorations or pathologies such as infections, apical periodontitis, secondary caries and cysts [9-13].
These conditions will need dental treatment but other potential consequences include aspiration or swallowing of the dislodged restoration or dental fragments and pain, this may lead to incapacitation while diving and premature discontinuation of the planned dive [14].
Dental barotrauma usually occurs while ascending; upon surfacing after completing the dive, the diver may report that a tooth broke or has shattered. The explanation could be that during descent, compressed air slowly enters these teeth due to a poor physical seal between the tooth and restoration, but cannot escape quickly enough during ascent. As the diver's depth decreases, there is pressure build up within the tooth due to expansion of the trapped air, leading to severe pain and sometimes even fracture. Displacement of the intra canal medicaments through the root apex has also been reported [15].
In severe cases the pressure build-up in the tooth may lead to explosion of the tooth, called barodontocrexis (barometric induced ‘tooth explosion’) [16].
Pre-existing leaked restoration and occult remaining or recurrent caries lesions underneath restoration are the most reported predisposing factors for dental barotrauma but Gunepin, et al. reported a unique case of fracture of previously intact molar during flight [17].
Fracture of porcelain bonded to metal due to air trapped at the porcelain/metal interface has been reported in divers as well as fracture of teeth undergoing endodontic therapy [18,19].
Atmospheric changes may cause a reduction in crown retention due to negative pressure effects on micro bubbles in dental cements. Lyons and Rodda cycled teeth to 3 atm in a simulated diving experience to study the micro leakage of three different cements (zinc phosphate, glass ionomer and resin cements) and the retention of full cast crowns. Their results suggest that the occurrence of micro leakage and the reduction in the retention of crowns cemented with zinc phosphate and glass ionomer cements after environmental pressure cycling may present clinically as barodontalgia before crown debonding [20].
This may be due to porosities generated during the preparation of zinc phosphate cement and glass ionomer cement, and the expansion and contraction of these micro bubbles upon pressure changes causing weakening of the cement (in approximately 90% and 50% of cases, respectively).
Micro leakage was detected in zinc phosphate and glass ionomer cements after pressure cycling, whereas no micro leakage was detected in the resin cement, probably owing to dentinal tubule obstruction by resin tags or cement flexibility.
Reduced barometric pressure can also impair the retention of full removable dentures (especially maxillary dentures), this has only been observed in flight conditions.
Barodontalgia
Barodontalgia (also known as tooth squeeze) refers to dental pain resulting from environmental pressure changes, it has been reported to occur in aviators from an altitude of 3,000 m (0.75 atm) and in divers at 10 m (1 atm).
It has been described among Self-Contained Underwater Breathing Apparatus (SCUBA) divers since the mid-20th century.
Although rare, in-diving or in-flight barodontalgia has been recognized as a potential cause of diver or aircrew member vertigo and sudden incapacitation, thus it could jeopardize the safety of a dive or flight.
Generally, it has been accepted that posterior teeth are more frequently involved than anterior teeth, maxillary teeth are more frequently involved than mandibular teeth, and restored teeth are more likely to be involved than those that are unrestored.
The etiology of barodontalgia has been investigated for many years; Kollman refers to three important hypotheses to explain this phenomenon:
• Expansion of trapped air bubbles under a root filling or against
dentin that activates nociceptors.
• Stimulation of nociceptors in the maxillary sinuses, with pain
referred to the teeth.
• Stimulation of nerve endings in a chronically inflamed pulp.
He strongly supports the last two hypotheses and states that, for
the latter, histologic evidence show that chronic pulpal
inflammation can still be present even when a thin dentin layer
covers the pulp, for example, as in a deep cavity preparation
(Table 1).
| Direct barodontalgia (owing to pulp disease with or without periradicular involvement) | Indirect barodontalgia | |
|---|---|---|
| Cause | Pulp/periradicular disease. | Barosinusitis, barotitis media. |
| Appearance | During ascent. | During descending pain usually continues on ground. |
| Symptoms | Reversible pulpitis or necrotic pulp: Beating dull pain. Irreversible pulpitis: Sudden sharp penetrating pain. Periradicular periodontitis: Continuous strong pain, swelling. | Toothache in upper premolar/molar region. |
| History | Recent dental treatment. Recent dental sensitivity (e.g. to cold drinks, percussion and/or eating). | Present acute upper respiratory infection, past sinusitis. |
| Clinical findings | Extensive caries lesions or (faulty) restoration. Acute pain upon cold or percussion test. | Pain on sinus palpation, pain upon a sharp change in head position. |
| Radiological findings | Pulpal caries lesions and/or restoration close to pulp horn. Periradicular radiolucency. Inadequate endodontic obturation. | Opacity (fluid) on the maxillary sinus image. |
Table 1. Direct vs. indirect barodontalgia.
Common oral pathologies that have been reported as possible sources of barodontalgia are dental caries, pulpitis, pulp necrosis, defective tooth restoration, apical periodontitis (jawbone cyst and granuloma), periodontal pockets, impacted teeth, and mucous retention cysts.
Pulpitis is the main cause of barodontalgia from the 1940’s to date. Researchers offered several suggestions to explain the mechanism underlying barodontalgia in pulpitis:
• Direct ischemia resulting from inflammation itself.
• Indirect ischemia resulting from intra pulpal increased pressure
as a result of vasodilatation and fluid diffusion to the tissue.
• The result of intra pulpal gas expansion. The gas is a by-product
of acids, bases, and enzymes in the inflamed tissue.
• The result of gas leakage through the vessels because of
reduced gas solubility.
Barodontalgia can be direct (dental and pulpal causes) or indirect (barotitis/barosinusitis-induced).
Facial barotraumas include the entities of external otitic barotrauma, barotitis-media, barosinusitis, barotrauma related headache and dental barotrauma. Referred pain from barotitis and barosinusitis can manifest as toothache, one tenth of the cases of pain in the oral cavity were reported to be caused by barosinusitis, and from here both conditions should appear in the differential diagnosis of barodontalgia.
Ferjentsik and Aker developed a classification of direct barodontalgia and it primarily is based on the underlying causes and clinical symptoms (Table 2).
| Class | Pathology | Features |
|---|---|---|
| I | Irreversible pulpitis | Sharp transient (momentary) pain on ascent |
| II | Reversable pulpitis | Dull throbbing pain on ascent |
| III | Necrotic pulp | Dull throbbing pain on descent |
| IV | Periradicular pathology | Severe persistent pain (on ascent/descent) |
Table 2. Classification of direct (dental induced) barodontalgia.
Temporomandibular Joint (TMJ) Dysfunction (TMD)
The scuba diver gets air from the compressed air tank which reaches the mouth via a regulator with the mouth piece. Diving regulator mouthpieces are typically silicone rubber and are held in place by a bite platform between incisors to premolar occlusion, they have labial flanges for labial seal and an occlusal lug that contacts the lingual side of the teeth to around the first premolar tooth and resists detachment (Figure 1).
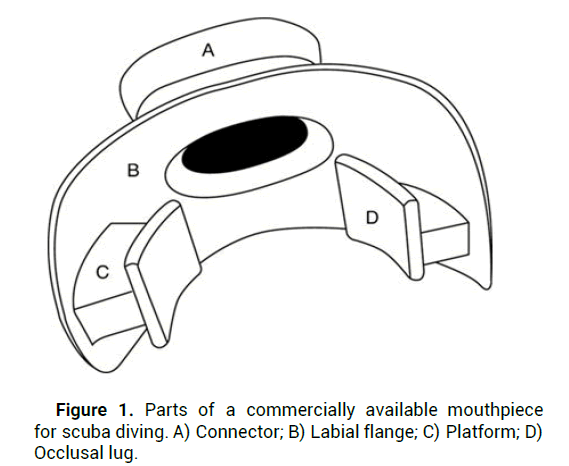
Figure 1: Parts of a commercially available mouthpiece for scuba diving. A) Connector; B) Labial flange; C) Platform; D) Occlusal lug.
In order to keep the regulator in place the mandible is protruded anteriorly leading to uneven loading of the TMJ due to lack of posterior support of the dentition. The regulator with the mouth piece have a significant weight and bulk on the anterior teeth, this with the possibility of gingival and oral mucosa trauma from the mouth piece flanges can cause pain in TMJ and the masticatory musculature [21].
TMD related to diving may manifest as pain and fatigue in the TMJ and muscles of mastication, TMJ crepitus or clicking, headache and tinnitus. These symptoms are known as “divers mouth syndrome” or “regulator mouth” which may involve all or some symptoms of TMD in different degrees and could be limited to diving time or become chronic and constant.
TMD risk factors include female gender and lack of diving experience. The effect of diving in cold or warm water has been discussed as most believe that cold temperature affects the diver’s capability to contract the lips for proper lip seal around the mouth piece and so enforcing over effort on the masticatory muscles for mouth piece stabilization. Bruxism, clenching, stress and poor quality mouth piece are also considered as risk factors for TMD.
There are three mouthpiece designs: Commercial, semicustomized and customized mouthpieces. A semi-customized mouthpiece requires less muscle activity for retention than commercial type while fully customized mouthpieces are reported to cause the least mandibular displacement from the normal resting position, thus usage results in the least discomfort, muscle pain, fatigue (Figure 2).
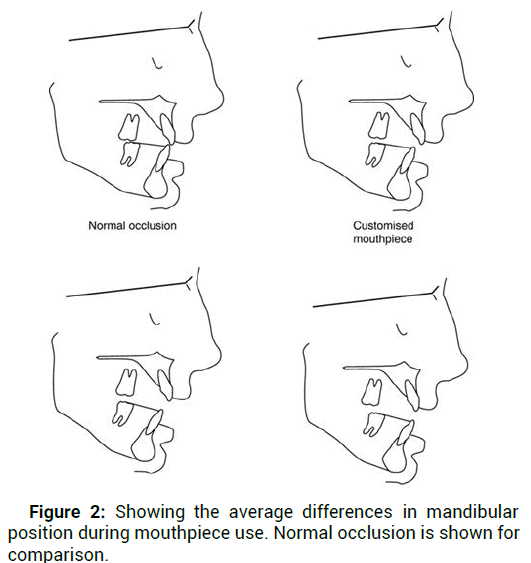
Figure 2: Showing the average differences in mandibular position during mouthpiece use. Normal occlusion is shown for comparison.
Custom mouthpieces are recommended for divers with TMD to optimize underwater occlusal forces. Newton reported that the preferred mouthpiece design should have bite platforms that include the premolar and molar dentition and be at least 4 mm of thickness and suggested that mouthpieces should have extended labial flanges posteriorly to the molars to improve retention and seal and be fabricated to each diver’s normal occlusal relationship, occlusovertical dimension, and freeway space [22].
But Jagger, et al. emphasized the safety aspects of the fabrication of the custom mouthpiece; the mouthpiece must be easily removed and compatible with the mate’s use in emergency (when air sharing by alternate breathing is needed), and the prepared custom mouthpiece should be pretested in a training pool before being used in open water diving.
Other complications related to mouth piece were reported by Robichaud and McNally who suggested that air pushing by mouthpiece into post-surgical wound may induce intraoral pain, mimicking barodontalgia.
Mouthpiece associated pharyngeal (gag) reflex during depth diving when associated with stress can lead the diver to ascend rapidly (panic ascent) a maneuver that may cause Decompression Sickness (DCS).
Diving with fixed orthodontic appliances could be difficult or prohibited using commercial mouthpieces. Jones and Graham described a method for custom mouthpiece fabrication made for a 15 years old trainee diver who lost bonded brackets after attempting to use a normal mouthpiece.
Diving with partial and complete denture is dangerous and can be a hazard when using commercial mouth pieces. Dentures both complete and partial due to their smaller size can become dislodged during a dive and pose an immediate threat for aspiration.
Documented cases of fatal aspiration from a dislodged dental prosthesis during dives was reported by Stein; a recreational diver who, during diving class in a pool, was found at the bottom of the pool and later pronounced dead from asphyxia due to airway obstruction from a maxillary complete denture. Custom mouthpieces can be fabricated to be retained by the edentulous arches so the risk of aspiration of a dislodged prosthesis is eliminated.
Osseo integrated implants because they are solid are not at risk for volumetric expansion or contraction under Boyle’s law and so do not cause any hazard for divers. However, patients with fixed removable prosthesis, such as a header bar retained mandibular complete denture, should follow the guidelines for removable prosthesis because dislodgement is still possible.
Treatment considerations
80% of all diving injuries are head and neck related and approximately 35% of all dive related head and neck complications occur in rhinologic and oral maxillofacial sub sites. Baring this in mind dentists should be aware of the practical recommendations for the prevention and management of such conditions.
Both barosinusitis and barotitis may manifest as barodontalgia and the dental practitioner must rule out an extra oral origin when diagnosing oral pain. This must be taken into consideration especially in higher risk patients (e.g. recent upper respiratory infection or corrected cleft palate with Eustachian tube dysfunction).
Treatment of sinus barotrauma is based on the presenting symptoms. Medical therapy can include saline irrigations, use of decongestants, as well as topical and oral corticosteroids.
Dental barotrauma and barodontalgia treatment aim the underlying source, including removal of dental caries, diseased tooth pulp and dental extractions when needed. Periodic examination can prevent barodontalgia in divers if proper periapical radiographs and vitality test are done with focusing on periapical pathology, secondary caries and faulty restorations. The FDI (Federation Denature International) has recommended an annual examination for scuba divers, sub mariners, air crews and passengers. Panoramic radiographs are recommended for divers and pilots on 3-5 years interval.
When restoring a carious tooth, the dentist should carefully examine the cavity floor to ensure no perforation into the pulp chamber, it’s advised to apply a layer of protective liner.
When teeth require endodontic treatment it’s preferable to inform the diver not to dive until treatment has been completed and patient is asymptomatic for 24 hours post operatively. In a pressure changing environment, open unfilled root canals may cause subcutaneous emphysema and/or leakage of the intracanal infected content to the periradicular tissues.
During surgical treatment for divers and personnel exposed to frequent atmospheric pressure change and especially when dealing with the upper posterior region the dentist must rule out the existence of Oroantral Communication (OAC), which can lead to sinusitis and potentially adverse consequences upon exposure to a pressure changing environment. When OAC is diagnosed, referral to an oral surgeon for its closure is advisable. If OAC is suspected or diagnosed diving should be restricted for at least two weeks. It is preferable to consider all sinus augmentation procedures as a potential for OAC and restrict the diving for longer time than two weeks to prevent augmentation failure and/or pain during diving.
Patients should not dive within 24 hours of a restorative treatment requiring anesthesia and within at least seven days of having surgery. This is to prevent post-surgical forcing of air into the tissues and dry socket. Prior going back to diving the dentist should confirm healing. Temporary diving restriction is also advisable when dentist is in doubt about the prognosis of treatment.
As for diving after major head and neck surgeries it is an individual case by case assessment involving diving medicine and surgical consultation which is essential in such circumstances [23].
Considering all the complications and conditions that could affect SCUBA divers due to the environmental and physiological conditions they face during their dive, it is very obvious that more work and research considering the dental field should be carried out to further explore these complaints. Dentists along with other health care givers are advised to keep the suggested treatment recommendations in mind when planning and treating divers at their clinics.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Ghanam MAA. "Dental Issues and Considerations among Divers". J Dent Res, 2023, 5 (3), 1-5.
Received: 21-Jul-2023, Manuscript No. JDRP-23-92456; Editor assigned: 23-Jul-2023, Pre QC No. JDRP-23-92456 (PQ); Reviewed: 06-Aug-2023, QC No. JDRP-23-92456; Revised: 22-Aug-2023, Manuscript No. JDRP-23-92456 (R); Published: 30-Aug-2023, DOI: 10.35248/JDRP.23.5(3).046
Copyright: © 2023 Ghanam MAA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.