Research Article - (2025) Volume 5, Issue 2
Complete dentures are a common line of treatment for edentulous patients. Many patients suffer from dentures fracture and changes that occur after repairing of the denture, different material and fracture edge profiles have been used for denture repair and to enhance denture accuracy after repair.
Aim: This study aimed to compare the accuracy of two different processed maxillary complete dentures before and after repair with using two different techniques.
Materials and methods: 20 acrylic maxillary complete denture are constructed using long cycle processing (10 denture) and microwave processing technique (10 dentures), dentures were sectioned at the mid-line and repaired using (auto polymerized acrylic resin and fiberglass mesh reinforced for acrylic repair improvement), denture were scanned and saved as STL file, superimposed and measured for adaptation, accuracy was measured, data were collected tabulated and statistically analyzed using paired T-test.
Results: Showed no significant differences using glass fiber reinforced mesh or using only auto polymerized acrylic resin for repair of fractured denture with different processing technique.
Conclusion: Within the limitation of this study, changing the technique of repair or the processing technique of denture base doesn’t affect the accuracy of denture after repair.
Complete denture • Denture repair • Fiberglass • Denture accuracy • T-test
Dentures are usually the first line of treatment of edentulism, Polymethyl Methacrylate (PMMA) is the material of choice for denture fabrication, one of the complications associated with PMMA denture fracture despite its widespread use.
Heat activation for resin polymerization is the conventional method for processing acrylic resin using long or short cycle. Microwave processing have been introduced in 1968, The resin is mixed and exposed to radio waves with a short curing cycle of about 3 minutes at 500 to 600 W/cycle. As the degree of polymerization increases, monomer content decreases proportionally. This technique has some advantages; it is cleaner, denture tooth movements is lower, equal distribution of temperature through the resin and gypsum mold, and increased homogeneity of the dough [1].
The main cause of the removable prosthesis failure is cracking and fracturing of denture bases.4 Denture fractures may occur because of flexural fatigue or impact. Flexural fatigue results due to repeated bending of a material, whereas catastrophic failure or impact failure is one of the mechanical material’s mechanical limitations. Constant stress cycles combined with inadequate denture support results in stress concentration and fatigue failure [2].
Denture acrylic bases fracture occurs in 64% of cases, and 68% of dentures fracture within 3 years after they were provided, midline fracture is commonly seen in the maxillary dentures, the fracture runs through the labial frenulum owing to tensile stress from the masticatory forces.
New denture fabrication is an expensive and time-consuming process. Furthermore, being without prosthesis may be a quite inconvenient for the patient. As a result of this it is common to repair dentures, whether as temporary or permeant [3].
Adequate strength, low cost, simplicity of processing, dimensional accuracy, and color matching with bulk material are all requirements of effective denture base repair material. The denture repair technique should preserve the original strength of the denture, shape of surfaces and prevent further fracture.
Various types of repair material surface patterns and gaps are developed for repair to improve strength and prevent further fracture. Methods for enhancing the strength of the repaired section such as repair surface design, different repair surface treatments, and joint use of autopolymerizing acrylic resin with a wide range of reinforcing materials, such as metal wire and glass fiber have been used [4].
Different edge profiles, such as 45° bevel rounded, butt joint, knife-edge, inverse knife-edge, rabbet, inverse rabbet, lap, joints with mechanical retention, and ogee joints are introduced to improve strength. Furthermore, several materials have been used in the restoration of broken/fractured denture bases, such as visible light polymerized, heat polymerized, autopolymerized, or microwavepolymerized acrylic resin. The edge profile of the repair surface has been proven to influence the fracture strength of the repaired joint. The 45° bevel design increases the interfacial bond area and changes the interfacial stress pattern toward shear stress rather of the more destructive tensile stress.
Denture fracture repair with autopolymerized cure acrylic resins is less expensive, acceptable and less time consuming, although it has certain drawbacks, including weak fracture strength, residual monomer content, and low dimensional accuracies. However, dentures repaired with auto polymerizing acrylic resin alone frequently experience a refracture at the repaired site [5].
Glass Fibers (GF) used as reinforced mesh have a substantial reinforcing impact, and they have several benefits over other fibers, such as less cytotoxicity and higher aesthetics and can bend without fracture. They can be utilized in dental fields for posts, splints, and the reinforcement of fixed dental prostheses. GF has been used as a reinforcing material in many fields.
A well-adapted denture base to supporting tissues is a fundamental objective in the complete denture’s fabrication. Complete denture retention is dependent on excellent denture base adaptation, which may be affected by fracture repair. The processing method, the thickness of the bases, and the form and size of the dentures, as well as the repair processes and materials utilized, may all have an impact on the dimensional correctness and stability of acrylic resin dentures. Because there is insufficient heat present during polymerization to create stress, denture accuracy (DA) is not impacted when applying auto polymerized acrylic resin . Heat-cured repairs, on the other hand, necessitate denture flasking and may deform the denture by releasing tensions during processing [6].
Materials used
A total of 20 complete maxillary dentures were conducted in this study. Stone casts were poured into the study model mold using type III stones (GH dental stone, Egypt). Group (A) Heat cure polymerization acrylic resin was mixed according to the manufacturer’s instructions and processed using a long cycle (hot water bath for 72°C for 6.5 hours.) to produce 10 maxillary denture base (Table 1). And Group (B) 10 microwave processed dentures using kitchen microwave (800 W, Panasonic) for 3 minutes [7].
| Heat cure acrylic resin | PMMA | Acrostone, acrostone Egypt |
|---|---|---|
| Auto-polymerized acrylic | PMMA | Acrostone, acrostone Egypt |
| Fiber bridge mesh (3 mm) | Glass fiber | Sanadent, Romania |
Table 1. Materials used.
All the dentures were finished and polished. Figure 1 dentures were sectioned from the midline using a metal disc. Figures 2 and 3, the gap was widened by 2 mm 20 denture halves were assembled using wax. The dentures were grouped according to the method of repair into 4 subgroups according to method of repair A-1, B-1 autopolymerized acrylic resin and A-2, B-2 reinforcing of the fracture area using glass mesh (Figure 4).
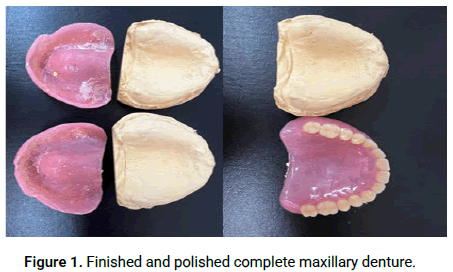
Figure 1: Finished and polished complete maxillary denture.
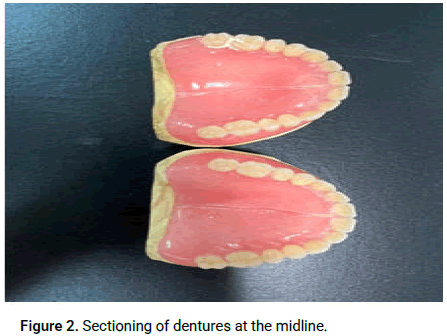
Figure 2: Sectioning of dentures at the midline.
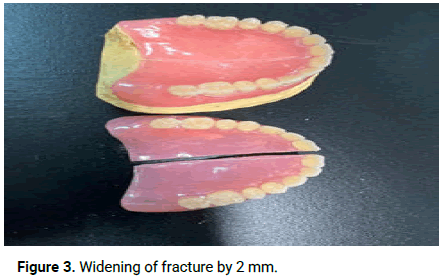
Figure 3: Widening of fracture by 2 mm.
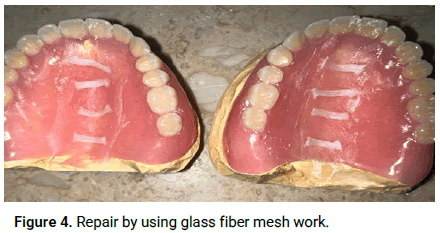
Figure 4: Repair by using glass fiber mesh work.
Superimposition
All denture intaglio surfaces were scanned using a Medit i700 (Medit., South Korea) scanner, which produced an STL file for each intaglio surface (Figure 5). Using surface matching software cast (Geomagic Control X; 3D Systems, Inc) each denture's STL file was superimposed on the STL file of the associated processing (Figure 6) [8].
Measurements were taken at 23 places for each denture, 7 points at the incisive papilla area and 16 along the denture midline color surface maps were developed to visually prove the denture base's adaptation to the cast. Surface matching and measurements were used to assess fit discrepancies along the midline fracture (Figure 7) [9].
Figure 5: Scanning of casts.
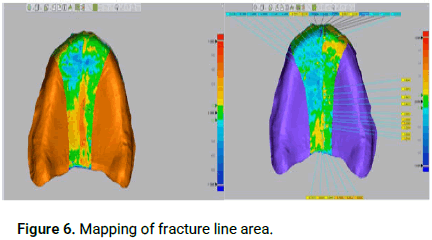
Figure 6: Mapping of fracture line area.
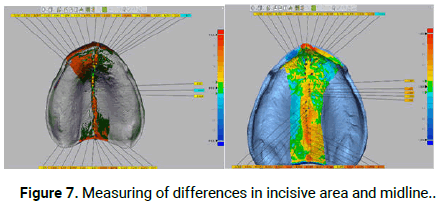
Figure 7: Measuring of differences in incisive area and midline.
Results was tabulated and statistically analyzes using SPSS program version 13, paired T test. mean and standard deviation for the two main groups and subgroups were calculated [10].
Table 2 shows slight difference in adaptation between group (A) with mean adaptation 0.4 at midline and 0.1 at incisal area, group (B) with mean 0.3 at midline and 0.09 at incisal area, but there was a nonsignificant difference at midline (p-value 0.99) and non-significant at incisal area (p-value 0.113) (Figure 8) [11].
| Characteristic | Total | Microwave processed | Heat cure acrylic | p-value |
|---|---|---|---|---|
| (n=20) | (n=10) | (n=10) | ||
| Midline adaptation | 0.3 ± 0.1 | 0.4 ± 0.1 | 0.3 ± 0.1 | 0.099 |
| Mean ± SD | ||||
| Incisional adaptation | 0.1 ± 0.06 | 0.1 ± 0.07 | 0.09 ± 0.04 | 0.113 |
| Mean ± SD |
Table 2. Comparison between two groups.
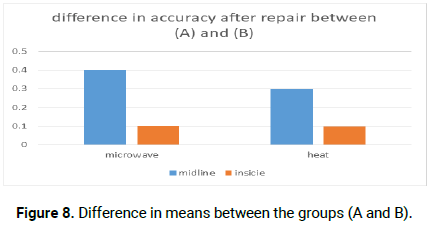
Figure 8: Difference in means between the groups (A and B).
Table 3 shows slight difference in adaptation between sub-group (A-1) with mean adaptation 0.3 at midline and 0.1 at incisal area, group (A-2) with mean 0.4 at midline and 0.1 at incisal area, there was a non-significant difference at midline (p-value 0.057) and nonsignificant at incisal area (p-value 0.687) (Figure 9) [12].
| Characteristic | Total | Glass fiber supported | Auto polymerized acrylic | p-value |
|---|---|---|---|---|
| (n=10) | (n=5) | (n=5) | ||
| Midline adaptation | 0.4 ± 0.1 | 0.3 ± 0.08 | 0.4 ± 0.1 | 0.057 |
| Mean ± SD | ||||
| Incisional adaptation | 0.1 ± 0.07 | 0.1 ± 0.1 | 0.1 ± 0.03 | 0.687 |
| Mean ± SD |
Table 3. Comparison of group acrylic resin.
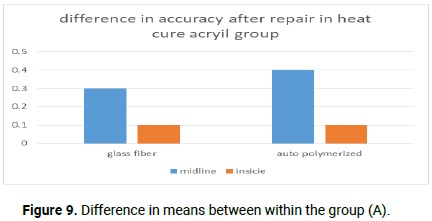
Figure 9: Difference in means between within the group (A).
Table 4 shows slight difference in adaptation between sub-group (B-1) with mean adaptation 0.2 at midline and 0.07 at incisal area, group (B-2) with mean 0.3 at midline and 0.1 at incisal area, there was a non-significant difference at midline (p-value 0.052) and nonsignificant at incisal area (p-value 0.168) (Figure 10) [13].
Subgroup analysis:
| Characteristic | Total | Glass fiber supported | Auto polymerized acrylic | p-value |
|---|---|---|---|---|
| (n=10) | (n=5) | (n=5) | ||
| Midline adaptation | 0.3 ± 0.1 | 0.2 ± 0.1 | 0.3 ± 0.1 | 0.052 |
| Mean ± SD | ||||
| Incisional adaptation | 0.09 ± 0.04 | 0.07 ± 0.05 | 0.1 ± 0.01 | 0.168 |
| Mean ± SD |
Table 4. Comparison of group microwave resin.
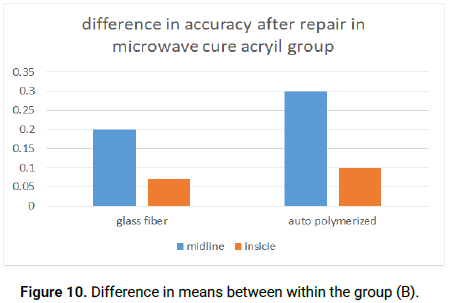
Figure 10: Difference in means between within the group (B).
Denture fractures are a genuine problem for patients and dentists, and denture repair procedures must address this issue. Numerous researches have been conducted to explore the influence of various repair materials and techniques on flexural strength, but few studies have investigated the accuracy of fitting surfaces following denture repair. Poly-Methyl Methacrylate (PMMA) is the most often used material for repairing partial and complete dentures, none the less this material has certain restrictions [14-17].
This research aimed to compare denture accuracy before and after repair with different techniques (autopolymerized acrylic resin and reinforcement glass fiber autopolymerized acrylic resin) in two different processed techniques denture bases, there was no significant difference in using auto polymerized acrylic resin and GF mesh in repair of heat cure acrylic resin or microwave cured acrylic resin.
This is consistent with research that used repairing dentures with an auto polymerized material supplied superior denture accuracy. The low heat generated by the auto polymerizing most likely prevented residual tension from being released the denture base material, thereby decreasing denture distortion. Superior adaptation was obtained using the auto polymerizing repair method, which was superior in adaptation to the other methods and did not differ from each other.
Other studies have reported that using self-cured resins for repair can be conducted faster because no denture flasking is required. furthermore, the denture accuracy is maintained because during polymerization, insufficient heat is present to release stress. Flasking of denture is required if heat cure acrylic resin is used for repair and may distort the denture by releasing stress during processing. Repair purpose is to obtain at least equal or greater transverse strength than the original material [18].
Additionally, utilizing a small size gap for preparation had less effect dimensionally on dentures in this study, which corresponds with the study that stated that the size of the gap between the two cracked segments should be 3 mm or less to minimize the bulk of repair material used. The lower the bulk of the repair material, the less polymerization shrinkage there will be.
Accordng to Sadamori, et al., and Rached, et al., suggested that the processing technique, thickness of the bases, and form and size of the dentures can all affect the dimensional correctness and stability of acrylic resin dentures [19,20].
Similar observations have been reported in cases where the resin for denture bases exhibits contractions and expansions in different locations, similar findings, where the resin for denture bases can show contractions and the use of a glass fiber reinforced autopolymerizing resin with a 45°bevel joint design of the damaged surfaces and surface preparation was shown to minimize stress concentration.
Keyf and Uzun observed that reinforcing the self-cure with glass fiber notably increased its resistance to crack propagation and did not affect the adaptation of the denture base.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mohamed SZ, et al. "Accuracy of Repaired Maxillary Dentures with Different Repairing Techniques In vitro Comparative Study". J Gen Dent, 2025, 5(2), 1-5.
Received: 13-Feb-2023, Manuscript No. JGD-23-89323; Editor assigned: 15-Feb-2023, Pre QC No. JGD-23-89323 (PQ); Reviewed: 01-Mar-2023, QC No. JGD-23-89323; Revised: 06-Jan-2025, Manuscript No. JGD-23-89323 (R); Published: 13-Mar-2025, DOI: 10.4172/jgd.25.5(2).037
Copyright: © 2025 Mohamed SZ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.